If you have allergies and keep getting sinus infections, you’re not alone. About 30 to 40% of all chronic sinusitis cases are tied directly to allergic reactions. It’s not just a stuffy nose that goes away after a week-it’s a cycle: your allergies trigger swelling in your sinuses, the mucus gets trapped, bacteria grow, and the inflammation sticks around for months. Standard cold remedies don’t cut it. You need a targeted plan that tackles both the allergy and the sinus inflammation at the same time.
Why Allergies Make Sinusitis Worse
Allergies don’t just cause sneezing and itchy eyes. When you breathe in pollen, dust mites, or mold, your immune system overreacts. That reaction swells the lining of your nasal passages and sinuses. Swollen tissue blocks the tiny drainage channels between your sinuses and nose. Mucus builds up. Bacteria multiply. What starts as mild congestion turns into a deep, persistent ache around your eyes, forehead, or cheeks.
Unlike regular sinus infections that clear up in 7 to 10 days, allergy-driven sinusitis often lasts longer than 12 weeks-this is called chronic sinusitis. And here’s the kicker: even after the infection clears, the underlying allergy keeps the inflammation going. That’s why so many people feel better for a few days after antibiotics, then crash again a week later. Antibiotics treat the bacteria, but they don’t fix the root cause: your allergic response.
First-Line Treatments That Actually Work
The most effective starting point isn’t antibiotics-it’s nasal corticosteroids. These aren’t the same as the steroids athletes use. They’re local anti-inflammatories sprayed directly into your nose. Options like fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort) reduce swelling, open up drainage, and lower mucus production. But they don’t work overnight. You need to use them every day for at least two to four weeks before you feel real relief. And here’s where most people fail: they stop after a week because they don’t see immediate results. That’s why adherence drops to just 35-40% after four weeks.
Alongside nasal sprays, saline irrigation is a game-changer. Using a neti pot or squeeze bottle with distilled or boiled water and a saline packet helps flush out allergens, mucus, and irritants. Do it once or twice daily. But don’t use tap water. Between 2011 and 2020, the CDC documented rare but deadly brain infections from Naegleria fowleri-amazingly, nearly all cases came from people rinsing their sinuses with unboiled tap water.
Oral antihistamines like cetirizine or loratadine help with sneezing and runny nose, but they don’t reduce sinus swelling as well as nasal steroids. One 2021 study showed fluticasone cut symptoms by 65%, while cetirizine only helped by 42%. If you’re still congested after two weeks of nasal steroids and saline, it’s time to reassess.
When Antibiotics Are-and Aren’t-Helpful
Antibiotics are overused in sinusitis. The Infectious Diseases Society of America says most acute cases (under 4 weeks) don’t need them. But in allergy sufferers, things get messy. About 0.5 to 2% of allergy-related sinusitis cases develop a bacterial superinfection. That’s when you get thick, yellow-green mucus, fever, and worsening pain after 5 to 7 days of seeming improvement.
If that happens, amoxicillin is the go-to first antibiotic. Take 500mg three times a day for 5 to 10 days. If you’ve been on antibiotics before or your symptoms don’t improve, your doctor may switch to amoxicillin-clavulanate (Augmentin), a stronger combo. But here’s the truth: antibiotics alone only work in 35 to 45% of allergy-driven cases. That’s because the real problem isn’t bacteria-it’s the inflammation keeping the sinuses blocked. Without fixing the allergy, the infection keeps coming back.

Advanced Options for Stubborn Cases
If you’ve tried nasal steroids, saline, and antibiotics-and you still have symptoms after 4 to 6 weeks-it’s time to think bigger. One red flag: nasal polyps. These are soft, noncancerous growths inside your nose that block airflow and drainage. Up to 70% of people with chronic sinusitis and polyps also have allergies. If you’ve got polyps, your doctor may recommend a biologic.
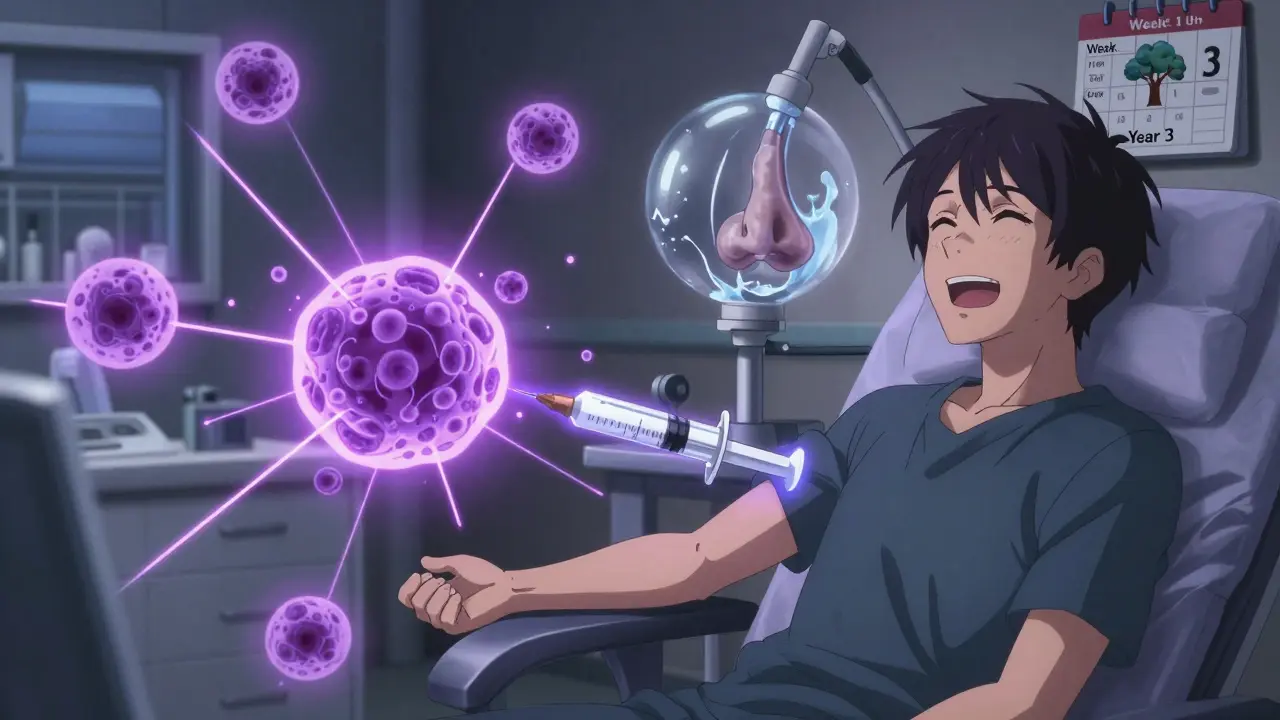
Biologics are targeted shots that block specific parts of your immune system’s allergic response. Dupilumab (Dupixent) is the most common. It’s given as a shot under the skin every two weeks. In clinical trials, it reduced nasal polyp size by 73% and improved breathing in 80% of users. But it costs around $3,500 a month without insurance. Omalizumab (Xolair) and mepolizumab (Nucala) are alternatives, each with slightly different targets. These aren’t cures-they’re long-term controllers for severe cases.
Another emerging option is tezepelumab (Tezspire), approved by the FDA in early 2023. It works higher up in the immune cascade and has shown a 56% drop in sinus flare-ups in trials. It’s not yet widely used, but it’s gaining traction for patients who don’t respond to dupilumab.
Immunotherapy: The Long-Term Fix
If you’re allergic to things like ragweed, dust mites, or pet dander, allergy shots (immunotherapy) can change the game. This isn’t a quick fix. You start with weekly injections for 4 to 6 months, then move to monthly shots for 3 to 5 years. But the payoff? Studies show 60 to 70% of patients see a big drop in sinus infections after completing the full course. That’s way better than the 25 to 30% improvement you get from meds alone.
There’s also sublingual immunotherapy-drops or tablets under the tongue. It’s less invasive than shots and approved for certain allergens like grass, ragweed, and dust mites. It’s not as strong as injections, but for people who hate needles, it’s a solid option.
When to See an ENT Specialist
You don’t need to wait until you’re desperate. See an ear, nose, and throat (ENT) specialist if:
- Your symptoms last more than 4 to 6 weeks despite proper treatment
- You have nasal polyps (visible or confirmed by endoscopy)
- You get 4 or more sinus infections a year
- You have complications like eye swelling, vision changes, or severe headaches
- Your doctor suspects fungal sinusitis (common in people with long-term allergies)
ENTs use a thin, flexible scope to look inside your nose and sinuses. They can see swelling, polyps, or pus that you can’t feel. This isn’t just a checkup-it’s a diagnostic tool that guides the next step. If your sinuses are structurally blocked or polyps keep growing back, surgery might be next.
Surgery: What to Expect
Endoscopic sinus surgery opens up blocked passages and removes polyps. It’s done under general anesthesia, takes about an hour, and most people go home the same day. Success rates are high-85% of patients report major symptom relief. But here’s the catch: in allergy sufferers, the polyps and inflammation can come back. Studies show 20 to 30% of allergic patients need another procedure within 5 years, compared to just 10 to 15% of non-allergic patients.
Surgery doesn’t replace allergy treatment. It’s a reset button. After surgery, you still need nasal steroids, saline rinses, and possibly immunotherapy to keep the inflammation from returning.
What’s Changing in 2026
The field is moving fast. In January 2024, allergy and immunology groups updated guidelines to recommend intranasal antifungals for people living in mold-heavy areas. Early trials showed a 32% drop in symptom severity. Researchers are also exploring microbiome therapies-using good bacteria to crowd out bad ones in the sinuses. Early data suggests this could cut antibiotic-resistant cases by 45% in the next five years.
But big gaps remain. Rural patients wait 30 to 40% longer than urban ones to see a specialist. Cost is a barrier too. Biologics are life-changing, but most insurance requires years of failed treatments before approving them. And while women are 1.3 times more likely to develop chronic sinusitis than men, research still lags on why.
The bottom line? Allergy-related sinusitis isn’t something you just live with. It’s a treatable condition-but only if you treat the allergy and the sinusitis together. Don’t settle for temporary fixes. Ask your doctor about testing, immunotherapy, and whether a specialist referral could break the cycle for good.
Can allergies cause chronic sinusitis?
Yes. Allergies are one of the most common causes of chronic sinusitis. When your immune system reacts to allergens like pollen or dust mites, it triggers inflammation in your nasal passages and sinuses. This swelling blocks drainage, traps mucus, and creates an environment where infections can linger. Up to 70% of people with chronic sinusitis also have allergic rhinitis.
Do I need antibiotics for sinusitis if I have allergies?
Not usually. Most sinusitis in allergy sufferers is caused by inflammation, not bacteria. Antibiotics only help if a bacterial infection develops on top of the allergy-driven swelling-which happens in less than 2% of cases. Even then, antibiotics alone won’t stop the cycle. Nasal steroids and saline rinses are more important long-term.
How long does it take for nasal steroids to work?
It takes 2 to 4 weeks of daily use before you feel the full effect. Many people stop too early because they don’t see instant results. But consistency is key. Missing doses or using them only when symptoms flare reduces effectiveness. Think of them like a daily vitamin for your sinuses-not a painkiller.
Are allergy shots worth it for sinusitis?
For many people, yes. Allergy immunotherapy (shots or drops) can reduce sinus infections by 60 to 70% over 3 to 5 years. It works by training your immune system to stop overreacting to allergens. It’s a long commitment-weekly shots at first, then monthly-but it’s one of the few treatments that can actually change the course of your allergies and prevent recurring sinusitis.
What’s the difference between sinusitis and a regular cold?
A cold usually clears up in 7 to 10 days and comes with a sore throat, cough, and mild fever. Sinusitis lasts longer-often more than 12 weeks-and features deep facial pressure, thick discolored mucus, reduced smell, and fatigue. If your symptoms linger past 10 days or keep coming back, it’s not a cold-it’s likely sinusitis, especially if you have allergies.
Can I use a neti pot with tap water?
No. Never use tap water in a neti pot. It can contain tiny organisms like Naegleria fowleri, which can cause a rare but deadly brain infection. Always use distilled water, sterile water, or water that’s been boiled for at least one minute and cooled. Clean your neti pot after every use with hot water and soap, and let it air-dry.
Is surgery a cure for sinusitis caused by allergies?
No. Surgery opens blocked sinuses and removes polyps, which gives you relief-but it doesn’t fix the allergy. Without ongoing allergy management (steroids, rinses, immunotherapy), polyps and inflammation often return within a few years. Surgery is a tool to reset your sinuses, not a permanent solution.




13 Comments
Ashley S
January 6, 2026This is why people are so sick all the time-they just take Sudafed and call it a day. No one wants to do the work. Spray your nose? Rinse? See a specialist? Nah, let me just suffer and blame the air.
Jeane Hendrix
January 6, 2026Okay but like… has anyone actually tried dupilumab? I’m on it and it’s wild. My polyps shrunk so fast I thought I was hallucinating. Also, the shot? Barely even feels like a pinch. 🤯 But yeah, the cost is insane-my insurance made me try 7 other things first. Like, I’ve been sick since 2019. Can we just skip the middleman??
Gabrielle Panchev
January 6, 2026Let me just say this-there is a systemic failure here: the medical-industrial complex is profiting off of your temporary relief, not your long-term health. Antibiotics are cheap, easy, and reimbursable; nasal steroids require discipline, consistency, and a willingness to tolerate a slight burning sensation for six weeks-which, let’s be honest, most Americans equate with torture. And don’t even get me started on the fact that biologics are priced like luxury handbags while people are dying from Naegleria because they used tap water in a neti pot. We have the science. We have the tools. But we don’t have the will. And that’s not a medical problem-it’s a moral one.
Vinayak Naik
January 7, 2026Bro in India we call this ‘jhatka sinus’-allergies turning into full-blown head pressure. I used to take antibiotics every season till I learned about saline rinse. Now I do it with rock salt + boiled water. Game changer. Also, don’t sleep with fans on-dust swirls like a tornado. And yeah, shots work. My cousin did 3 years, now he hikes in pollen season like a boss. No drama. Just discipline.
Saylor Frye
January 9, 2026Wow. Such a comprehensive guide. Truly, I’m impressed someone managed to write 2,000 words without using the word ‘holistic.’ But let’s be real-this reads like a pharma whitepaper disguised as a Reddit post. Did you get paid to write this? Because I’m suspicious.
Kiran Plaha
January 10, 2026I had this for years. Felt like my face was full of wet cement. Tried everything. Then my doctor said ‘try Flonase daily, no excuses.’ I did. 3 weeks later? I could breathe through my nose for the first time in 8 years. I cried. It’s not magic. It’s just… consistent care. Don’t give up.
Matt Beck
January 10, 2026Life is a cycle of inflammation, isn’t it? 🌱 We’re all just trying to survive the chaos of our own immune systems. Allergies? Sinusitis? It’s just your body screaming, ‘I’m not okay with this world!’ And yet-we medicate instead of… I don’t know… move to a forest? Meditate? Stop eating gluten? 😔 The real cure is inner peace. Or maybe just a better filter on your AC.
Molly McLane
January 12, 2026For anyone new to this-don’t feel ashamed if you’ve been using tap water in your neti pot. You’re not alone. But now you know. And knowledge is power. Start today. Use boiled water. Clean your pot. Breathe easier. You deserve to feel good in your own body. And if you’re struggling with cost? Ask your doctor about patient assistance programs. They exist. You just have to ask.
Wesley Pereira
January 14, 2026Okay so I’ve been on this ride for 12 years. Antibiotics? Check. Neti pot? Check. Flonase? Twice a day like a monk. And guess what? Still got polyps. So I did the shots. 3 years. Now I’m off them. My ENT says I’m one of the rare ones who actually stuck with it. So if you’re thinking ‘nah, I’ll just wait’-don’t. This ain’t a Netflix binge. It’s your sinuses. Do the work. Even when it sucks.
Stuart Shield
January 16, 2026I used to think sinusitis was just ‘bad luck.’ Then I moved from London to rural Oregon and my nose turned into a swamp. Turned out I was allergic to everything out here-ragweed, mold, pine pollen. I thought I was just ‘sick.’ Turns out I was allergic to my new home. Took me two years to figure it out. Now I use saline twice a day and carry a steroid spray like it’s my wallet. Don’t wait till you’re sobbing in the shower.
Indra Triawan
January 16, 2026I just want to know… why does no one talk about how lonely this is? You’re tired all the time. People think you’re faking it because you ‘just have allergies.’ You cancel plans. You miss work. You feel like a burden. And then you read this article and it’s all ‘just use Flonase’ like it’s that easy. No one says, ‘I see you. This is hard.’
Joann Absi
January 18, 2026AMERICA IS BEING POISONED BY MOLD AND BIG PHARMA! 🇺🇸🔥 This isn’t health care-it’s a scam! They want you on drugs FOREVER! They don’t want you to heal-they want you to PAY! Use Himalayan salt! Sleep on copper! Go off-grid! Stop drinking cow milk! This article is just a corporate ad for dupilumab! 🤡
Mukesh Pareek
January 19, 2026Most people don’t even know what a cytokine is. You’re talking about biologics like they’re vitamins. If you don’t have a PhD in immunology, you shouldn’t be self-prescribing. Stick to saline. That’s it. The rest is snake oil wrapped in FDA approval.