Opioid Therapy Risks: What You Need to Know About Pain Management Dangers
When you hear opioid therapy, a medical treatment using drugs like oxycodone, hydrocodone, or morphine to manage moderate to severe pain. Also known as narcotic pain relief, it can be life-changing for people with cancer, surgery recovery, or serious injuries—but it’s also one of the most dangerous treatments in modern medicine. The CDC reports that over 70% of drug overdose deaths in the U.S. involve opioids, and many start with a simple prescription. This isn’t about street drugs—it’s about pills given by doctors, taken as directed, and still leading to addiction.
One of the biggest opioid dependence, a physical and psychological reliance on opioid medications that develops even with short-term use isn’t always obvious. People don’t wake up addicted. It creeps in. Your body adapts. You need more to get the same relief. Then you feel sick if you skip a dose. That’s not weakness—it’s biology. And it can happen in as little as two weeks. opioid overdose, a life-threatening reaction where breathing slows or stops due to excessive opioid use doesn’t always mean someone took too many pills. Sometimes it’s mixing opioids with alcohol, sleep aids, or even certain anxiety meds. The risk goes up if you’re over 65, have lung problems, or take more than 50 morphine milligram equivalents daily.
Long-term opioid therapy, a medical treatment using drugs like oxycodone, hydrocodone, or morphine to manage moderate to severe pain can cause hormonal changes, immune suppression, and even increased pain sensitivity over time—called opioid-induced hyperalgesia. That means the drug meant to reduce pain ends up making it worse. Many patients don’t realize this is happening until they try to stop and face withdrawal, depression, or unexplained aches. That’s why guidelines now push for the lowest effective dose for the shortest time possible.
There are alternatives. Physical therapy, nerve blocks, cognitive behavioral therapy, and non-opioid meds like gabapentin or NSAIDs often work just as well for chronic pain—with far fewer risks. Even for acute pain after surgery, combining acetaminophen and ibuprofen can cut opioid needs by half. The goal isn’t to avoid opioids entirely—it’s to use them wisely, monitor closely, and have an exit plan before you start.
What you’ll find below are real, practical guides on how opioid therapy intersects with other treatments, what to watch for, and how to protect yourself or a loved one when these drugs are part of your care plan. These aren’t theoretical warnings—they’re stories from people who’ve been there, and the science that backs up what they lived through.
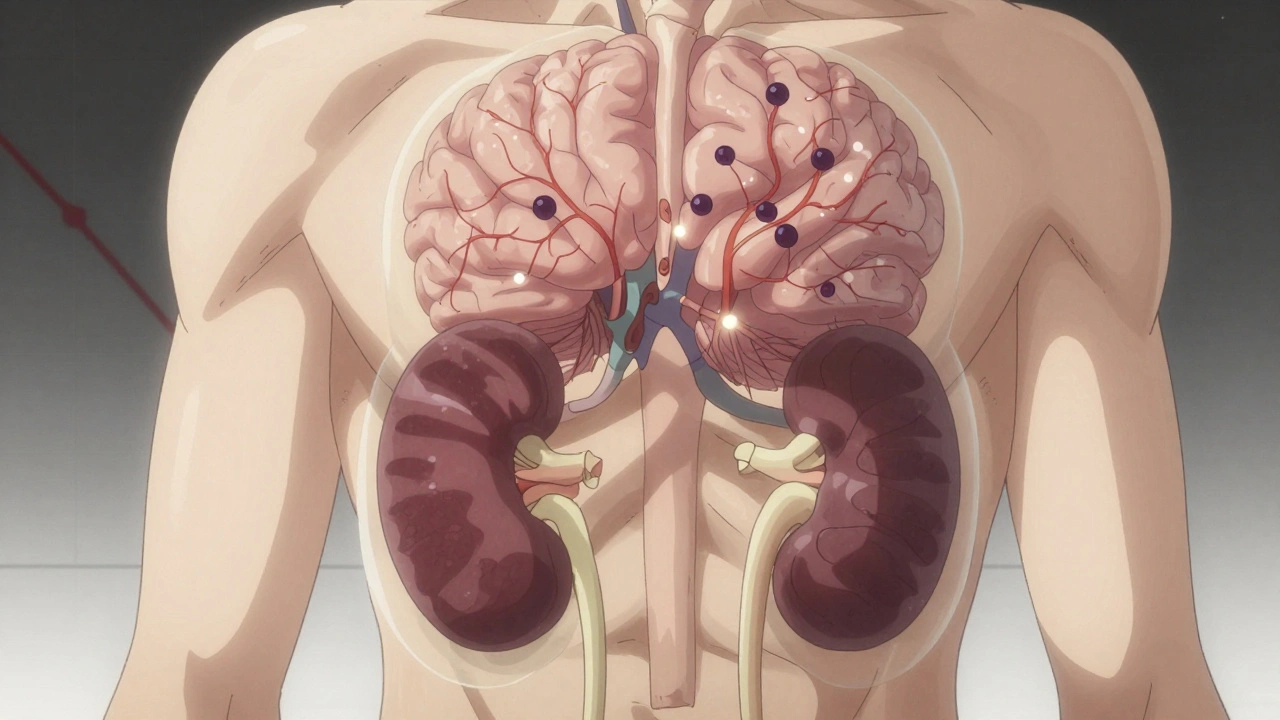
Opioids and Adrenal Insufficiency: A Rare but Life-Threatening Side Effect You Need to Know
Opioid-induced adrenal insufficiency is a rare but life-threatening side effect of long-term opioid use. It suppresses cortisol production, leaving patients vulnerable to crisis during stress. Early testing can save lives.
Continue Reading



