SGLT2 Inhibitor Hydration Calculator
Based on clinical guidelines, you should increase your daily fluid intake by 500-1000 mL when starting SGLT2 inhibitors. This calculator helps determine your personalized recommendation based on your individual risk factors.
Your recommended additional fluid intake:
0 mL/day
This is in addition to your regular fluid intake
Important: If you experience dizziness, dark urine, or extreme thirst, stop this calculation and contact your doctor immediately.
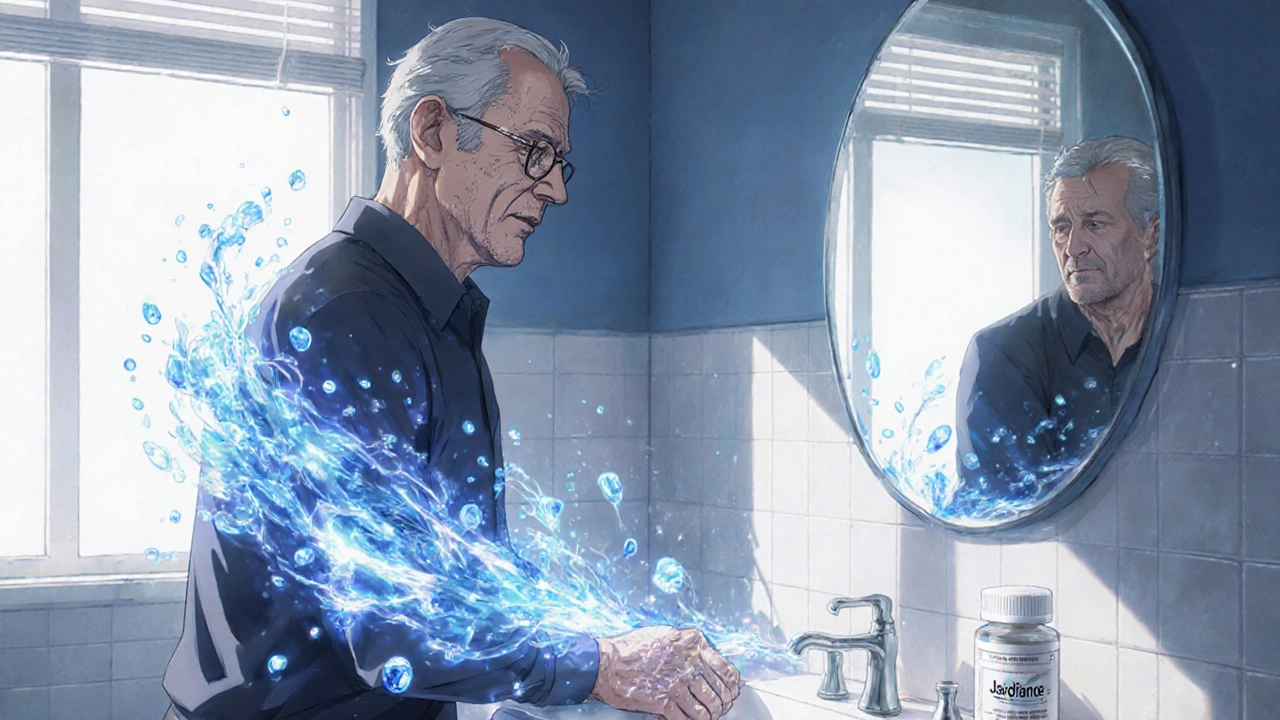
When you start taking an SGLT2 inhibitor like Jardiance, Farxiga, or Invokana, you might notice something unexpected: you’re peeing more than usual. That’s not a bug - it’s the whole point. These drugs were designed to lower blood sugar by making your kidneys flush out excess glucose. But that same mechanism also pulls water and sodium out of your body, creating a natural diuretic effect. For many people, this leads to weight loss, lower blood pressure, and better heart and kidney outcomes. But for others, it brings dizziness, dry mouth, or even fainting spells. Understanding how these side effects connect - and how to manage them - can make all the difference between feeling better and ending up in the ER.
How SGLT2 Inhibitors Work as Diuretics
SGLT2 inhibitors block a specific protein in your kidneys called sodium-glucose cotransporter-2. Normally, this protein reabsorbs about 90% of the glucose your kidneys filter. When it’s blocked, glucose spills into your urine - along with water and sodium. For every gram of glucose excreted, you lose about 3.4 mL of water. That adds up. On average, someone on a 10 mg dose of dapagliflozin loses 200-300 grams of glucose daily. That’s like burning 700-1,000 extra calories a day - without changing your diet or exercise.
But here’s the catch: that glucose doesn’t leave alone. It drags sodium and water with it. This isn’t just a sugar flush - it’s a volume shift. Your body loses 1-1.5 liters of fluid in the first week. That’s why people often drop 2-3 kg quickly after starting the drug. It’s mostly water, not fat. This fluid loss is what makes SGLT2 inhibitors effective for heart failure and high blood pressure. Less fluid means less pressure on your heart and arteries. But it also means your blood volume drops - and that’s where the problems start.
Why Dehydration Happens - And Who’s at Risk
Dehydration from SGLT2 inhibitors isn’t rare. In clinical trials, 1.3% to 2.8% of users reported symptoms like dry mouth, dizziness, or low blood pressure - compared to less than 1% on placebo. But real-world data shows it’s worse. One study found that older adults on canagliflozin had more than double the risk of hospitalization for dehydration than younger patients. Why? Because as we age, our sense of thirst fades. You might not feel thirsty even when your body is running on empty.
High-risk groups include:
- People over 65
- Those with kidney disease (eGFR below 60)
- Patients already taking diuretics (like furosemide or hydrochlorothiazide)
- Anyone on ACE inhibitors, ARBs, or other blood pressure meds
- People who don’t drink enough fluids, especially in hot weather or after exercise
One patient on Reddit shared: "I started Invokana and felt like I was drinking a liter of water every hour - but still had a dry mouth. By day 10, I nearly passed out stepping out of the shower." That’s not an isolated story. Emergency rooms see these cases often. The key is recognizing the early signs: dark yellow urine, fatigue, headache, or feeling lightheaded when standing up. If you notice these, don’t wait. Drink water. Check your blood pressure. Call your doctor.
Dizziness: The Silent Red Flag
Dizziness is the most common complaint tied to SGLT2 inhibitors. Clinical trials report rates between 3.5% and 5.8% - higher than placebo. But here’s what most people don’t tell you: it’s rarely just "feeling woozy." In 63% of cases, it’s orthostatic hypotension - your blood pressure crashes when you stand up. Your systolic pressure drops 20 mmHg or more. That’s enough to make your vision blur, your legs feel weak, or you nearly fall.
It usually hits within the first four weeks. That’s when fluid loss peaks. Risk factors? Age over 75, baseline blood pressure under 130 mmHg, or taking a diuretic. One study found patients on both a diuretic and an SGLT2 inhibitor were more than three times as likely to feel dizzy. The worst part? Many doctors don’t check for it. A survey of endocrinologists found only 42% routinely test orthostatic blood pressure at the first follow-up.
If you’re dizzy after standing, don’t brush it off. Sit down. Drink water. Measure your blood pressure lying down and then again after standing. If your systolic drops by 20 or more, your doctor may need to adjust your meds. Don’t stop the SGLT2 inhibitor without talking to them - the benefits for your heart and kidneys are strong. But you don’t have to live with dizziness.
How Blood Pressure Drops - And Why It’s a Good Thing
Lowering blood pressure is one of the biggest hidden benefits of SGLT2 inhibitors. On average, systolic pressure drops 4-6 mmHg, diastolic 1-2 mmHg. That might sound small, but in heart failure patients, it translates to a 17% lower risk of cardiovascular death. The effect isn’t just from losing fluid. These drugs also improve artery flexibility, reduce stiffness, and calm overactive stress hormones in your kidneys. That’s why they work even in people without diabetes.
Empagliflozin lowered blood pressure in heart failure patients regardless of whether they had high blood pressure to begin with. Dapagliflozin did the same in the DAPA-HF trial. This isn’t a fluke - it’s built into the drug’s design. The same mechanism that flushes out glucose also reduces pressure inside your kidneys, protecting them long-term. That’s why guidelines now recommend SGLT2 inhibitors for heart failure even if you’re not diabetic.
But here’s the balance: too much pressure drop can be dangerous. If your blood pressure was already low - say, below 110 mmHg systolic - you’re at higher risk for fainting or falls. One study found patients with baseline SBP under 120 had more than three times the risk of symptomatic hypotension. That’s why doctors are now told to check your blood pressure before starting these drugs. If it’s already low, they might start with a lower dose or delay treatment until you’re more stable.
How to Stay Safe While Taking SGLT2 Inhibitors
You don’t have to avoid these drugs because of side effects. But you do need to be smart about them. Here’s what works:
- Start low, go slow. If you’re over 65 or on other blood pressure meds, ask for the lowest available dose - like 10 mg of empagliflozin instead of 25 mg.
- Drink more water. Add 500-1,000 mL (about 2-4 cups) of fluid daily, especially in heat or after exercise. Don’t wait until you’re thirsty.
- Check your blood pressure. Take readings lying down and standing up during the first week. If your systolic drops 20 mmHg or more when standing, tell your doctor.
- Monitor your weight. A sudden drop of more than 2 kg in a week could mean too much fluid loss. Weigh yourself daily for the first month.
- Pause during illness. If you have vomiting, diarrhea, or a fever, hold the medication until you’re rehydrated. These drugs don’t work well when you’re already dehydrated.
- Don’t mix with other diuretics unless supervised. If you’re on a water pill, your doctor may need to reduce the dose by 25-50%.
Many patients who feel dizzy at first end up feeling better after a few weeks. Their bodies adjust. But if dizziness lasts beyond four weeks, or if you feel faint, don’t ignore it. Your doctor can adjust your treatment plan without giving up the benefits.

When to Call Your Doctor
Not every side effect needs an emergency room visit - but some do. Call your doctor right away if you experience:
- Feeling faint or passing out
- Extreme thirst with very dark urine
- Confusion, rapid heartbeat, or shallow breathing
- Swelling in your legs or ankles that gets worse
- Urine output drops suddenly (less than 300 mL in 24 hours)
These could signal severe dehydration, kidney stress, or low blood pressure that needs immediate attention. Don’t wait. Most of these issues are preventable - but only if you speak up early.
The Bigger Picture: Benefits vs. Risks
It’s easy to focus on side effects. But remember: SGLT2 inhibitors have changed the game for heart failure and kidney disease. In the EMPEROR-Reduced trial, empagliflozin cut the risk of cardiovascular death by 38% in heart failure patients. In the DAPA-HF trial, dapagliflozin reduced hospitalizations for heart failure by 30%. These aren’t small wins - they’re life-saving.
For every 100 people treated with dapagliflozin for 18 months, about 6 lives are saved. The risk of dizziness? Around 4%. That’s a trade-off most patients and doctors accept. The key is managing the risk, not avoiding the drug. With proper monitoring, most people tolerate these medications well. The goal isn’t to stop them - it’s to use them safely.
Can SGLT2 inhibitors cause dehydration even if I drink enough water?
Yes. Even if you drink plenty of water, SGLT2 inhibitors force your kidneys to excrete more fluid than usual. This isn’t just about intake - it’s about how your body holds onto water. The drugs change kidney function, so your body loses more fluid than normal, even with good hydration. That’s why doctors recommend increasing fluid intake by 500-1,000 mL daily when starting the medication - to compensate for this built-in diuretic effect.
Is dizziness from SGLT2 inhibitors permanent?
No. For most people, dizziness improves within 2-4 weeks as the body adjusts to lower fluid volume. It’s usually tied to the initial fluid loss and drop in blood pressure. If it persists beyond a month, your doctor may check for other causes like anemia, low sodium, or interactions with other medications. In many cases, reducing the dose of the SGLT2 inhibitor or adjusting other blood pressure meds helps - without losing the heart and kidney benefits.
Should I stop SGLT2 inhibitors if I feel dizzy?
Don’t stop on your own. Dizziness is common at first, and stopping the drug means losing its protective effects on your heart and kidneys. Instead, sit down, drink water, and measure your blood pressure. If your systolic drops more than 20 mmHg when standing, call your doctor. They may lower your dose, reduce other diuretics, or delay the next dose - but they won’t necessarily stop the SGLT2 inhibitor. The benefits usually outweigh the side effects in appropriate patients.
Do SGLT2 inhibitors work the same in people without diabetes?
Yes. In fact, their heart and kidney benefits are often stronger in people without diabetes. The diuretic and blood pressure-lowering effects come from blocking glucose and sodium reabsorption in the kidneys - not from lowering blood sugar. That’s why guidelines now recommend them for heart failure with reduced ejection fraction (HFrEF) regardless of diabetes status. Clinical trials like DAPA-HF and EMPEROR-Reduced included many non-diabetic patients and still showed major benefits.
Can I take SGLT2 inhibitors if I have low blood pressure?
It depends. If your systolic blood pressure is below 110 mmHg, you’re at higher risk for dizziness, fainting, or falls. Many doctors will delay starting the drug until your pressure stabilizes. If you’re already on one and your pressure drops too low, your doctor may reduce the dose or temporarily stop it. But if your low blood pressure is stable and you’re not symptomatic, you may still be a candidate - especially if you have heart failure or kidney disease. The decision is individualized.
What Comes Next
As generic versions of SGLT2 inhibitors become more widely available, more people will start taking them - including those in primary care settings where monitoring might be less frequent. That makes patient education even more critical. If you’re on one of these drugs, know the signs of dehydration and dizziness. Drink water. Track your weight. Check your blood pressure. Talk to your doctor before making any changes. These medications are powerful tools - but they work best when you’re informed, not afraid.





9 Comments
Jeff Moeller
November 19, 2025Been on Jardiance for 8 months. Lost 12 lbs in the first month. Mostly water. Still feel like a ghost when I stand up too fast. Drank a gallon of water today and still felt dehydrated. My body just doesn't hold onto shit anymore. Not complaining. Just saying it's wild.
Herbert Scheffknecht
November 21, 2025Think about it like this. Your kidneys are basically running a 24/7 detox spa for your blood. SGLT2 inhibitors? They're the bouncer kicking out glucose like it's a VIP who forgot his ID. But in doing that, they're also tossing out sodium, water, electrolytes, your dignity, your will to live on hot days. It's not medicine. It's metabolic civil war. And we're just the collateral.
Jessica Engelhardt
November 22, 2025They say it's for heart health but I swear Big Pharma just wants us to pee more so we buy more bottled water and electrolyte powders. Also why is this only approved in rich countries? Third world folks don't even have clean toilets let alone access to this. It's all a scam. You think you're getting healthier but you're just funding another shareholder dividend.
Martin Rodrigue
November 24, 2025While the clinical data presented is largely accurate, I must emphasize that the incidence of orthostatic hypotension in the DAPA-HF trial was 4.7% versus 2.1% in the placebo group, with a hazard ratio of 2.18 (95% CI 1.72–2.76). The recommendation to increase fluid intake by 500–1000 mL daily is reasonable, though it should be individualized based on renal function and concomitant medications. Furthermore, the term 'natural diuretic effect' is misleading; pharmacologically, this is a deliberate osmotic diuresis.
Sherri Naslund
November 25, 2025ok but what if you just dont drink water at all?? like i dont care if i pee 10x a day i just wanna be done with this diabetes thing. my doctor said drink more but i dont like water. i like coke zero. is that bad?? i mean its zero sugar so its healthy right??
Ashley Miller
November 26, 2025They told me this was for diabetes. Then I found out it’s used for heart failure. Then I read it works even if you don’t have diabetes. Now I’m wondering… is this just a fancy water pill they repackaged as a miracle drug? Who decided we needed another way to make people pee? Who profits? Who’s watching the labs? I’m not mad. I’m just… suspicious.
Lauren Hale
November 28, 2025For anyone new to this: the dizziness gets better. I was terrified the first week. Felt like I was going to pass out every time I stood up. I started drinking 2 liters a day, weighed myself every morning, and sat down for 30 seconds before standing. After 3 weeks, the fog lifted. I lost 8 pounds of water weight, my BP dropped from 145 to 128, and my A1c went from 8.2 to 6.9. It’s not magic. It’s science. But you have to treat it like a tool, not a cure-all. Listen to your body. Don’t ignore thirst. And if you’re over 65? Start low. Like, really low.
Greg Knight
November 29, 2025I’ve helped over 40 patients start SGLT2 inhibitors and here’s the thing: the biggest mistake isn’t taking the pill - it’s not preparing for it. People think, ‘Oh, I’ll just take it like my metformin.’ No. This is different. You need a plan. Water schedule. BP log. Weight tracker. Tell your family so they know why you’re suddenly peeing every 20 minutes. I had one guy who almost fainted at his kid’s soccer game because he didn’t drink before leaving the house. Now he carries a bottle in his pocket. You don’t need to be scared. You just need to be ready. This drug saves lives. But only if you show up for it.
rachna jafri
November 30, 2025India has 100 million diabetics. We don’t need fancy American drugs. We need clean water, walking paths, and less sugar in our chai. My uncle took this and got dizzy. He stopped. He walks 5 km every morning now. His sugar is better. His BP is better. His spirit is better. You think science is in a pill? Nah. Science is in sweat. In tradition. In community. This drug is a Band-Aid on a broken system. But hey, if you wanna pay $500 a month to pee more, go ahead. I’ll be over here with my neem leaves and my chai without sugar.