It’s easy to think of thyroid medication like a simple pill you take once a day - something that fixes a problem and then fades into the background. But when it’s misused, even a common drug like levothyroxine can turn dangerous. People take it to lose weight, boost energy, or chase performance gains without knowing the risks. The result? A quiet epidemic of thyroid medication misuse that’s landing people in emergency rooms with heart rates over 140 beats per minute, chest pain, and even life-threatening fever.
How a Safe Drug Becomes a Hazard
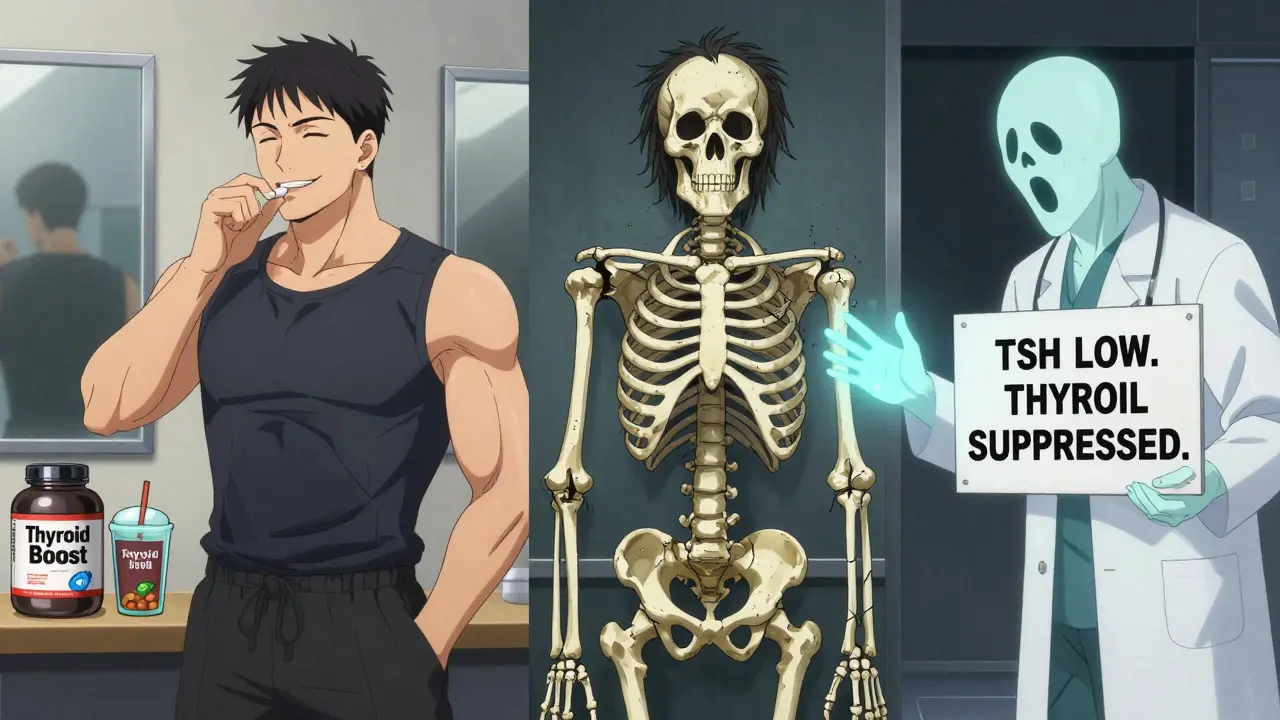
Levothyroxine, the synthetic form of thyroxine (T4), is one of the most prescribed medications in the U.S., with over 120 million prescriptions filled in 2023. It’s lifesaving for people with hypothyroidism. But when someone takes more than prescribed - or takes it without a diagnosis - the body gets flooded with thyroid hormone. That’s not therapy. That’s poisoning. The body doesn’t care if you’re doing it for weight loss, fitness, or just feeling "more alive." Excess thyroid hormone speeds up every system: your heart races, your metabolism burns too fast, your muscles shake, your bones weaken. The American Thyroid Association says about 20% of hyperthyroidism cases come from medication misuse. Of those, 5-10% are intentional abuse - often by people who don’t even realize they’re harming themselves. Here’s the scary part: the symptoms look like stress, anxiety, or just being "out of shape." Tremors, insomnia, sweating, diarrhea, rapid heartbeat - all dismissed as lifestyle issues. But they’re red flags. A 2021 study found that 12% of people showing up with hyperthyroid symptoms were actually abusing thyroid meds. Most were women in their mid-30s.What Happens When You Take Too Much
If you’re taking extra levothyroxine, your body sends clear signals:- Weight loss that doesn’t match your diet or exercise
- Heart palpitations or chest pain - even when you’re sitting still
- Shaky hands, trouble sleeping, constant nervousness
- Heat intolerance - sweating through clothes in a cool room
- Diarrhea or nausea without a clear cause
- Temporary hair thinning - not from genetics, but from hormonal chaos
It’s Not Just Levothyroxine
Levothyroxine is the usual suspect, but it’s not the only culprit. Some drugs you wouldn’t expect can wreck your thyroid too. Amiodarone, a heart rhythm drug, is 37.3% iodine by weight. That’s a massive dose. It can cause both hyperthyroidism and hypothyroidism. Type 1 amiodarone-induced thyrotoxicosis (AIT) happens when the thyroid goes into overdrive. Type 2 is worse - the thyroid literally swells and leaks hormone, causing sudden, severe symptoms. Iodinated contrast agents used in CT scans? They can trigger thyrotoxicosis weeks later, especially in people with existing thyroid issues. Immune checkpoint inhibitors - cancer drugs that help the body fight tumors - cause thyroid dysfunction in up to 8% of patients. Symptoms show up fast, and they’re silent until it’s too late. Doctors now recommend thyroid tests every 4-6 weeks during treatment. Even lithium, used for bipolar disorder, causes hypothyroidism in 15-20% of long-term users. Unlike Hashimoto’s, which is permanent, lithium-induced hypothyroidism often reverses after stopping the drug.Real People, Real Consequences
Reddit’s r/Thyroid community has over 125,000 members. One post from September 2023 tells the story of "FitLifeJunkie," who took 200 mcg of levothyroxine daily for three months to lose weight. They ended up in the ER with a heart rate of 142 bpm and chest pain. "Doctors said I was lucky to be alive," they wrote. Another user, "SarahM," shared how her doctor kept increasing her dose because she was losing weight - not knowing she was secretly taking extra pills. It took six months to stabilize after she confessed. On Drugs.com, levothyroxine has a 5.4/10 rating. Nearly 4 out of 10 negative reviews blame doctors for not monitoring levels. Over a quarter cite side effects from incorrect dosing. These aren’t rare cases. A 2022 survey found 19% of thyroid patients admitted to skipping doses. Of those, 43% had worsening symptoms within three days. Meanwhile, gym-goers are turning to thyroid pills as a shortcut. One study found 8.7% of people who work out regularly admitted to using thyroid medication without a prescription. They think they’re being efficient. They’re risking their hearts.How to Avoid the Trap
The good news? Most medication-induced thyroid problems are preventable.- Never take thyroid medication unless prescribed. No exceptions. Not for weight loss. Not for energy. Not because a friend said it worked.
- Take it on an empty stomach. Calcium, iron, soy, and even coffee can block absorption by up to 50%. Wait at least 30-60 minutes before eating or taking supplements.
- Get tested regularly. TSH and free T4 should be checked every 6-8 weeks when starting or adjusting dose. It takes six weeks for your body to fully respond to a change.
- Don’t double up. If you miss a dose, take it as soon as you remember - unless it’s close to your next dose. Never double up to "catch up."
- Ask about alternatives. If you’re on amiodarone or lithium, ask your doctor about thyroid monitoring schedules. Don’t wait for symptoms.
The Bigger Picture
The global thyroid treatment market is growing fast - expected to hit $5.2 billion by 2027. But growth doesn’t mean safety. The FDA has documented 217 websites selling thyroid hormones without prescriptions - a 43% jump since 2020. These aren’t regulated. Doses vary wildly. Some pills contain nothing. Others have lethal amounts. Compounded thyroid medications, often marketed as "natural" or "customized," caused 127 cases of iatrogenic hyperthyroidism between 2018 and 2022. They’re not FDA-approved. No quality control. Just dangerous guesswork. And the cost? In the U.S. alone, hospitalizations for thyroid medication complications now cost $427 million annually. That’s not just money - it’s lives disrupted, careers derailed, families stressed.What Recovery Looks Like
If you’ve misused thyroid medication, recovery is possible - but it takes time and patience. Mild cases often resolve within 2-3 weeks of stopping the drug, with cardiac monitoring. Your TSH will slowly return to normal. Your heart rate drops. The tremors fade. Hair regrows. But bone density? That’s a slower story. Chronic misuse increases osteoporosis risk by 3.2 times. Bone loss can continue for years unless caught early. For those with drug-induced hypothyroidism - say, from amiodarone or lithium - thyroid hormone replacement may be temporary. Many patients return to normal function after stopping the offending drug. The key? Honesty. With yourself. With your doctor. If you’ve taken extra pills, say so. If you’ve skipped doses to "reset," admit it. Your doctor isn’t judging - they’re trying to save you.Final Thought: Thyroid Health Isn’t a Shortcut
Thyroid medication isn’t a magic pill for weight loss or energy. It’s a precise tool for a specific medical condition. When used correctly, it restores balance. When misused, it breaks your body. The rise in misuse reflects a deeper problem: we’re looking for quick fixes in a world that rewards speed over sustainability. But your thyroid doesn’t work that way. It doesn’t respond to willpower or Instagram trends. It responds to biology - and biology doesn’t forgive mistakes. If you’re struggling with fatigue, weight changes, or mood swings, talk to a doctor. Get tested. Don’t self-diagnose. Don’t self-medicate. The safest, most effective way to feel better isn’t through a pill you bought online. It’s through understanding your body - and treating it with care.Can taking too much levothyroxine cause permanent damage?
Yes, if abuse continues for months or years. Chronic excess thyroid hormone can lead to irreversible heart damage, including atrial fibrillation and cardiomyopathy. It also accelerates bone loss, increasing osteoporosis risk by 3.2 times. While many symptoms reverse after stopping the drug, some damage - especially to the heart and bones - may not fully recover without long-term intervention.
How do doctors tell if someone is abusing thyroid medication?
Doctors look for three key signs: high T3/T4 levels with low TSH, low thyroglobulin (a protein made by the thyroid), and low radioactive iodine uptake on a scan. In autoimmune hyperthyroidism like Graves’ disease, the thyroid is overactive and takes up iodine. In medication abuse, the thyroid is suppressed - it’s not making hormone, you’re just flooding your system with it. Low thyroglobulin confirms this. A patient who claims they’ve been taking their dose consistently but has these markers is likely hiding misuse.
Can thyroid medication cause weight gain?
Yes - but only if you’re underdosed or stop taking it. Levothyroxine increases metabolism. If you’re taking too little, your body slows down, leading to weight gain. If you suddenly stop taking it after long-term use, you may gain weight quickly as your metabolism drops. But taking too much doesn’t cause weight gain - it causes rapid, unhealthy weight loss from muscle and water loss, not fat loss.
Is it safe to take thyroid medication with coffee or calcium supplements?
No. Calcium, iron, soy, and even coffee can block up to 50% of levothyroxine absorption. Always take it on an empty stomach, at least 30-60 minutes before eating or taking any supplements. If you take calcium for bones or iron for anemia, space them at least 4 hours apart from your thyroid pill.
Are there natural alternatives to levothyroxine?
No. Natural thyroid extracts (like desiccated pig thyroid) are not safer or more effective than levothyroxine. They contain inconsistent doses of T3 and T4, which can cause dangerous spikes in hormone levels. The FDA has warned against compounded thyroid products because they lack quality control. Levothyroxine is the gold standard because it’s pure, stable, and predictable.
How long does it take to recover from thyroid medication abuse?
Symptoms like tremors, heart palpitations, and insomnia often improve within days to weeks after stopping. But TSH levels can take 6-12 weeks to normalize. Bone density recovery may take years and requires calcium, vitamin D, and weight-bearing exercise. Full recovery depends on how long and how much you abused the medication. Early intervention makes a huge difference.






9 Comments
Christine Joy Chicano
January 7, 2026People treat thyroid meds like energy drinks-pop a pill, feel alive, no questions asked. But your thyroid isn’t a gas tank you can just refill. It’s a delicate orchestra, and throwing in extra hormones? That’s like hiring a metal drummer to play Mozart. The body doesn’t care if you’re chasing abs or a 6 a.m. workout buzz. It just screams until something breaks. And by then, it’s not just fatigue-it’s atrial fibrillation, brittle bones, and a doctor asking why you didn’t say anything sooner.
And don’t even get me started on those ‘natural’ desiccated thyroid pills from sketchy websites. They’re like baking a cake with a bag of sugar and a prayer-no consistency, no safety, just chaos in a capsule. Levothyroxine is boring because it works. That’s the point.
Also, coffee? Seriously? I once had a patient who took her pill at 7 a.m. and had her espresso at 7:05. She was shocked her TSH was still high. Spoiler: calcium and caffeine are the silent saboteurs of endocrinology.
It’s not about willpower. It’s about biology. And biology doesn’t do shortcuts.
Stop treating your endocrine system like a TikTok hack.
Adam Gainski
January 9, 2026This is such an important post. I’ve seen too many patients come in thinking levothyroxine is a ‘metabolism booster’-especially women in their 30s who’ve been told by influencers that ‘thyroid issues are why you can’t lose weight.’
The truth? Most of them have normal thyroid function. They’re just stressed, sleep-deprived, or eating too many processed carbs. But the myth is so pervasive that they self-medicate. And then they show up with palpitations, insomnia, and a TSH of 0.01.
Doctors need to do more patient education. Not just hand out prescriptions and say ‘come back in 6 weeks.’ We need to explain why this isn’t like taking a vitamin. It’s a hormone replacement that can literally kill you if misused.
Also, props for mentioning amiodarone. That drug is a silent thyroid wrecking ball. I’ve had patients develop hyperthyroidism 6 months after starting it and had no clue why.
Keep spreading awareness. This needs to be in every primary care office.
Rachel Steward
January 10, 2026Let’s be real-this isn’t about thyroid meds. It’s about the collapse of medical trust and the rise of self-diagnosis culture. People don’t trust doctors anymore because doctors spend 7 minutes per visit and hand out prescriptions like candy. So they go online, find a Reddit thread, and decide they’re hypothyroid because they feel ‘tired’ after a bad night’s sleep.
Then they buy pills off a shady site because ‘it worked for my cousin.’
And now we have a generation of people with iatrogenic hyperthyroidism who think they’re ‘biohacking.’
It’s not a medical crisis. It’s a cultural one.
Stop blaming the drug. Blame the system that lets people think their thyroid is broken because they ate pizza last night.
And yes, the 200 mcg guy? He’s not a victim. He’s a liability. And if he’s still alive, he should be ashamed.
Also, ‘natural thyroid’ is a scam. Pig thyroid? That’s just medieval medicine with a wellness influencer filter.
Alex Danner
January 10, 2026Bro. I saw a guy in the ER last month. 28 years old. Gym bro. Took levothyroxine ‘to burn fat faster.’ He was sweating through his shirt, heart rate 156, shaking like he’d just done 500 push-ups. He thought he was being smart.
Turns out he bought it off a guy at the gym who said, ‘It’s just a pill, man. No one gets hurt.’
He’s lucky he didn’t have a stroke.
And now he’s got a 3-month follow-up with an endocrinologist and a lifetime of wondering if his heart will ever be the same.
This isn’t just ‘misuse.’ It’s a slow-motion suicide pact with the internet.
Someone needs to make a documentary on this. Like ‘The Social Dilemma’ but for thyroid pills.
Elen Pihlap
January 11, 2026OMG I did this for 2 months and didn’t even know it was bad I lost 15 pounds and felt so awake but then my heart started racing and I thought I was having a panic attack but it was the pill I’m so scared now please tell me I’m not broken
Sai Ganesh
January 12, 2026In India, thyroid issues are often dismissed as ‘stress’ or ‘women’s problems.’ Many women self-medicate with leftover prescriptions from relatives, believing it will help with fatigue or weight gain. There’s little awareness about the dangers.
One patient I knew took her mother’s levothyroxine for three years because she ‘felt sluggish.’ She developed atrial fibrillation at 34. No family history. No prior diagnosis. Just a pill passed down like a family recipe.
We need public health campaigns-not just for the West. In rural clinics, doctors don’t always have time to explain TSH levels. So misinformation spreads faster than the meds themselves.
Education is the real cure. Not just more tests.
Paul Mason
January 12, 2026Look, I’m not a doctor, but I’ve read a lot. And let me tell you-this is a total mess. People are treating thyroid meds like Adderall. ‘I’m tired? Take a pill.’ ‘I’m fat? Take more.’
And don’t even get me started on the ‘natural thyroid’ cult. Desiccated pig thyroid? That’s not medicine, that’s a horror movie. No regulation, no science, just vibes and vibes alone.
Also, coffee after your pill? You’re not a genius. You’re just wasting your money.
Stop being a biohacker. Start being a human. Your thyroid doesn’t care about your Instagram bio. It cares about balance.
And if you’re still taking it without a prescription? You’re not brave. You’re just dumb.
Katrina Morris
January 12, 2026i had no idea thyroid meds could do this to you i thought it was just for tired people
my aunt took hers every morning with her coffee and never told anyone
she had a stroke last year and the doctors said it might have been from the pills
im gonna get tested now
thank you for posting this
Andrew N
January 13, 2026Everyone’s acting like this is new. It’s not. I’ve been in endocrinology for 15 years. We’ve been seeing this since the 2010s. It’s just getting worse because of social media.
People don’t want to hear ‘get more sleep’ or ‘eat better.’ They want a pill. And the internet gives it to them.
The real problem? Doctors who prescribe without follow-up. You can’t just write a script and disappear.
And the worst part? Patients who lie about dosing because they’re embarrassed.
We’re not here to judge. We’re here to fix. But we can’t fix what you won’t admit.
So if you’re reading this and you’ve taken extra pills-tell your doctor. It’s not a crime. It’s a mistake. And mistakes can be fixed.
But only if you speak up.