Opioid Adrenal Insufficiency Risk Calculator
Risk Assessment Tool
Based on clinical guidelines and recent studies showing 5% incidence in high-risk patients
Results will appear here
Most people know opioids can cause constipation, drowsiness, or addiction. But few realize they can also shut down your body’s natural stress response - a silent, dangerous side effect called opioid-induced adrenal insufficiency. It’s rare, but when it happens, it can kill you if no one catches it.
What Exactly Is Opioid-Induced Adrenal Insufficiency?
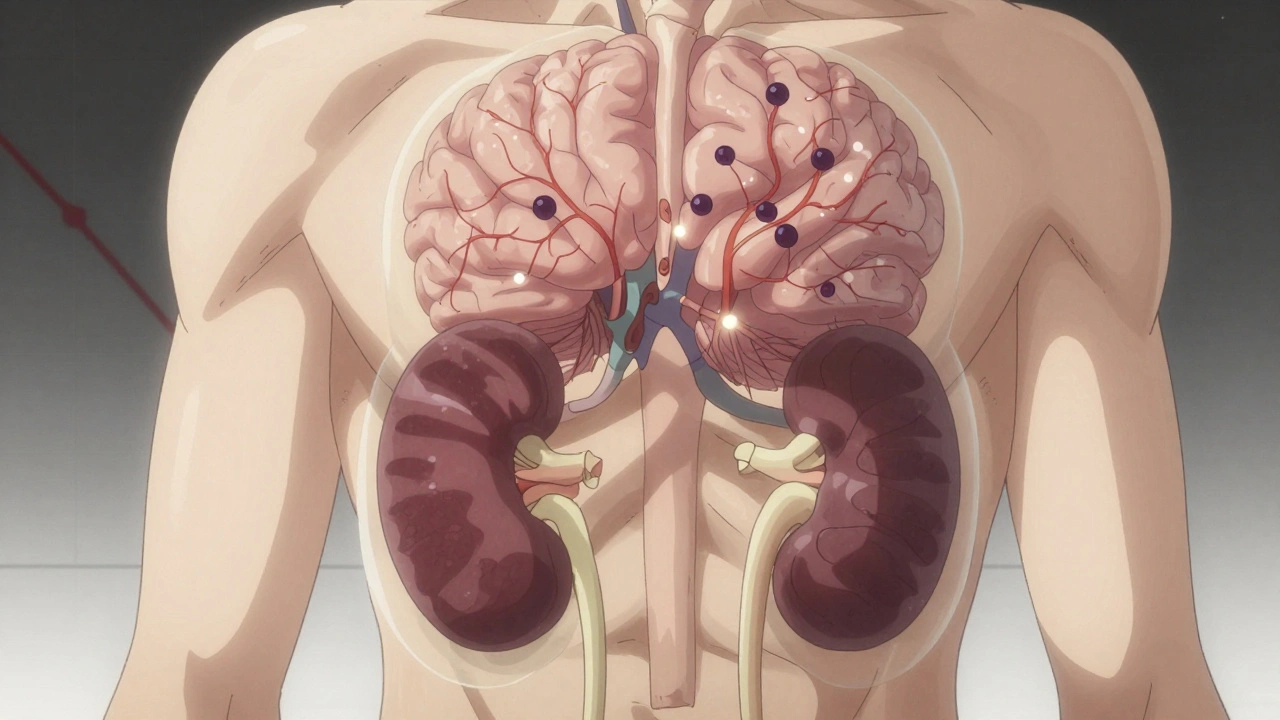
Your adrenal glands sit on top of your kidneys and make cortisol - the hormone that keeps you alive during stress. When you get sick, injured, or even just under serious emotional pressure, cortisol kicks in to raise blood sugar, boost blood pressure, and calm inflammation. Without it, your body can’t cope. Opioids - even when taken exactly as prescribed - can stop your brain from telling your adrenals to make cortisol.
This isn’t damage to the glands themselves. It’s a communication breakdown. Opioids bind to receptors in your hypothalamus and pituitary gland, the brain’s command center for stress response. The result? Less ACTH (the signal hormone), less cortisol, and a body that’s defenseless when it needs to be strongest.
It’s not new science. Studies from the 1970s first noticed this effect. But for decades, doctors dismissed it as a lab curiosity - something that didn’t matter in real life. Now, we know better. In a 2023 study of 162 people on long-term opioid therapy, 5% had adrenal insufficiency. That’s 1 in 20. And those patients were taking more than 20 morphine milligram equivalents (MME) per day - a dose many pain clinics still consider "moderate."
Who’s at Risk?
You don’t need to be a heroin user. This affects people on long-term prescriptions for back pain, arthritis, or cancer-related discomfort. The risk climbs with:
- Daily opioid dose above 20 MME
- Duration longer than 90 days
- Use of methadone or high-dose oxycodone
- Having other chronic illnesses like kidney disease or diabetes
A 2020 review of 27 studies found that 22.5% of long-term opioid users showed signs of adrenal suppression in stimulation tests. That’s more than 1 in 5. Compare that to 0% in healthy people not on opioids. The pattern is clear: higher dose, longer time = higher risk.
And here’s the catch: most of these patients didn’t feel different. No sudden weakness. No weight loss. No darkening skin - the classic signs of Addison’s disease. That’s because their symptoms - fatigue, nausea, dizziness - looked just like their original pain or depression. So no one tested them.
How Is It Diagnosed?
If your doctor suspects this, they’ll order a morning cortisol test. Normal levels are above 5 mcg/dL. If it’s below 3 mcg/dL, that’s a red flag. But the real test is the ACTH stimulation test: you get a shot of synthetic ACTH, and your cortisol is measured 30 and 60 minutes later. A normal response is a peak over 18 mcg/dL. If you stay below that, your adrenal glands aren’t responding - and opioids are likely the cause.
Some newer research suggests even lower cortisol thresholds might be meaningful. One 2024 study proposed that levels under 4 mcg/dL in high-dose opioid users should trigger further testing. But guidelines haven’t caught up yet. That’s why so many cases slip through.
And here’s something critical: opioids don’t affect aldosterone. That’s the hormone that controls salt and potassium. So if you have low sodium or high potassium, it’s probably not from opioid-induced adrenal insufficiency. That’s a clue for doctors to look elsewhere.

What Happens If It’s Not Caught?
Imagine you’re hospitalized for pneumonia. Your body is fighting for survival. Your cortisol should surge. But if opioids have shut it down, your blood pressure crashes. Your blood sugar drops. You go into shock. This is an Addisonian crisis - and it’s fatal if untreated.
One case report from 2015 describes a 25-year-old man recovering from a critical illness. He developed dangerously high calcium levels - a sign his body was breaking down bone for energy because it had no cortisol. He was misdiagnosed for weeks. Only when his cortisol was tested did they realize methadone had caused adrenal failure. Within days of starting steroid replacement, his calcium normalized. After he stopped methadone, his adrenal function returned completely.
That’s the good news: this is reversible. Unlike some forms of adrenal failure that require lifelong treatment, opioid-induced insufficiency usually fixes itself once the drugs are tapered. But you have to survive the first crisis to get there.
Why Is This So Often Missed?
Doctors aren’t trained to look for it. Medical schools barely mention it. Pain management guidelines focus on addiction, tolerance, and overdose - not endocrine side effects. And patients don’t report symptoms because they assume fatigue is just part of chronic pain.
Even when cortisol is low, some doctors assume it’s "just stress" or "not clinically significant." But that’s dangerous thinking. A 2024 review in Frontiers in Endocrinology bluntly says: "A high index of suspicion is prudent for patients treated with high-dose opioids and/or for prolonged periods."
And here’s the irony: patients on opioids often have worse quality of life - less energy, worse mood, more pain - than people not on them. That’s not just the pain talking. It’s low cortisol. One study found opioid users scored significantly lower on the SF-36 health survey across physical, emotional, and social domains. Their bodies were literally running on empty.
What Should You Do?
If you’ve been on opioids for more than three months - especially at doses above 20 MME - and you feel constantly tired, dizzy, nauseous, or weak, ask your doctor for a cortisol test. Don’t wait for a crisis. Bring up the possibility of opioid-induced adrenal insufficiency. Mention the 2023 and 2024 studies. Most doctors haven’t heard of it, but they’ll listen if you come prepared.
If you’re a doctor: Screen patients on chronic high-dose opioids. Test morning cortisol. If it’s low, do the ACTH stimulation test. Don’t assume it’s depression or deconditioning. Start glucocorticoid replacement if confirmed - and taper opioids slowly under endocrine supervision. You might save a life.
The Bigger Picture
Over 5% of the U.S. population is on chronic opioid therapy. That’s millions of people. Even if only 5% of them develop adrenal insufficiency, that’s still 100,000+ cases. Most are undiagnosed. And every one of them is one infection, one fall, one surgery away from disaster.
This isn’t about stopping pain treatment. It’s about making it safer. We don’t need fewer opioids. We need smarter prescribing - and better monitoring. If you’re managing chronic pain, your body’s stress system matters as much as your spine or your joints. It’s time we treated it that way.
Can You Recover?
Yes. In every documented case where opioids were tapered or stopped, adrenal function returned. Some patients saw improvement in weeks. Others took months. But cortisol levels climbed back up. The glands weren’t broken - they were silenced. And once the opioids were out of the way, they woke up.
That’s the most important thing to remember: this isn’t permanent. It’s treatable. And it’s preventable - if you know to look for it.
11 Comments
Olivia Portier
December 11, 2025omg i had no idea opioids could do this 😱 i’ve been on them for 8 months for my back and i’m always so tired but thought it was just the pain or me being lazy. time to ask my doc for a cortisol test.
Jennifer Blandford
December 12, 2025THIS. I’m so glad someone finally said it. My cousin almost died after a minor surgery because no one checked her cortisol. She was on oxycodone for 2 years for fibromyalgia. They thought she was just ‘depressed.’ Turns out her body was running on fumes. She’s fine now but scared to even sneeze without steroids. We need WAY more awareness.
Ryan Brady
December 13, 2025lol another anti-opioid scare tactic. You people act like every pain patient is a junkie. My dad’s on methadone for 15 years and he’s still working construction. Stop scaring people for clicks.
Rich Paul
December 14, 2025Actually, the HPA axis suppression is well-documented in endocrinology literature since the 80s. The ACTH stimulation test is gold standard, but cortisol binding globulin (CBG) dysregulation in chronic opioid users can cause false low total cortisol readings. Free cortisol assays are more accurate. Also, methadone’s half-life skews circadian rhythm - morning cortisol might be artificially suppressed. Recommend dynamic testing with insulin tolerance test if borderline.
Darcie Streeter-Oxland
December 14, 2025It is, indeed, a matter of considerable concern that this condition remains under-recognized within primary care and pain management protocols. The literature, as cited, is robust and unequivocal. One may reasonably posit that the absence of routine screening constitutes a systemic failure in clinical vigilance. I urge the medical establishment to implement mandatory endocrine assessment for patients exceeding 20 MME for durations surpassing 90 days. The cost of inaction is, quite frankly, unacceptable.
Mona Schmidt
December 15, 2025Thank you for writing this. I’ve been telling my rheumatologist for months that I feel like I’m walking through mud every morning. She said it was just aging. I’m 42. I asked for a cortisol test last week. It came back at 2.1. They’re doing the ACTH test next week. I’m terrified, but also relieved I’m not crazy. This is real. And it’s not just me.
Guylaine Lapointe
December 16, 2025Of course this happens. People take opioids like candy now. It’s not about pain - it’s about avoiding life. You think you’re managing arthritis? You’re just numbing yourself. This is the price of modern weakness. If you can’t handle discomfort, maybe you shouldn’t be on drugs at all. This isn’t a medical crisis - it’s a moral one.
Sarah Gray
December 16, 2025Wow. Another person who thinks every side effect is a conspiracy. I’ve seen 12 patients on opioids with low cortisol. All of them had depression, poor sleep, and no real pathology. Cortisol is not a magic bullet. You can’t diagnose adrenal insufficiency based on fatigue alone. This is dangerous misinformation. Stop giving patients permission to doubt their doctors.
Kathy Haverly
December 16, 2025So now we’re blaming opioids for everything? What about the 70% of people who take them and don’t have this? You’re pathologizing normal human suffering. This isn’t science - it’s fearmongering dressed up as medicine. Your ‘1 in 20’ statistic? Probably inflated by selection bias. And why no mention of the fact that cortisol levels naturally decline with age? You’re just scaring people to sell more tests.
Arun Kumar Raut
December 18, 2025Very important post. My uncle in India was on tramadol for years. He got very weak after flu. Doctors thought it was dengue. Later found out his cortisol was zero. He is fine now after steroids and stopping tramadol. This should be told to every doctor who gives opioids. Not just in US.
om guru
December 19, 2025Adrenal suppression from opioids is reversible. Test morning cortisol. If below 5, proceed with ACTH stimulation. Replace glucocorticoids if confirmed. Taper opioids under supervision. Recovery is expected. This is not speculation. This is protocol.