HPA Axis Suppression: What It Is, Why It Matters, and How Medications Cause It
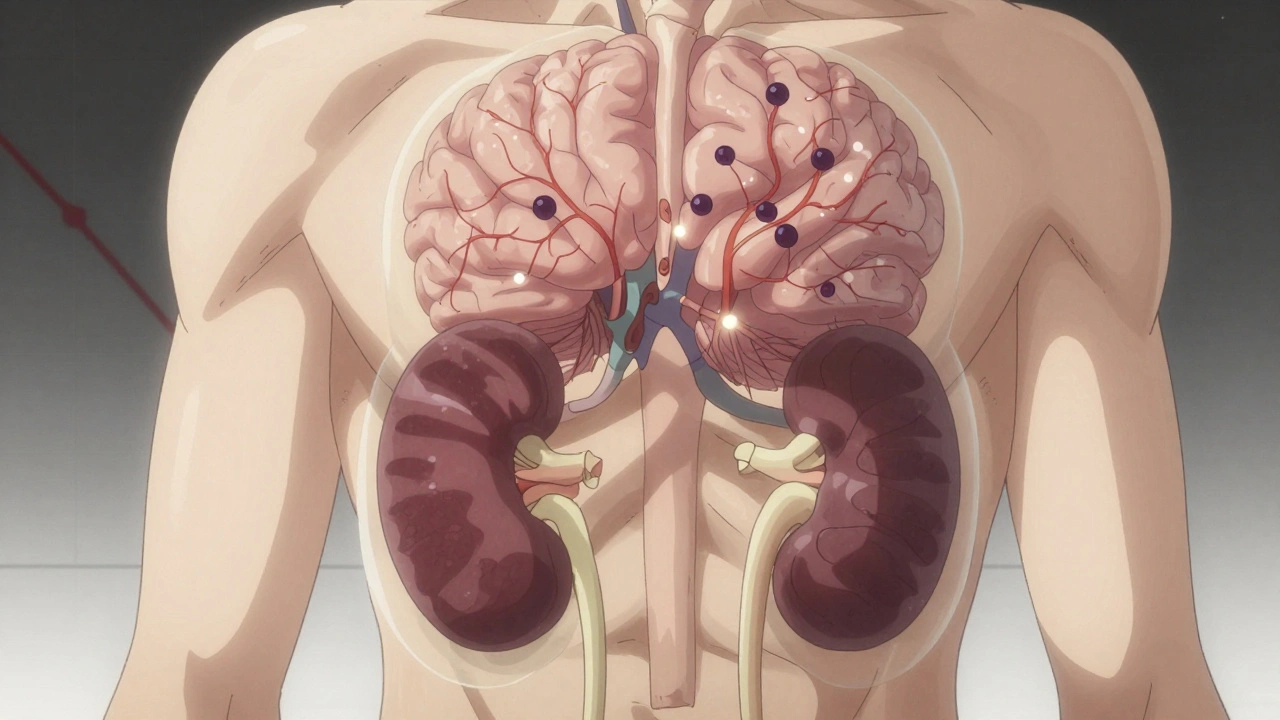
When your body is under stress, the HPA axis, the hypothalamic-pituitary-adrenal axis, is your body’s built-in stress response system. Also known as the stress hormone pathway, it controls cortisol production—the key hormone that helps you wake up, handle pressure, and recover from illness. But when you take certain medications for weeks or months, this system can shut down. That’s called HPA axis suppression. It’s not a side effect you can ignore. It’s a physiological reset that leaves you vulnerable to fatigue, low blood pressure, and even life-threatening crashes if you stop the drug too fast.
Corticosteroids, like prednisone and dexamethasone, are the most common cause of HPA axis suppression. They mimic cortisol so well that your brain thinks you’re already producing enough—and stops signaling your adrenal glands to make more. Over time, those glands shrink from disuse. Even anti-inflammatory drugs used for autoimmune conditions can trigger this. But it’s not just steroids. Some antidepressants, especially long-term SSRIs, and even certain cancer drugs can interfere with cortisol rhythm. And if you’ve ever been told to "taper slowly" after a course of pills, that’s because of HPA axis suppression. Your body doesn’t forget how to make cortisol overnight. It needs time to wake up again. Jumping off these meds cold turkey can cause adrenal crisis—nausea, dizziness, low blood sugar, and in severe cases, shock. That’s why doctors don’t just prescribe these drugs lightly.
What makes HPA axis suppression tricky is that you might feel fine while taking the medication. The problem shows up when you try to stop—or when you get sick, injured, or stressed. Your body has no reserve. No backup cortisol. No emergency response. That’s why people on long-term steroids carry medical alert cards. That’s why some patients need supplemental cortisol during surgery or infection. It’s not about being weak. It’s about biology.
The posts below show how this plays out in real life: from how prednisone affects autoimmune patients to why switching antidepressants can trigger adrenal fatigue, and how doctors miss the signs because symptoms look like burnout or depression. You’ll find practical advice on spotting early warning signs, managing tapering schedules, and protecting your adrenal health without giving up necessary treatment. This isn’t theoretical. It’s something that happens to real people—and you need to know how to protect yourself.
Opioids and Adrenal Insufficiency: A Rare but Life-Threatening Side Effect You Need to Know
Opioid-induced adrenal insufficiency is a rare but life-threatening side effect of long-term opioid use. It suppresses cortisol production, leaving patients vulnerable to crisis during stress. Early testing can save lives.
Continue Reading



