Metabolic Complications: What They Are and Why They Matter
When dealing with Metabolic Complications, a range of disorders that disrupt normal chemical processes in the body. Also known as metabolic disorders, they often show up as elevated blood sugar, abnormal cholesterol, or weight changes. Right alongside you’ll find Diabetes, a chronic condition marked by high glucose levels and Obesity, excess body fat that strains metabolic pathways. Together they form a cluster that affects millions and drives many health policies.
Key Players in the Metabolic Web
Insulin Resistance, the reduced ability of cells to respond to insulin sits at the heart of many metabolic complications. When insulin can’t get glucose into cells efficiently, blood sugar spikes, prompting the pancreas to pump more insulin. Over time this feedback loop fuels Hyperlipidemia, high levels of lipids in the blood, raising heart disease risk. Both conditions often appear together, creating a vicious cycle that worsens diabetes and obesity.
Diet plays a huge role. High‑fiber foods help regulate blood sugar and improve gut health, which in turn can blunt insulin spikes. Soluble fiber slows carbohydrate absorption, while insoluble fiber keeps the digestive system moving, reducing the chance of diarrhea that sometimes follows abrupt diet changes. By stabilizing glucose, fiber indirectly eases the burden on insulin‑producing cells, making it a frontline tool against metabolic complications.
Medications can tip the balance, too. Diuretics like Lasix (furosemide), a loop diuretic used for fluid overload may cause electrolyte shifts that affect metabolism. Antidepressants such as Effexor (venlafaxine), an SNRI linked to weight changes sometimes lead to weight gain, feeding obesity and insulin resistance. Even iron supplements like Ferrous Sulfate, a common iron preparation can influence metabolic rate when used improperly, highlighting the need for careful dosing.
Monitoring is essential. Routine lab tests—fasting glucose, HbA1c, lipid panel, and electrolytes—provide a snapshot of where your metabolism stands. When values drift, a clinician can adjust diet, tweak meds, or add targeted therapies. Early detection of insulin resistance or hyperlipidemia often prevents progression to full‑blown diabetes or cardiovascular disease.
Lifestyle tweaks go beyond food. Regular aerobic exercise boosts insulin sensitivity, helping cells capture glucose more effectively. Even modest activity, like brisk walking for 30 minutes a day, can lower triglycerides and improve HDL cholesterol. Combining movement with a fiber‑rich diet creates a double‑hit against metabolic complications, tackling both the cause and the symptom.
For those already dealing with diabetes or obesity, personalized plans matter. Some patients benefit from low‑carb approaches, while others thrive on Mediterranean‑style meals rich in healthy fats and whole grains. The key is consistency and monitoring—track blood sugars, weight, and lipid levels regularly to see what works.
All these pieces—conditions, diet, meds, labs, and activity—interlock to form the bigger picture of metabolic health. Below you’ll find a curated collection of articles that dive deeper into each area, from how fiber can soothe diarrhea to safe ways to buy generic medications online. Use them as a toolbox to manage or prevent metabolic complications in real life.
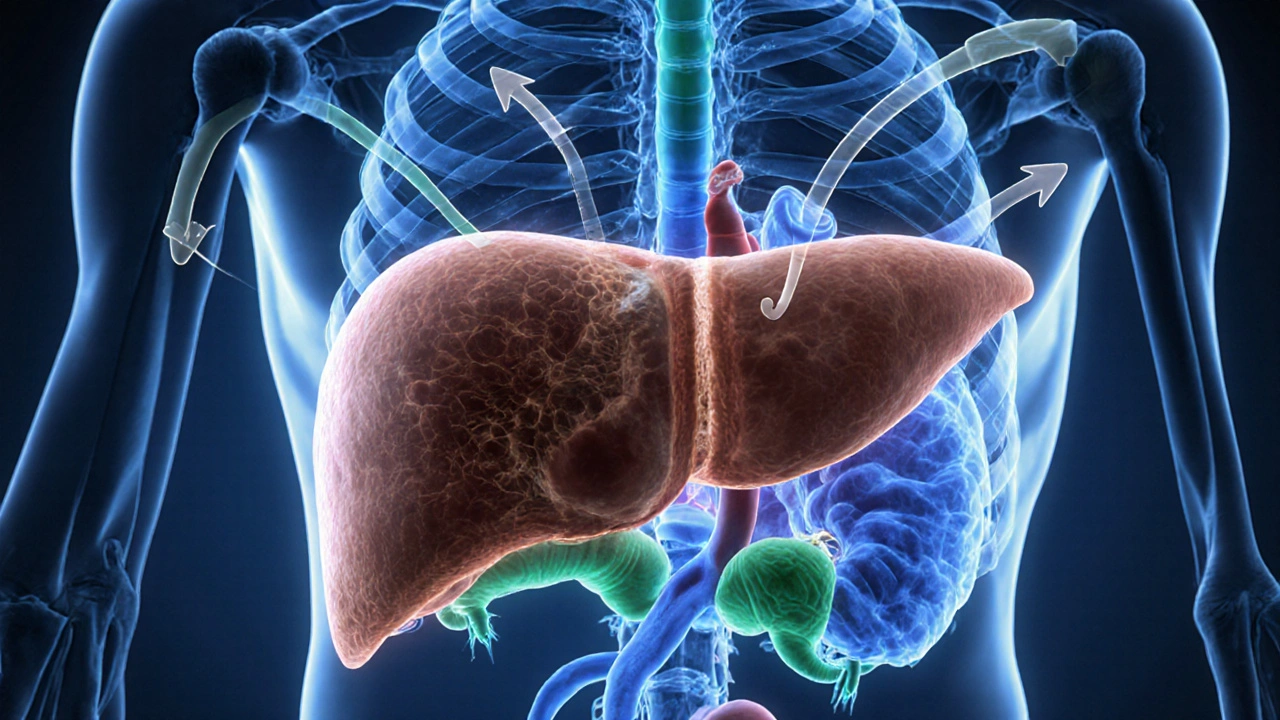
Liver Failure & Endocrine System: Essential Facts & Hormone Impacts
Learn how liver failure disrupts insulin, thyroid, sex hormones and cortisol, recognize symptoms, and manage hormonal imbalances for better health.
Continue Reading



