When a patient picks up a prescription and sees a pill that looks completely different from what they’re used to, it’s not unusual for them to pause. Generic medications are just as effective as brand-name drugs, but many patients don’t believe it. In fact, nearly 1 in 4 patients express concern about switching to generics, according to a 2021 study in the Journal of the American Pharmacists Association. The problem isn’t that generics don’t work-it’s that patients don’t understand how they work. And too often, the way we talk about them makes things worse.
Why Patients Doubt Generics
It starts with appearance. A patient who’s taken a blue oval pill for years might panic when they get a white rectangle instead. That’s not a mistake-it’s standard. Generic manufacturers aren’t allowed to copy the exact look of brand-name drugs. But without context, patients assume it’s a different medicine, or worse, a lower-quality one. A University of Michigan study found that 78% of patients base their trust on how the pill looks, not what’s inside. Then there’s misinformation. Many believe generics contain only 80% of the active ingredient. That’s false. The FDA requires generics to deliver 80-125% of the same active ingredient as the brand. That’s not a range of quality-it’s a range of absorption. Think of it like two different brands of aspirin: one dissolves faster, one slower. Both work. Both are safe. And then there’s cost. When a pharmacist says, “This is cheaper,” it sounds like a compromise. Patients hear: “This is the budget version.” A 2021 study in the Journal of General Internal Medicine showed that framing generics as “cheaper” only increased acceptance by 7%. But when pharmacists said, “This contains exactly the same active ingredient but without the brand name marketing costs,” acceptance jumped 29%.What Actually Works: The Science of Trust
The most effective conversations don’t start with facts. They start with listening. The Ask-Tell-Ask method is backed by real data. First, ask: “What do you know about this medication?” Then, tell: “Here’s what’s actually in it.” Then, ask again: “Can you tell me in your own words why this is safe?” This isn’t just polite-it’s proven. A 2020 study of over 1,200 patients found that using this method led to 68% acceptance of generics, compared to just 42% with standard advice. Even more powerful? Personal endorsement. When a pharmacist says, “I prescribe this for my own family,” acceptance rises by 37 percentage points. Why? Because trust isn’t built on data sheets. It’s built on shared humanity. Patients don’t need a lecture. They need to know you’re on their side. The VALUE framework-Validate, Acknowledge, Listen, Understand, Educate-works better than any script. A 2023 review of 12 communication methods found that pharmacists using this approach achieved 76% success in getting patients to accept generics. That’s 18 points higher than standard counseling. And timing matters. If you wait until the patient is at the counter to explain, you’re already behind. The FDA’s 2022 report found that 89% of patients who heard about generic substitution at the time of prescribing accepted it. Only 63% did when they learned about it at the pharmacy. Prescribers and pharmacists need to work as a team. When both explain the switch, acceptance jumps to 85%.What Doesn’t Work
Dismissive language kills trust. Saying “It’s the same drug, just cheaper” doesn’t reassure-it alienates. One patient on Reddit shared: “When my pill changed shape, I thought I was being given a knockoff. I didn’t take it for three days.” That’s not an outlier. It’s common. Overemphasizing cost backfires. A 2021 JAMA Internal Medicine study showed that when cost was the only reason given, trust dropped by 22%. Patients start to wonder: “If it’s so good, why are they pushing it so hard?” And rushing through the conversation? That’s worse than silence. A 2020 study found that primary care doctors average just 18 seconds before interrupting patients who raise concerns about medication. That’s not counseling. That’s dismissal.
Tools That Help
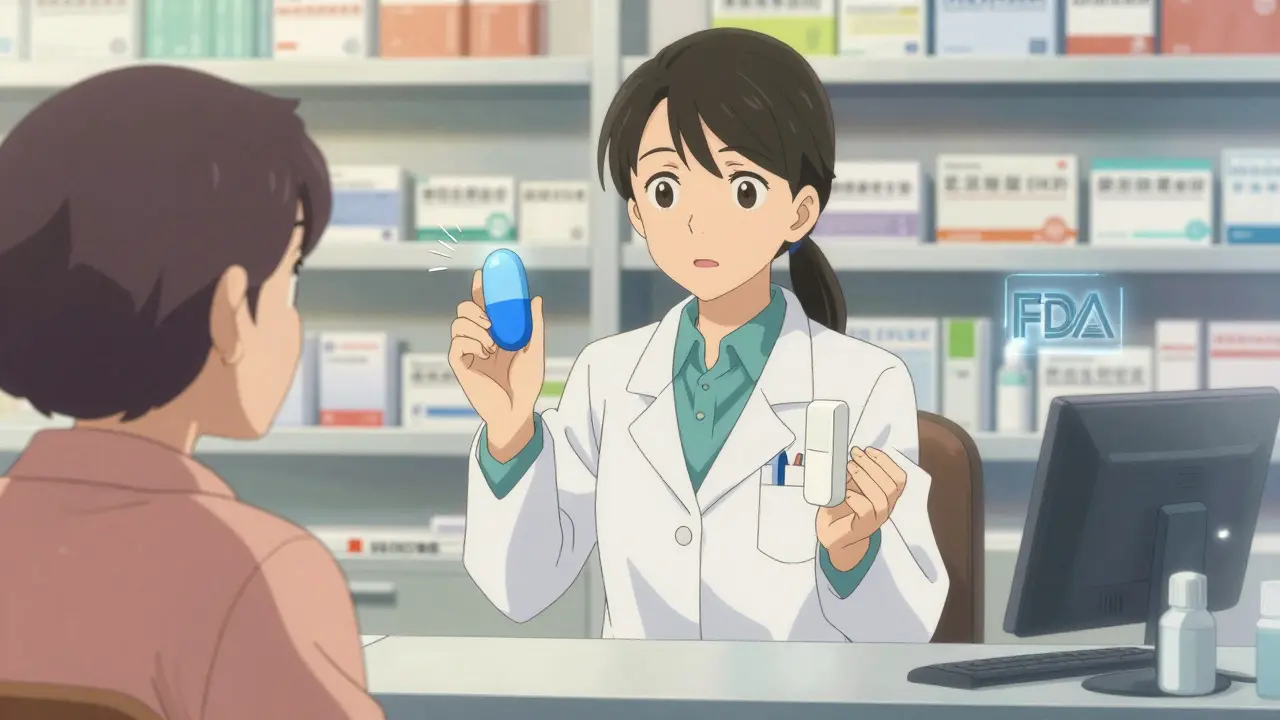
The FDA now offers free, evidence-based tools to help pharmacists. There are counter mats with visual comparisons of brand and generic pills. There are brochures that explain bioequivalence in plain language. And there’s a new digital toolkit called Generics Smart, launched in 2023, which includes 3D pill models and virtual reality demos of manufacturing. In a pilot at 15 CVS pharmacies, it increased acceptance by 29%. One of the most powerful tools is simple: showing patients the pill they’re used to next to the new one. A Healthcare Hotline survey found that 68% of patients would accept generics if they could see a side-by-side comparison. And 41% specifically asked for pictures of the old and new pills. Teach-back works too. Instead of just explaining, ask the patient to explain it back. In a Kaiser Permanente study, using teach-back increased generic acceptance from 54% to 81% across 12,000 patients. When patients say it in their own words, it sticks.Who’s Affected Most
This isn’t just a general issue-it hits certain groups harder. Patients over 65 are nearly twice as likely to hesitate about generics as younger adults. Rural patients report higher concern than urban ones. And those with chronic conditions-like high blood pressure or diabetes-are more likely to stick with brand names out of fear. That’s why a one-size-fits-all approach fails. A patient who’s been on the same medication for 20 years needs a different conversation than a 28-year-old starting their first prescription. Tailoring matters.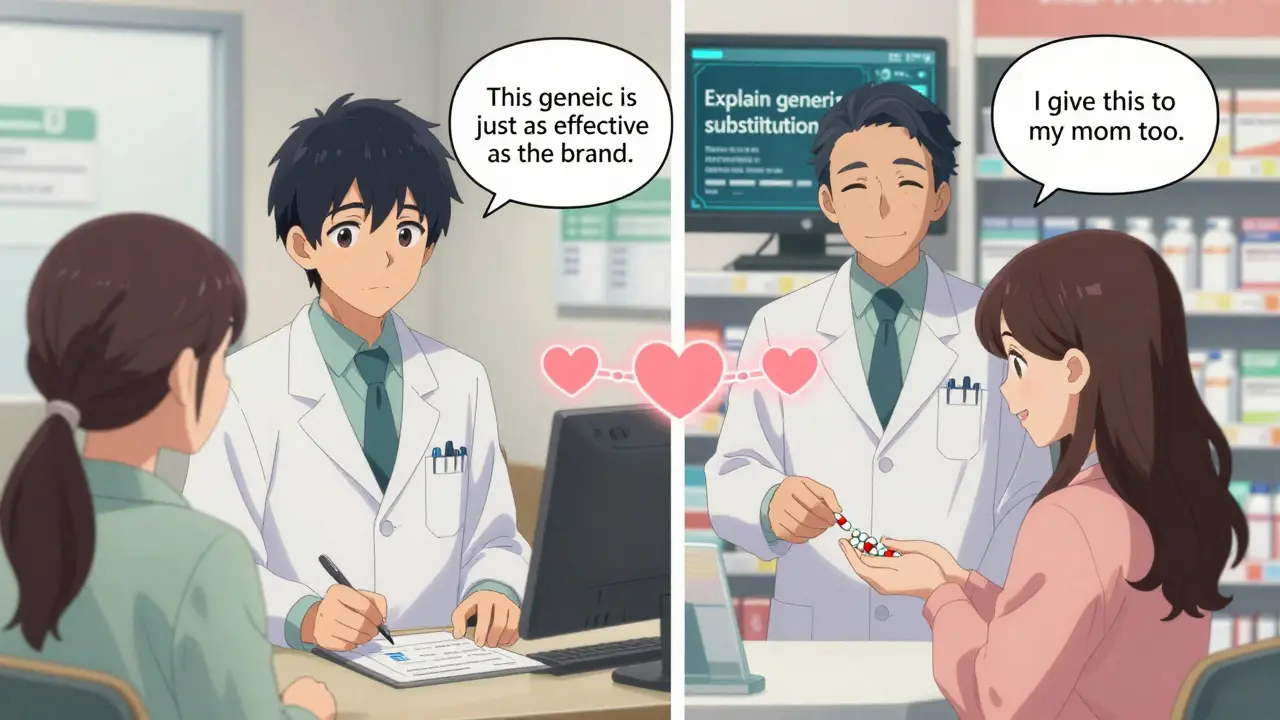
What’s Changing Now
Regulations are catching up. Starting in January 2024, the FDA requires all generic substitution discussions to be documented in patient records using standardized language. And for the first time in 2024, Medicare Part D Star Ratings now include “generic substitution acceptance rate” as a quality metric. Pharmacies that do this well will be rewarded. Those that don’t? They’ll fall behind. Electronic health records are also starting to help. The American Medical Association now recommends automated prompts in EHRs that remind prescribers to explain generics at the time of writing the script. That’s a game-changer. And research is moving forward. The NIH has funded a $2.3 million study testing AI-driven communication tools that adapt to individual patient beliefs. Imagine a system that detects when a patient is skeptical about generics and adjusts its message in real time. That’s not science fiction-it’s coming.What You Can Do Today
You don’t need a fancy toolkit to make a difference. Start here:- Always ask first: “What are your thoughts about this medication?”
- Never say “It’s cheaper.” Say “It has the same active ingredient, no brand name costs.”
- Use a pill comparison chart if you have one-even a printed image helps.
- Share a personal story: “I give this to my mother, too.”
- Use teach-back: “Can you explain why this is safe to me?”
- Coordinate with prescribers. If they mention it at the visit, your job becomes easier.
The Bigger Picture
Generics make up 90.9% of all prescriptions in the U.S., but they cost just 22.9% of total drug spending. That’s over $313 billion saved every year. Yet patient hesitation costs the system $8.2 billion annually in unnecessary brand-name prescriptions. That’s money that could go to better care, better access, better outcomes. This isn’t about pushing pills. It’s about building trust. The data is clear: when pharmacists take the time to listen, explain, and connect, patients choose generics. Not because they’re told to. But because they believe.Why do patients think generics are less effective?
Patients often believe generics are less effective because they look different from the brand-name version they’re used to. Misinformation also plays a role-many think generics contain only 80% of the active ingredient, when in fact, the FDA requires them to deliver 80-125% of the same ingredient. Studies show that 43% of patients hold this misconception. The real issue isn’t the drug-it’s the lack of clear, empathetic communication about how bioequivalence works.
Is it true that generics are made in lower-quality factories?
No. The FDA requires all generic drug manufacturers to meet the same strict quality standards as brand-name companies. In fact, many generic drugs are made in the same facilities as brand-name versions. The FDA inspects both types of facilities using the same criteria. A 2022 report from the FDA’s Center for Drug Evaluation and Research confirmed that there is no difference in manufacturing quality between generics and brand-name drugs.
How can pharmacists overcome patient resistance without spending too much time?
Even a 3-minute conversation can make a big difference. Focus on the Ask-Tell-Ask method: ask what the patient knows, give one clear fact (like “This has the same active ingredient”), then ask them to explain it back. Use visual aids like pill comparison cards-these reduce the need for lengthy explanations. Also, partner with prescribers so the conversation starts before the patient even reaches the pharmacy. The goal isn’t to give a lecture-it’s to build trust quickly and clearly.
Why does saying “It’s cheaper” backfire?
When cost is the only reason given, patients assume the drug is inferior. A 2021 study found that framing generics as “cheaper” increased acceptance by only 7%, while explaining that it’s the same medicine without brand marketing costs increased acceptance by 29%. Patients don’t mistrust generics because they’re expensive-they mistrust them because they’re told they’re a “budget option.” That triggers a subconscious belief that you’re cutting corners on their care.
Can visual aids really improve acceptance?
Yes. A 2022 survey found that 68% of patients would accept generics if shown side-by-side images of the brand and generic pill. Seeing the difference in shape or color helps normalize the change. The FDA’s Generics Smart toolkit includes these visuals, and early pilot data shows a 29% increase in acceptance when they’re used. Visuals bypass language barriers and reduce anxiety by making the abstract concrete.
What’s the role of the prescriber in this process?
The prescriber plays a critical role. When a doctor says, “I’m prescribing this generic because it’s just as effective,” patients are far more likely to accept it. Studies show that when both the prescriber and pharmacist communicate the same message, acceptance jumps to 85%. That’s why automated EHR prompts reminding physicians to explain generics at the time of prescribing are now recommended by the American Medical Association.





1 Comments
Philip Blankenship
February 16, 2026Man, I’ve seen this play out a million times in my pharmacy. Old lady comes in, sees her blood pressure pill changed from a blue oval to a white rectangle, and she’s ready to walk out. I just show her the FDA chart side by side, say, ‘Same stuff, no fancy packaging,’ and boom-she nods like it’s the most obvious thing in the world. No lecture. No jargon. Just truth and a picture. Works every time.
And honestly? The ‘cheaper’ line is the worst. People don’t hate generics-they hate being talked to like they’re dumb. When you frame it as ‘same medicine, no ad budget,’ they feel smart for choosing it. That’s the win.
Also, the VR pill thing? I tried it. My 72-year-old mom thought it was a game. She asked if she could ‘level up’ to the brand version. I said no. She laughed. Accepted it. That’s the future right there.