Key Takeaways
- Budesonide is a locally acting corticosteroid that targets gut inflammation with fewer systemic side effects.
- It is most effective for mild‑to‑moderate Crohn's disease and ulcerative colitis affecting the colon and ileum.
- Enteric‑coated formulations (e.g., Entocort EC) release the drug in the distal intestine, exploiting high first‑pass metabolism.
- Typical regimens last 8-12 weeks, followed by tapering to avoid adrenal suppression.
- When budesonide fails, escalation to biologics or surgery is recommended per NICE guidelines.
When you hear the name Budesonide is a synthetic glucocorticoid designed to act mainly inside the gastrointestinal tract. Thanks to its high first‑pass metabolism in the liver, less than 10% reaches the bloodstream, which means you get strong anti‑inflammatory action where you need it without the classic steroid baggage.
Inflammatory bowel disease (Inflammatory Bowel Disease, or IBD) is an umbrella term for chronic conditions that cause painful inflammation of the intestine. The two most common forms are Crohn's disease and ulcerative colitis. Both can lead to abdominal pain, diarrhea, fatigue, and weight loss, but they differ in the depth and pattern of bowel involvement.
Why Budesonide Became a Go‑to Option for IBD
Traditional steroids like prednisone flood the whole body with cortisol‑like hormones, which can trigger weight gain, bone loss, and blood‑sugar spikes. Budesonide was engineered to stay mostly in the gut, giving it a better safety profile for long‑term use. The drug’s high affinity for glucocorticoid receptors shuts down the inflammatory cascade-lowering cytokines such as TNF‑α, IL‑1β, and IL‑6-while sparing the rest of the body.
Clinical trials from 2022‑2024 show that budesonide induces remission in about 55‑60% of patients with mild‑to‑moderate Crohn's disease limited to the ileum or right colon. For ulcerative colitis affecting the distal colon, remission rates hover around 45‑50% when used for 8 weeks. Those numbers are comparable to oral prednisone but with half the dropout rate due to side effects.
How Budesonide Is Formulated for Targeted Delivery
The magic lies in the enteric‑coated capsules (brand name Entocort EC in the UK). The coating resists dissolution in the stomach’s acidic environment and only breaks down in the higher pH of the ileum or colon. This timing ensures the drug meets inflamed tissue head‑on.
Another version, Pulmicort (inhalation spray), isn’t meant for IBD but highlights budesonide’s versatility. For gut use, the recommended dosage is 9mg once daily for adults, taken with food to aid absorption. Children over 6years may start at 6mg, adjusted by weight.
Step‑by‑Step Guide to Starting Budesonide
- Confirm diagnosis with colonoscopy and biopsy. A recent Colonoscopy report helps map disease extent.
- Discuss with your gastroenterologist whether your IBD is mild‑to‑moderate and limited to the last part of the small intestine or colon-these are the sweet spots for budesonide.
- Obtain a prescription for the delayed‑release capsule (Entocort EC). In the UK, the NHS typically covers it under the NICE guideline NG130.
- Take the capsule each morning with breakfast. Swallow whole-no crushing or chewing.
- Schedule a follow‑up at 8 weeks. Your doctor will assess symptoms, stool frequency, and may repeat blood markers like C‑reactive protein (CRP).
- If remission is achieved, begin a taper: 9mg → 6mg → 3mg over 2‑week intervals to reduce adrenal suppression risk.
- Maintain a maintenance plan that includes diet, stress management, and possibly a low‑dose 5‑ASA if needed.

Comparing Budesonide with Other IBD Medications
| Drug | Typical Indication | Remission Rate (8‑12 wk) | Common Side Effects | Systemic Exposure |
|---|---|---|---|---|
| Budesonide | Mild‑to‑moderate ileal/colonic Crohn’s, distal ulcerative colitis | 55‑60% | Mild oral thrush, headache | Low (≈10% systemic) |
| Prednisone | Moderate‑to‑severe IBD across any segment | 65‑70% | Weight gain, hypertension, osteoporosis | High (≈90% systemic) |
| Mesalamine | Maintenance of remission in ulcerative colitis | 30‑35% | Nausea, kidney dysfunction (rare) | Negligible |
When Budesonide Isn’t Enough
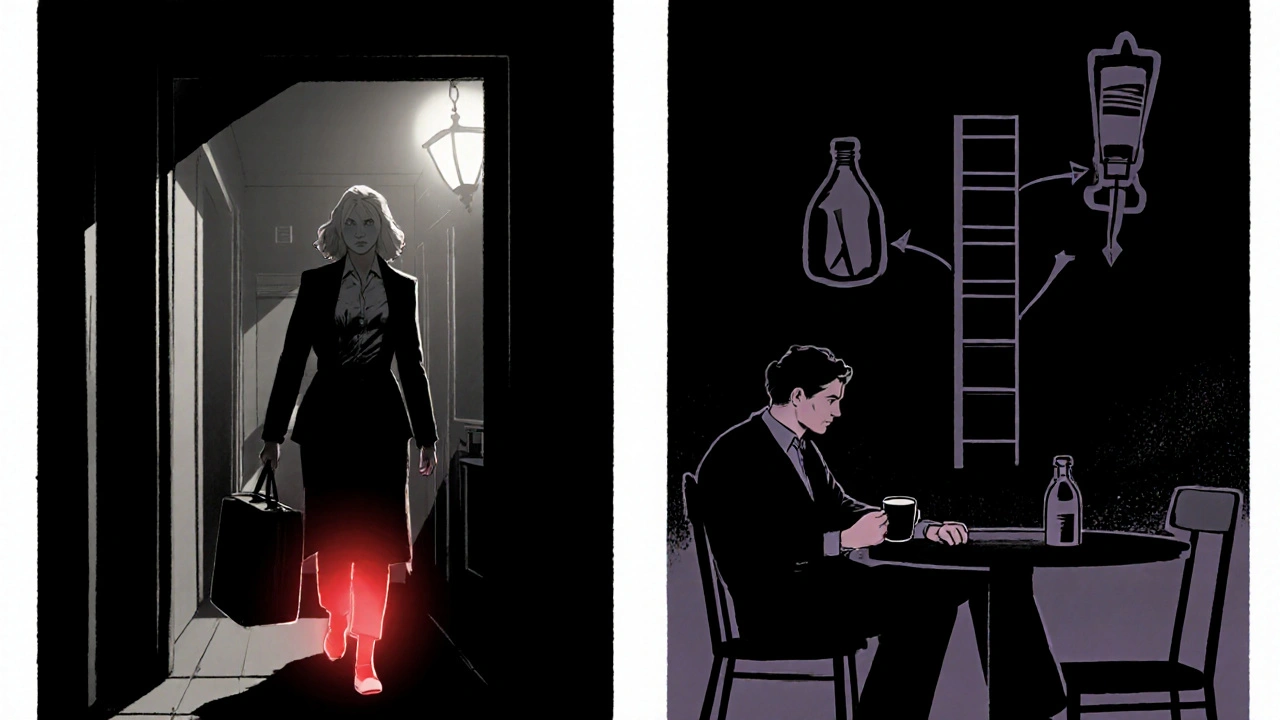
About 30‑40% of patients either don’t respond or lose response after a few months. In those cases, the treatment ladder moves upward:
- Biologics such as infliximab, adalimumab, or vedolizumab target specific immune pathways and have shown remission rates >70% in refractory disease.
- Small‑molecule Janus kinase (JAK) inhibitors-tofacitinib for ulcerative colitis-offer an oral alternative but come with a black‑box warning for thrombosis.
- For localized strictures or perforation, surgical resection remains the definitive option.
British NICE guideline NG130 advises that budesonide should be trialed for at least 8 weeks before deciding on escalation. If you’re still symptomatic after a proper taper, discuss the next step with your specialist.
Monitoring and Managing Side Effects
Even with low systemic absorption, caregivers watch for adrenal suppression, especially when treatment exceeds 12 weeks. A simple morning cortisol level can flag problems early. If cortisol falls below 5µg/dL, taper more slowly or switch to a non‑steroidal agent.
Other manageable issues include:
- Oral candidiasis-use a sugar‑free chlorhexidine mouthwash.
- Headaches-often resolve after the first week.
- Transient rise in blood sugar-monitor if you have diabetes.
Never combine budesonide with CYP3A4 inhibitors like ketoconazole without medical advice, as they can raise systemic levels.
Real‑World Patient Stories
Emma, a 28‑year‑old teacher from Manchester, struggled with Crohn’s flares that kept her off work. After a colonoscopy confirmed ileal disease, her gastroenterologist started budesonide 9mg. Within six weeks, her pain scores dropped from 8/10 to 2/10, and she could return to teaching. She tapered over four weeks and now stays on a low‑dose 5‑ASA for maintenance.
James, 45, has ulcerative colitis limited to the sigmoid colon. He tried mesalamine for years with modest benefit, then switched to budesonide during an acute flare. After eight weeks, his stool frequency fell from 8 to 2 per day, and his CRP normalized. He now follows a low‑FODMAP diet and sees his doctor every six months.
Key Points to Remember
- Ask your doctor if your disease location (ileum or distal colon) matches budesonide’s target area.
- Stick to the prescribed dosing schedule; don’t crush the enteric‑coated tablets.
- Plan a taper to avoid adrenal issues, especially after more than 8 weeks of use.
- Keep regular labs (CRP, cortisol) and schedule colonoscopy checks as advised.
- Know when to move on: persistent symptoms after a full course signal the need for biologics or surgery.
Frequently Asked Questions
How long does a typical budesonide course last?
The standard induction lasts 8-12 weeks, followed by a gradual taper over 2-4 weeks to minimise adrenal suppression.
Can I take budesonide with other IBD meds?
Yes, it’s often combined with a 5‑ASA for maintenance or used before starting biologics. Always check for drug‑interaction warnings, especially with CYP3A4 inhibitors.
What are the signs of adrenal suppression?
Fatigue, dizziness, low blood pressure, and difficulty coping with stress can indicate low cortisol. A morning serum cortisol test confirms the diagnosis.
Is budesonide safe during pregnancy?
Current data suggest low systemic exposure makes it relatively safe, but you should discuss risks and benefits with your obstetrician and gastroenterologist.
How does budesonide compare to prednisone in cost?
In the UK, budesonide is often reimbursed via the NHS under NICE NG130, whereas prednisone is cheaper but may lead to higher long‑term costs due to side‑effect management.
Understanding how budesonide fits into the IBD treatment puzzle helps you make informed choices, stay ahead of flare‑ups, and keep your life moving forward.






11 Comments
Jason Montgomery
October 16, 2025Hey folks, great rundown on budesonide! If you're new to IBD meds, just remember the key is consistency – take that capsule with breakfast and don’t crush it. The taper schedule might feel weird, but it really saves you from adrenal hiccups later. Keep tracking your stool count and energy levels, and let your doc know if anything feels off. Stay hopeful, this drug can be a real game‑changer for many.
Kenny ANTOINE-EDOUARD
October 25, 2025Budesonide’s pharmacokinetics are worth noting: the high first‑pass metabolism keeps systemic exposure under 10 %, which translates to fewer classic steroid side effects. For mild‑to‑moderate Crohn’s limited to the ileum, the 9 mg daily dose induces remission in roughly 55‑60 % of patients after eight weeks. In ulcerative colitis of the distal colon, remission hovers near 45‑50 %, still respectable compared to systemic prednisone. Monitoring should include a morning serum cortisol after any course exceeding 12 weeks, plus routine CRP to gauge inflammatory control. Oral thrush is the most common local side effect; a sugar‑free chlorhexidine rinse usually clears it up. If you notice persistent headache or a rise in fasting glucose, flag it with your gastroenterologist promptly. Remember, the taper-9 mg → 6 mg → 3 mg-over 2‑week intervals is crucial to avoid adrenal suppression. Finally, if you don’t hit remission, escalating to biologics is recommended per NICE guidelines.
Sandra Perkins
November 2, 2025Oh great, another steroid that prteends to be a superhero.
rama andika
November 11, 2025Wow, this “miracle” capsule sounds like the pharma version of a magician’s wand, doesn’t it? They dress it up with fancy enteric coating while the real trick is hoping you don’t notice the hidden side‑effects. And of course, when it inevitably fails, the next step is “the expensive biologics” – as if the industry never runs out of cash grabs. Still, if you’re desperate for a placebo‑like fix, budesonide might keep you afloat for a few months. But don’t be fooled; the “low systemic exposure” claim is just marketing gloss.
Craig Jordan
November 20, 2025Let me play devil’s advocate for a moment and dissect why this whole enthusiasm for budesonide might be misplaced. First, the notion of “local action” is a bit of a myth; even with the enteric coating, a measurable fraction still reaches systemic circulation, especially in patients with altered gut motility. Second, the remission rates quoted-mid‑fifties for Crohn’s and mid‑forties for ulcerative colitis-are hardly groundbreaking when you compare them to the placebo arms of some trials. Third, the design of the studies cited often excludes patients with concomitant medications, which means the real‑world effectiveness could be lower. Fourth, the tapering schedule is more of a bureaucratic hurdle than a scientific necessity; many clinicians simply stop after eight weeks without any adrenal fallout. Fifth, the side‑effect profile, while “milder,” still includes oral candidiasis, headache, and occasional hyperglycemia-issues that can erode quality of life. Sixth, the cost factor, especially in private insurance systems, can make budesonide nearly as pricey as the newer biologics once you factor in monitoring labs and follow‑up visits. Seventh, the guidelines that push budesonide as a first‑line therapy are often influenced by outdated economic models rather than current patient‑centric outcomes. Eighth, the “high first‑pass metabolism” claim ignores genetic polymorphisms in CYP3A4 that can dramatically alter drug levels in certain populations. Ninth, there’s a lack of long‑term data on its safety beyond a year, which is a glaring omission for a chronic disease like IBD. Tenth, the narrative that budesonide “spares” the rest of the body is contradicted by reports of adrenal suppression in a minority of patients after prolonged use. Eleventh, the literature rarely addresses the psychological impact of switching from a “mild” steroid to heavy biologics, which can be demoralizing for patients. Twelfth, many gastroenterologists admit they prescribe budesonide more out of habit than solid evidence. Thirteenth, the table comparing budesonide to prednisone and mesalamine oversimplifies the nuanced decision‑making required for each individual’s disease phenotype. Fourteenth, the article fails to mention the potential drug–drug interactions, especially with common antifungals that inhibit CYP3A4. Finally, the patient anecdotes, while heart‑warming, are anecdotal at best and should not replace robust clinical data. In sum, while budesonide has its place, the hype surrounding it should be tempered with a critical eye.
Wade Developer
November 28, 2025Your critique raises several valid points that merit discussion. While the systemic absorption is indeed not zero, pharmacokinetic studies consistently show it remains below the threshold associated with classic glucocorticoid toxicity. Moreover, the remission figures you cite are derived from randomized controlled trials that accounted for placebo effects, and the differences remain statistically significant. Regarding tapering, current guidelines recommend it precisely to mitigate adrenal suppression, which has been documented in a small subset of long‑term users. Cost considerations vary by health system; in the UK the NHS often covers budesonide, making it a cost‑effective option before moving to biologics. Genetic variability in CYP3A4 metabolism is an emerging field, yet standard dosing remains appropriate for the majority of patients. Finally, long‑term safety data, while still accruing, have not demonstrated any alarming signals beyond those already known for corticosteroids. Thus, while vigilance is essential, budesonide remains a reasonable first‑line choice for appropriately selected IBD cases.
carl wadsworth
December 7, 2025Hold up, Craig. Throwing every possible downside at the wall doesn’t make the drug ineffective. Patients who can’t afford biologics need a bridge, and budesonide actually provides that without the massive immunosuppression risk. If you’re looking for perfect data, you’ll never find it in real‑world practice, but the evidence we have is enough to justify its use as a stepping stone.
Christy Pogue
December 16, 2025Love how you break down the monitoring steps, Kenny! That makes the whole process feel much less intimidating. I’ll definitely keep an eye on my cortisol levels and stick to the taper schedule.
Helena Pearson
December 25, 2025Thanks for the upbeat reminder, Jason! 🙌 Taking the capsule with breakfast is such a simple hack that can make a huge difference. I’ll definitely track my stool count and energy – those little metrics are gold. Keep the positivity flowing! 😊
Neeraj Agarwal
January 2, 2026Just a quick note: “prteends” should be “pretends.” Also, “steroid” is singular, so the article “a” fits better than “another.”
Rose K. Young
January 11, 2026Sure, Kenny, but let’s not pretend this is a cure‑all. Those remission numbers are still modest, and many patients end up on biologics anyway. The “cost‑effective” claim ignores the hidden expenses of monitoring and possible adrenal issues.