Azathioprine-Allopurinol Interaction Calculator
Dosage Adjustment Calculator
This tool calculates proper dosage adjustments when azathioprine and allopurinol must be used together under specialist supervision. Remember: This combination is extremely dangerous without precise monitoring and is only appropriate for 25-30% of patients who are "thiopurine shunters."
Combining allopurinol and azathioprine might seem like a simple fix for someone with both gout and an autoimmune condition-but it’s one of the most dangerous drug combinations in medicine. This isn’t a theoretical risk. It’s caused real deaths, hospitalizations, and life-threatening drops in blood cell counts. If you’re taking azathioprine for Crohn’s disease, ulcerative colitis, rheumatoid arthritis, or after an organ transplant, and your doctor prescribes allopurinol for gout, you need to know exactly what’s at stake.
What Happens When These Two Drugs Meet?
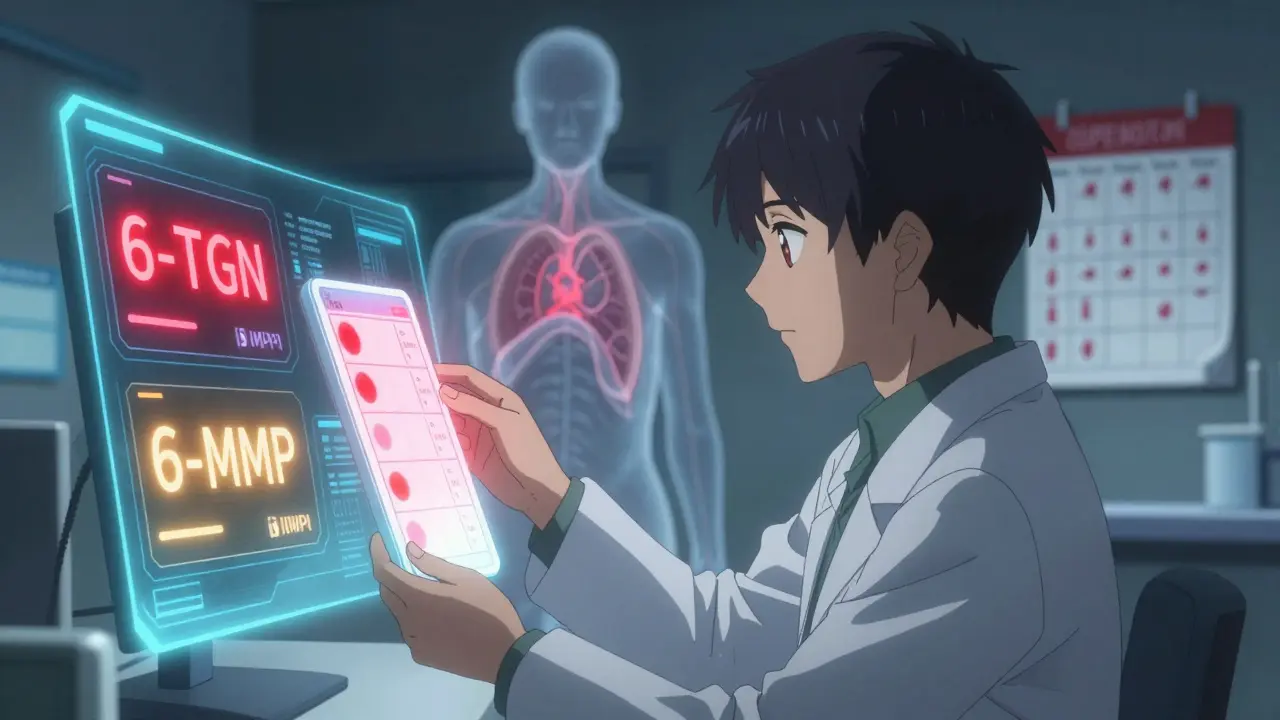
Allopurinol lowers uric acid to treat gout. Azathioprine suppresses the immune system. On the surface, they do different jobs. But inside your body, they collide in a way that can shut down your bone marrow. Azathioprine breaks down into 6-mercaptopurine (6-MP), which your liver turns into two types of metabolites: one that fights inflammation (6-TGN), and another that can damage your liver (6-MMP). Normally, xanthine oxidase, an enzyme, helps break down 6-MP into harmless waste. Allopurinol blocks that enzyme. When that happens, your body can’t clear 6-MP properly. Instead, it dumps more of it into the 6-TGN pathway, flooding your system with active immune-suppressing compounds. The result? Your white blood cells, platelets, and red blood cells stop being made. In severe cases, white blood cell counts plunge below 1,000 per mm³ (normal is 4,000-11,000). Neutrophils-your frontline infection fighters-can drop below 500. Platelets may fall under 20,000, putting you at risk of uncontrolled bleeding. Hemoglobin can crash to 3.7 g/dL, causing extreme fatigue, dizziness, and heart strain. This isn’t rare. In a 1996 case report, a 63-year-old heart transplant patient on azathioprine was given allopurinol for wrist pain thought to be gout. Within weeks, he developed pancytopenia. He needed blood transfusions and intensive care. The hospital bill? Over $25,000 in today’s money. He survived. Many don’t.Why This Interaction Is So Deadly
The danger isn’t just about too much drug. It’s about how your body handles it. When allopurinol blocks xanthine oxidase, 6-MP gets redirected. You get up to four times more 6-TGN in your blood. That’s not a little extra-it’s a toxic overload. These metabolites get stuck in your DNA, stopping blood cells from dividing. At the same time, they trigger white blood cells to self-destruct. It’s a one-two punch: fewer cells made, more cells killed. The FDA requires a black box warning on azathioprine labels-the strongest possible alert-for this interaction. The European Medicines Agency says the same. Yet, it still happens. Why? Because many doctors don’t know. Or they assume the patient’s gout is minor. Or they don’t check what else the patient is taking. A 2021 survey of U.S. gastroenterologists found only 32% had ever used this combination. Most avoided it. Those who did? They worked in academic hospitals with pharmacists trained in thiopurine metabolism. This isn’t a primary care decision.When Is It Ever Safe to Combine Them?
There’s one exception-and it’s narrow, complex, and only for specialists. About 25-30% of people on azathioprine are “thiopurine shunters.” Their bodies turn too much of the drug into 6-MMP, which harms the liver instead of helping the gut. These patients often can’t tolerate standard doses. They get sick from liver damage, not from their disease. For them, adding low-dose allopurinol can be life-changing. By blocking xanthine oxidase, allopurinol forces the body to use the 6-TGN pathway instead. That means better control of Crohn’s or colitis, less liver damage, and fewer steroids. A 2018 study of 73 IBD patients showed that when allopurinol was added at 50-100 mg daily and azathioprine was cut to 25% of the normal dose, 53% went into steroid-free remission. Over 80% were able to stop steroids completely. Their inflammation markers dropped. Their quality of life improved. But here’s the catch: this only works with extreme precision.- Azathioprine must be reduced to 0.5-0.75 mg per kg per day (not the usual 2-2.5 mg/kg).
- Allopurinol starts at 100 mg daily.
- Complete blood counts must be checked weekly for the first month, then every two weeks for two months, then monthly.
- Thiopurine metabolite levels (6-TGN and 6-MMP) must be tested before and during treatment.
- Therapeutic 6-TGN range: 230-450 pmol/8×10⁸ RBCs. 6-MMP must stay below 5,700 pmol/8×10⁸ RBCs.
What Should You Do If You’re on Azathioprine?
If you’re taking azathioprine, here’s your action plan:- Check your medication list. Do you take allopurinol? If yes, don’t stop it-call your doctor immediately.
- If you have gout symptoms (swollen joint, redness, intense pain), tell your doctor you’re on azathioprine. Ask: “Is there a safer option than allopurinol?”
- Ask for a referral to a specialist if you’re being considered for this combination. Don’t accept a prescription without a metabolite test.
- Know the warning signs: unexplained bruising, fever, sore throat, extreme tiredness, nosebleeds, or pale skin. Go to the ER if you have any of these.
Why This Interaction Still Happens
The problem isn’t just lack of knowledge. It’s fragmented care. A patient sees a rheumatologist for arthritis, a gastroenterologist for IBD, and a primary care doctor for gout. None of them talk to each other. The primary care doctor sees “gout” and writes “allopurinol.” They don’t see the azathioprine on file. One study found that over half of patients on azathioprine had no mention of this interaction in their electronic records. Prescribers didn’t get alerts. No one asked. That’s why Medsafe (New Zealand’s drug safety agency) says: “When azathioprine is initiated, the prescriber should check that the patient is not taking allopurinol.” That’s not a suggestion. It’s a safety rule.
What’s Changing in 2026?
New guidelines from the American College of Gastroenterology now conditionally recommend this combination for thiopurine shunters with refractory IBD. But they stress: “Only under expert supervision.” Research is moving toward precision dosing. The TAILOR-IBD trial (NCT04256590) is testing whether tailoring doses based on metabolite levels can make this safer. Early results show 68% remission rates at 12 months with careful monitoring. Genetic testing for TPMT (thiopurine methyltransferase) is also becoming more common. About 10% of people have low or intermediate TPMT activity, making them even more vulnerable to this interaction. Testing for this before starting azathioprine could prevent disaster. Still, the bottom line hasn’t changed: allopurinol and azathioprine should not be taken together unless under the direct care of a specialist who monitors blood and metabolites weekly.What If You’re Already Taking Both?
If you’re currently on both drugs, don’t panic. But do this now:- Call your pharmacy. Ask if they flagged this interaction.
- Ask your doctor for your latest complete blood count and thiopurine metabolite results.
- If you haven’t had a blood test in the last 30 days, schedule one immediately.
- If you’re not under the care of a gastroenterologist or transplant specialist, ask for a referral.
Can I take allopurinol and azathioprine together safely?
Only under strict medical supervision by a specialist-typically a gastroenterologist or transplant pharmacist-with regular blood tests and metabolite monitoring. Even then, azathioprine must be reduced to 25-33% of the normal dose. For most people, the risk outweighs the benefit. Avoid this combination unless you’re in a specialized care program.
What are the signs of bone marrow suppression from this interaction?
Watch for unexplained bruising or bleeding, frequent infections, fever, extreme fatigue, pale skin, shortness of breath, or nosebleeds. These can appear within days or weeks of starting allopurinol. If you notice any of these, stop the medication and go to the emergency room immediately.
Is there a safer alternative to allopurinol for gout?
Yes. Febuxostat is a common alternative that lowers uric acid without blocking xanthine oxidase. Colchicine can treat gout flares. Pegloticase is an IV option for severe, treatment-resistant gout. Always discuss alternatives with your doctor if you’re on azathioprine.
How often should blood tests be done if I’m on both drugs?
If this combination is absolutely necessary, blood counts must be checked weekly for the first month, every two weeks for the next two months, and then monthly. Thiopurine metabolite levels (6-TGN and 6-MMP) should be tested before starting and every 3-6 months after stabilization. This level of monitoring is not possible in general practice.
Why do some doctors still prescribe this combination?
Some specialists use it in carefully selected IBD patients who are “thiopurine shunters”-those whose bodies turn azathioprine into liver-toxic metabolites instead of anti-inflammatory ones. In these rare cases, adding low-dose allopurinol can redirect the drug’s effect and improve outcomes. But this requires expertise, testing, and monitoring that most doctors don’t have.
Can genetic testing help prevent this interaction?
Yes. Testing for TPMT gene activity can identify people who metabolize azathioprine more slowly, putting them at higher risk for toxicity. About 10% of people have intermediate TPMT activity. While this doesn’t eliminate the risk of the allopurinol interaction, it helps identify who needs the closest monitoring. Many specialists now test TPMT before starting azathioprine.





15 Comments
laura Drever
January 14, 2026lol who even reads this shit anymore? allopurinol + azathioprine = bad. got it. moving on.
Diana Campos Ortiz
January 14, 2026i had a cousin on both of these. she got pancytopenia. spent 3 weeks in the hospital. they didn't even check her meds properly.
if you're on azathioprine, just ask your doctor: 'is this safe?' and don't take no for an answer.
Jesse Ibarra
January 15, 2026this is why medicine is a fucking circus. doctors prescribe like they're playing darts blindfolded.
black box warning? yeah, right. that's just a sticker they print and ignore.
the real problem? lazy prescribers who think 'gout' is a tiny thing and don't bother checking the rest of the med list.
we're not saving lives here. we're just delaying the next coroner's report.
lucy cooke
January 15, 2026the tragedy isn't the drug interaction-it's the epistemological collapse of clinical judgment.
we've reduced human physiology to a checklist, then outsourced vigilance to algorithms that don't understand suffering.
allopurinol isn't the villain. it's the symptom. the real disease? the fragmentation of care.
when your rheumatologist, gastroenterologist, and PCP operate in silos, you're not a patient-you're a data point with a pulse.
Gregory Parschauer
January 16, 2026you people act like this is news. i've been screaming about this since med school.
azathioprine + allopurinol = bone marrow suicide. period.
if your doctor doesn't know this, they shouldn't be prescribing.
and don't give me that 'but my gout is mild' crap-your life isn't a tradeoff.
febuxostat exists. use it. or get your blood drawn. or die quietly. your choice.
Rosalee Vanness
January 16, 2026i'm a nurse who's seen this go sideways too many times.
one guy? 72, on azathioprine for RA, gets allopurinol for a swollen toe.
two weeks later, he’s in ICU with a WBC of 400.
his daughter said he didn’t even know he was on azathioprine-his old doc had switched him to it years ago and never told him.
we had to transfuse him twice.
he’s fine now, but he won’t walk right for months.
so yeah. this isn’t theoretical.
if you’re on either of these, ask for your last CBC.
if it’s older than 30 days? you’re playing russian roulette with your blood.
Trevor Davis
January 17, 2026i’m on azathioprine for crohn’s. my doc tried to put me on allopurinol for gout. i said no.
then i looked it up.
holy shit.
so i went back and said: 'i read your notes. you didn’t check my meds properly.'
he apologized. gave me febuxostat.
now i’m gout-free and not one blood cell short.
don’t be shy. ask. demand. google it. your life’s not worth the risk.
Avneet Singh
January 18, 2026the pharmacokinetic dynamics of thiopurine metabolism are fundamentally incompatible with xanthine oxidase inhibition unless 6-TGN levels are tightly constrained within the 230-450 pmol/8x10^8 RBC therapeutic window.
any deviation beyond 6-MMP >5700 pmol/8x10^8 RBC induces hepatotoxic shunting.
non-specialists lack the infrastructure for metabolite monitoring.
therefore, the combination is not merely risky-it is epistemologically invalid outside tertiary centers.
Adam Rivera
January 18, 2026just wanted to say thanks for this post.
i’m from the US but my mom’s in the UK and she’s on azathioprine.
i showed her this and she went straight to her doc.
they switched her to febuxostat last week.
she says her joints feel better and she’s not scared anymore.
you saved her life without even knowing it.
thank you.
Nelly Oruko
January 19, 2026i think the real issue is how we treat patients like systems to optimize rather than people to protect.
we have the tools. we have the data.
but we don’t have the will to slow down.
if your doctor writes a script without asking about every other med you’re on… that’s not negligence.
that’s a system failure.
and we’re all paying for it.
Priyanka Kumari
January 21, 2026this is why i always tell my patients: 'if you're on immunosuppressants, treat every new med like a grenade.
pull the pin, read the label, ask three questions.'
i had a 58-year-old woman come in with a fever and bruising.
she was on azathioprine for lupus.
her PCP gave her allopurinol for 'a little toe pain.'
she had a WBC of 600.
we saved her.
but she lost 3 months of work.
don't let this happen to you.
you're not being difficult. you're being smart.
Lance Nickie
January 21, 2026allopurinol bad. febuxostat good. done.
Lethabo Phalafala
January 22, 2026i’m from South Africa and we don’t have access to metabolite testing here.
so when my rheumatologist said 'allopurinol is fine,' i said no.
i drove 200km to a private clinic just to get a second opinion.
they told me the same thing as this post.
i’m on febuxostat now.
my gout still flares, but at least i’m alive to complain about it.
if you have ANY access to a specialist-use it.
don’t wait until you’re in the ER.
Adam Vella
January 22, 2026the paradox of modern pharmacotherapy lies in its precision and its ignorance.
we can sequence genomes but we can’t coordinate prescriptions.
we know the exact metabolite thresholds for toxicity, yet we entrust this knowledge to overworked primary care physicians who manage 40 patients a day.
this isn’t a drug interaction-it’s a societal failure of care coordination.
the solution isn’t better drugs. it’s better systems.
until then, patients must become their own pharmacists.
and pray.
Alan Lin
January 24, 2026I want to thank the author for this meticulously detailed and clinically vital post.
The interaction between allopurinol and azathioprine represents one of the most preventable iatrogenic catastrophes in internal medicine.
As a physician who practices in an academic center, I can confirm that the 2021 survey data cited is accurate: the majority of non-specialists remain unaware of this risk.
It is not sufficient to rely on electronic health record alerts-these are frequently ignored or overridden.
What is required is a mandatory, system-wide protocol: when azathioprine is prescribed, a pharmacogenetic review of all concomitant medications must be triggered.
Furthermore, every patient on thiopurines should receive a printed, laminated safety card detailing this interaction.
Until then, patient advocacy remains the last line of defense.
Thank you for raising this critical issue with such clarity and urgency.