Constipation isn’t just about not going to the bathroom often-it’s about struggling to pass stool, feeling full even after going, or needing to strain for minutes without results. If you’re having fewer than three bowel movements a week and it’s been going on for weeks or months, you’re not alone. About one in three people in clinical settings deal with this daily. In the U.S., over 2.5 million people visit doctors each year just for constipation. It’s not a minor annoyance. It’s a sign your body’s system is out of sync.
Why Does Constipation Happen?
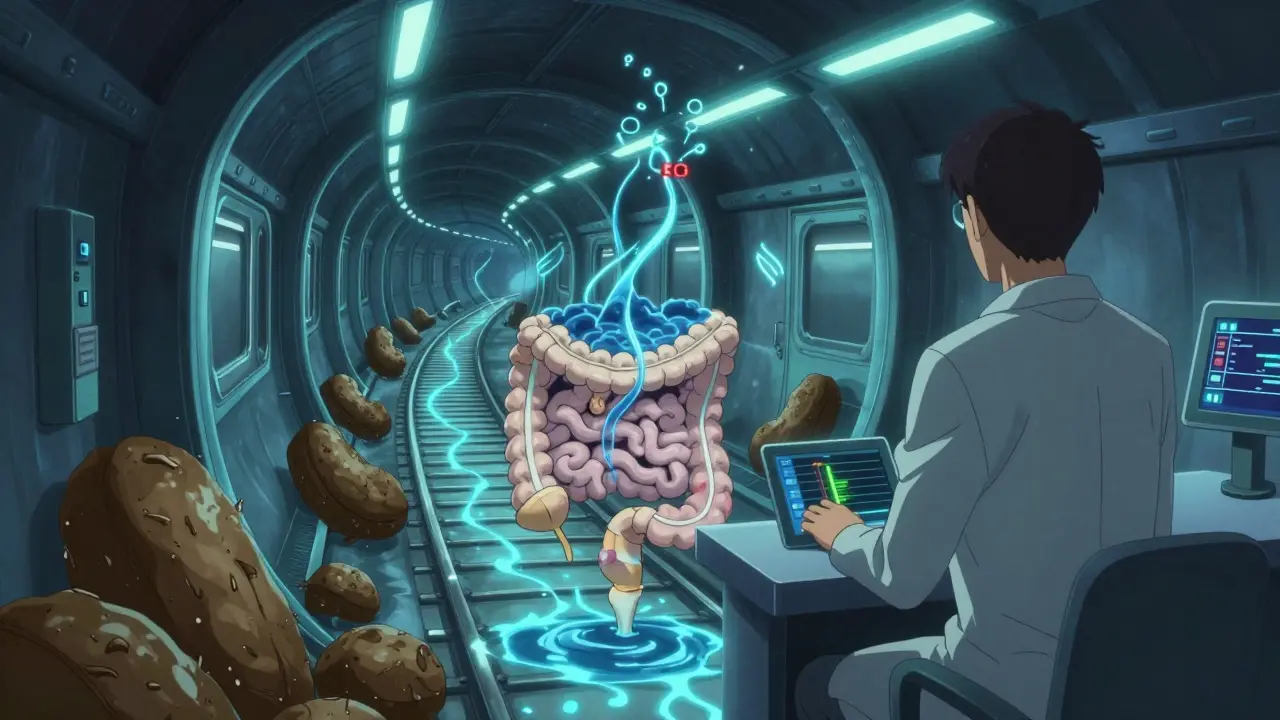
It starts with how your colon works. After food moves through your stomach and small intestine, waste enters the colon. Normally, the colon absorbs water and pushes stool out within 24 to 72 hours. But when that process slows down, too much water gets pulled out. The stool becomes hard, dry, and stubborn. That’s constipation.There are two main types of causes: primary (functional) and secondary (due to something else). Primary constipation happens without a clear disease. It’s often from not eating enough fiber, drinking too little water, or sitting too much. The average American eats only 15 grams of fiber a day-but experts recommend 25 to 30 grams. That’s a big gap.
Secondary causes are trickier. Medications are a major player. Opioids cause constipation in up to 95% of long-term users. Calcium channel blockers for high blood pressure, tricyclic antidepressants, and even iron supplements can slow things down. Medical conditions like diabetes (affecting nearly 60% of patients), hypothyroidism, Parkinson’s disease, and multiple sclerosis also interfere with nerve signals that control bowel movement.
Women are more likely to experience it-67% of chronic constipation patients are female. Age matters too. After 60, the risk goes up by 1.5% every year. If you’ve had a stroke, suffer from COPD, or have kidney disease, your chances go up even more.
Types of Constipation: Not All Are the Same
Not everyone with constipation has the same problem. Doctors classify it into four main types:- Normal transit constipation (60% of cases): Your colon moves stool at a normal speed, but you still feel like you haven’t emptied fully. Straining, hard stools, and bloating are common. This is often tied to diet and habits.
- Slow transit constipation (15-30%): Stool moves too slowly through the colon-sometimes taking over 72 hours. This can be genetic or linked to nerve damage.
- Defecatory disorders (20-50%): Your pelvic floor muscles don’t relax properly when you try to go. You might push hard but nothing comes out. This is often misdiagnosed as simple constipation.
- Refractory constipation (15-20%): Nothing seems to work. You’ve tried fiber, water, and laxatives, and symptoms stick around.
Diagnosing the right type matters. For defecatory disorders, doctors use a balloon expulsion test-filling a small balloon in the rectum with 50 mL of water and seeing if you can push it out in under a minute. If you can’t, it’s likely a muscle coordination issue, not a slow colon.
Laxatives: What Works and What Doesn’t
Laxatives are the go-to fix for many, but not all are created equal. There are five main types:- Bulk-forming laxatives (psyllium, methylcellulose): These soak up water and swell to make stool bigger and softer. They work well for normal transit constipation-but only if you drink enough water. If you don’t, they can make things worse by causing blockages. Take at least 8 ounces of water with each dose.
- Osmotic laxatives (PEG 3350, lactulose, magnesium hydroxide): These pull water into the colon. PEG 3350 (MiraLAX) is the first-line choice. It’s effective in 65-75% of people, gentle on the gut, and safe for long-term use. Dose: 17 grams daily.
- Stimulant laxatives (senna, bisacodyl): These crank up colon contractions. They work fast-usually within 6 to 12 hours. But using them longer than 2 to 3 weeks can damage your colon’s natural rhythm. Doctors warn against using them for more than 12 weeks. Risk: cathartic colon, where the colon loses its ability to move stool on its own.
- Stool softeners (docusate sodium): These are popular, but studies show they’re barely better than a placebo. Don’t rely on them alone.
- Prescription options (lubiprostone, linaclotide, plecanatide): For stubborn cases, these drugs trigger fluid secretion in the gut. Linaclotide (Linzess) helps 45-60% of patients. But they’re expensive-up to $500 a month without insurance.
Real-world data shows most people try three or more laxatives before finding what works. The average time to effective relief? Nearly 15 months.
Long-Term Management: Beyond Pills
Laxatives can help, but they’re not a cure. True long-term relief comes from changing your daily habits.1. Eat more fiber-but slowly. Jumping from 15g to 30g overnight will make you bloated. Add 5g every 3 to 4 days. Focus on soluble fiber: oats, beans, apples, chia seeds, and flax. It holds water and softens stool better than insoluble fiber like bran.
2. Drink water with every meal. For every 5g of extra fiber you add, drink an extra 250-500 mL of water. Most people forget this. That’s why fiber sometimes backfires.
3. Train your body to go. Sit on the toilet for 10-15 minutes after breakfast. That’s when your gastrocolic reflex is strongest-your body naturally wants to move after eating. Don’t rush. Don’t scroll. Just sit.
4. Use a footstool. Elevating your feet so your knees are higher than your hips (about a 35-degree angle) helps straighten your rectum. Studies show this reduces straining by 60%. A simple stool under your feet does wonders.
5. Try biofeedback. If you’re straining with no result, you might have a pelvic floor disorder. Biofeedback therapy retrains your muscles using sensors and visual feedback. After 6 to 8 weekly sessions, 70-80% of patients see major improvement.
6. Know when to worry. If you lose weight without trying, see blood in your stool, or your bowel habits change for more than 6 weeks, get checked. These are alarm signs that could point to something serious-like colon cancer.
What Doesn’t Work (and Why)
Many people fall into traps that make constipation worse:- Using stimulant laxatives for months thinking they’re harmless. They’re not. Long-term use damages your colon’s natural movement.
- Believing that “natural” means safe. Senna tea, cascara, and aloe vera are stimulants too. Same risks.
- Skipping water because you’re “not thirsty.” Your body doesn’t always tell you when it needs more fluid.
- Waiting until you’re “really backed up” to act. Prevention beats cure every time.
One patient, a 52-year-old woman, struggled for years. She tried everything-supplements, enemas, prescriptions. Nothing stuck. Then she started: 25g of psyllium daily, 2 liters of water, coffee every morning (it triggers the gut reflex), and 10 minutes of squatting on a footstool after breakfast. Within 8 weeks, she was going regularly without any laxatives.

What’s New in Constipation Care
Science is catching up. In 2023, the FDA approved tenapanor (Ibsrela), a new drug that blocks sodium absorption in the gut, helping fluid stay in the colon. It’s for irritable bowel syndrome with constipation, but it’s a sign of progress.Researchers are also looking at gut bacteria. The Microbiome Constipation Project found that people with chronic constipation often have less of a specific bacteria called Bacteroides uniformis. Future treatments might include targeted probiotics instead of pills.
And there’s tech. At Augusta University, scientists are testing smartphone apps that use motion sensors to detect if you’re properly evacuating. Early results show 85% accuracy in spotting pelvic floor dysfunction-no expensive machines needed.
By 2030, constipation is expected to rise 12% globally, mostly because of aging populations and rising diabetes. That means we need better, smarter, long-term solutions-not just quick fixes.
Final Thoughts: It’s Manageable
Constipation isn’t a life sentence. It’s a signal. It’s telling you something’s off-diet, hydration, movement, or even your nervous system. Most people can fix it without drugs. Start with fiber, water, and posture. Give it 4 to 6 weeks. If it doesn’t improve, see a doctor who understands the difference between a slow colon and a faulty pelvic floor.Don’t accept daily discomfort as normal. You don’t have to live with it. And you don’t have to rely on laxatives forever. With the right approach, your body can learn to work the way it should.
How often is it normal to have a bowel movement?
There’s no single “normal.” Going anywhere from three times a day to three times a week is considered within the healthy range. What matters more is consistency and comfort. If you’re suddenly going less than three times a week, straining often, or feeling incomplete after going, that’s constipation-even if you’re not “blocked.”
Can constipation be caused by stress?
Yes. Stress affects your gut-brain axis-the communication line between your brain and digestive system. When you’re anxious or under pressure, your body may slow digestion, reduce gut motility, and increase water absorption in the colon. This can lead to harder stools and fewer bowel movements. Managing stress through breathing, walking, or mindfulness can help improve symptoms.
Is it safe to use laxatives every day?
Osmotic laxatives like PEG 3350 are generally safe for daily use over months or even years. Stimulant laxatives like senna or bisacodyl are not. Using them daily for more than 2-3 weeks can damage your colon’s natural ability to contract, leading to dependency and worsening constipation. Always start with the mildest option and only use stimulants briefly under medical guidance.
Why does constipation get worse with age?
As we age, muscles in the colon and pelvic floor weaken. Nerve signals slow down. Medications become more common-especially for blood pressure, pain, or depression-all of which can cause constipation. Many older adults also drink less water and move less. It’s not inevitable, but it’s common. The good news? Lifestyle changes still work, even in your 70s and 80s.
Should I take probiotics for constipation?
Some strains show promise. Studies suggest Bifidobacterium lactis and Lactobacillus acidophilus may help soften stool and increase frequency slightly. But results are mixed. Probiotics aren’t a first-line treatment. They might help as a supplement if you’re already doing fiber, water, and posture right. Don’t expect miracles.
When should I see a doctor for constipation?
See a doctor if you’ve had symptoms for more than 3 weeks despite lifestyle changes, or if you have warning signs: unexplained weight loss, rectal bleeding, vomiting, severe abdominal pain, or a family history of colon cancer. Also, if you’re over 50 and your bowel habits have changed, get checked. Early detection of underlying issues can be life-saving.
Can exercise help with constipation?
Yes. Walking, yoga, swimming, or even light stretching helps stimulate the muscles in your abdomen and colon. One study found that just 30 minutes of daily walking improved bowel frequency in 70% of people with chronic constipation. You don’t need to run a marathon-just move more than you sit.






10 Comments
Chelsea Harton
January 16, 2026i just eat salad and call it a day lol
Christina Bilotti
January 17, 2026Oh wow, another ‘just drink more water’ miracle cure from someone who clearly thinks the colon is a stubborn toddler. Did you also forget to mention that your ‘fiber’ is a sad kale chip you ate once in 2021? Please. The real issue is that people treat their guts like a broken toaster they’ll fix with duct tape.
And don’t even get me started on laxatives. You think MiraLAX is a ‘gentle’ solution? It’s just the pharmaceutical version of whispering sweet nothings to your colon until it gives in. Meanwhile, people are popping senna like candy because ‘it’s natural’-as if ‘natural’ means ‘safe’ and not ‘historically used to purge witches.’
And yet, no one talks about the real villain: sitting. You sit at a desk, you sit in a car, you sit watching Netflix until your pelvis forgets it has a purpose. Then you wonder why your body won’t cooperate. It’s not magic. It’s physics. Gravity. Muscles. And yes, maybe your posture is worse than your credit score.
Footstools? Groundbreaking. I’m sure the Romans didn’t have them either. And biofeedback? You’re telling me we need sensors to teach people how to poop? That’s not medicine-that’s a TED Talk with a $400 co-pay.
And don’t even mention probiotics. ‘Some strains show promise’? That’s not science, that’s a marketing email from a guy who sells gummies shaped like poop emojis.
brooke wright
January 18, 2026wait so if i’m 35 and my mom had colon cancer and i’ve been going every 4 days for 3 months and i use a footstool but still feel like i’m trying to push out a brick… am i just not trying hard enough? or is this my body telling me something? i’m scared
vivek kumar
January 19, 2026Interesting article, but the data is incomplete. You cite 67% of chronic constipation patients are female, yet you provide no breakdown of hormonal influence, menstrual cycle correlation, or estrogen-progesterone impact on colonic motility. Also, the 1.5% annual risk increase after 60-what’s the baseline? Is this relative or absolute? Where’s the confidence interval? Without this, the statistics are just noise.
Furthermore, the claim that ‘fiber works better if added slowly’ is empirically true, but the mechanism is rarely explained. Soluble fiber forms a gel, which increases stool bulk and water retention. Insoluble fiber adds bulk but doesn’t hydrate. Why do so many people confuse the two? Because supplement labels don’t differentiate. That’s not consumer education-that’s negligence.
And you mention tenapanor. Good. But you don’t mention its mechanism: it inhibits NHE3, reducing sodium absorption, which increases intraluminal fluid. This is a novel pathway. Why not compare it to lubiprostone’s ClC-2 activation? Why not discuss the gut-brain axis modulation via vagal stimulation? This reads like a blog post, not a clinical review.
And where’s the data on cultural differences? In India, we use triphala, psyllium, and warm water with lemon daily. Constipation rates are lower. Is that diet? Lifestyle? Or something else? You mention India’s population growth but ignore its traditional remedies. That’s a missed opportunity.
Finally, the ‘no laxatives for more than 12 weeks’ rule-where’s the evidence? Some patients need long-term osmotic agents. Denying them is not medicine-it’s dogma. Evidence-based doesn’t mean ‘one-size-fits-all.’
Nick Cole
January 19, 2026Bro, I was in the same boat. Used senna for 8 months. Felt like my insides were on strike. Then I started the footstool, 25g psyllium, and made myself sit on the toilet after coffee every morning-even if I didn’t feel like it. No laxatives. No supplements. Just time and posture. 6 weeks later, I’m going daily without thinking about it. It’s not magic. It’s consistency.
And yeah, stress messes with you. I used to get backed up every time I had a big deadline. Now I take 10-minute walks before I sit down to work. Doesn’t fix everything, but it helps. You don’t need a PhD to fix this. Just patience and a little discipline.
Riya Katyal
January 21, 2026Oh sweetie, you think you’re the first person to tell women to ‘sit on the toilet after breakfast’? I’ve been told that since I was 14. By my mom. By my gyno. By my yoga instructor. By my aunt who runs a tea shop. We get it. We’re not lazy. We’re just tired of being told our colon is a garden that needs ‘tending’ while men get to be ‘busy’ and ‘stressed’ and no one asks if they’re pooping.
And don’t even get me started on ‘natural’ remedies. Senna tea? That’s just a fancy way of saying ‘I’m poisoning my nerves so I can feel something.’ You don’t get a medal for using ‘herbs.’ You get a broken colon.
Henry Ip
January 22, 2026Love this breakdown. The footstool tip alone changed my life. I used to think I was just ‘slow’-turns out I was sitting like a statue. Now I have a $12 plastic stool under my feet. No more straining. No more shame. Just… normal. Also, the part about not waiting until you’re ‘really backed up’? Game changer. I started adding fiber before I even felt the need. It’s like brushing your teeth-you don’t wait for a cavity.
And yes, probiotics are overhyped. But if you’re already doing the basics? Might as well try. I take a Bifidobacterium strain with my morning oatmeal. No miracles. But no side effects either. Worth a shot.
waneta rozwan
January 24, 2026OMG I’m crying. I’ve been dealing with this for 12 years. I’ve tried everything. Enemas. Colonics. Prescription drugs that made me vomit. I thought I was broken. I thought I was weird. I thought I’d never have a ‘normal’ day again. And now I’m reading this and realizing… it’s not me. It’s the system. The sitting. The water. The fiber. The damn posture. I’m going to try the footstool. I’m going to drink water before coffee. I’m going to sit for 10 minutes after breakfast even if I hate it. I’m not giving up anymore. Thank you. I needed this.
Nicholas Gabriel
January 25, 2026Hey, just wanted to add something-don’t forget the role of circadian rhythm! Your colon has its own clock. It’s most active in the morning, right after you eat. That’s why the gastrocolic reflex kicks in. If you skip breakfast, or eat it while scrolling on your phone, or stand up immediately after, you’re basically yelling at your colon: ‘Hey, I don’t care about you!’ It’s not lazy-it’s ignored.
Also, people think ‘fiber’ means bran cereal. No. Bran is insoluble. It’s like adding gravel to your stool. Soluble fiber-chia, flax, oats, apples-is the real MVP. It turns into a gel. It’s like a sponge for water. That’s what softens things. And yes, you need water. Always. Always. Always. One gram of fiber needs 15-20 mL of water. That’s not optional. That’s physics.
And biofeedback? It’s not ‘weird.’ It’s like physical therapy for your butt. You’re retraining muscles that forgot how to relax. It’s not embarrassing. It’s smart. And if you’re over 50, or had a baby, or sit all day? You’re probably a candidate. Don’t be shy. Ask your doctor. Seriously.
Cheryl Griffith
January 27, 2026I’m 68 and I’ve been constipated since my hip surgery. I thought it was just ‘old age.’ But I tried the footstool, added chia seeds to my yogurt, and started walking after dinner. No laxatives. Just movement and water. It took 5 weeks. But now I go every day. No pain. No stress. I didn’t know it could be this simple. I wish I’d known this 10 years ago.