Liver Failure & Hormone Impact Simulator
This interactive simulates how liver dysfunction affects key hormones and their associated symptoms. Select a hormone to learn more about its disruption patterns.
Insulin & Glucose
Impaired glucose regulation and insulin resistance
Hypoglycemia Weight changesThyroid Hormones
Reduced T3 conversion and binding protein production
Fatigue Cold intoleranceSex Hormones
Altered estrogen and testosterone metabolism
Sexual dysfunction Irregular periodsCortisol
Delayed clearance leading to elevated levels
Muscle wasting High BPGrowth Hormone
Reduced IGF-1 production and muscle loss
Weakness Poor healingAcute vs Chronic
Different hormonal profiles over time
Transient ProgressiveKey Takeaways
- Severe liver damage disrupts insulin, thyroid, sex hormones and cortisol
- Acute and chronic liver failure show different hormonal patterns
- Symptoms like sudden weight change, low blood sugar or sexual dysfunction often signal endocrine disruption
- Medical management focuses on correcting hormone levels and supporting nutrition
Key Takeaways
- Severe liver damage messes with insulin, thyroid, sex hormones and cortisol.
- Acute and chronic liver failure show different hormonal patterns.
- Symptoms like sudden weight change, low blood sugar or sexual dysfunction often signal endocrine disruption.
- Medical management focuses on correcting hormone levels, preventing complications and supporting nutrition.
- Regular monitoring of blood tests and endocrine function can improve quality of life.
If you’ve heard the term liver failure tossed around, it’s more than just a bad liver-it reshapes your whole hormonal landscape. Below we break down what happens when the liver quits and how the endocrine system reacts, so you can spot warning signs early and work with doctors on a plan that covers both organs.
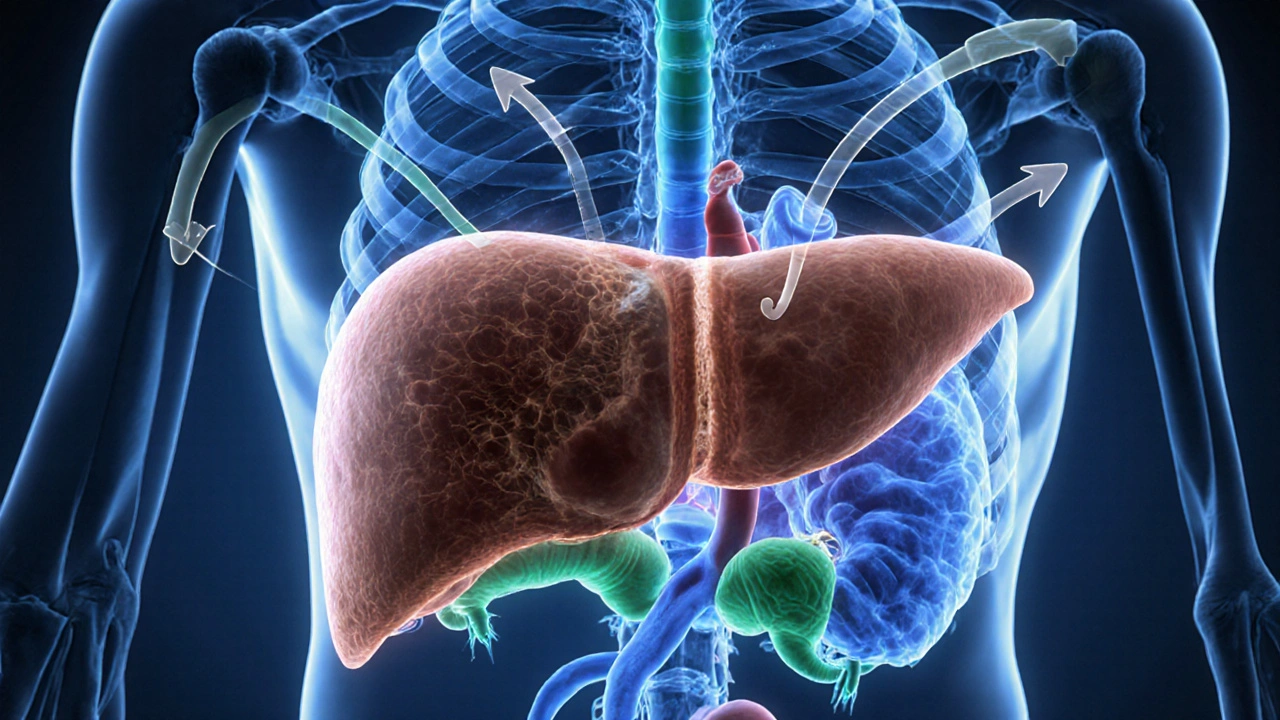
What is Liver Failure?
When the liver stops working properly, Liver Failure is a condition where the organ can no longer perform its vital metabolic, detoxifying and synthetic functions, leading to a buildup of toxins and a drop in essential proteins. occurs in two main forms: acute (sudden injury such as a drug overdose) and chronic (progressive scarring from hepatitis, alcohol or fatty liver disease). The liver’s role in processing nutrients, storing glucose, and producing carrier proteins makes it a central hub for the body’s chemistry. When that hub collapses, hormone production and clearance go off‑track.
How the Endocrine System Works
The endocrine system Endocrine System is a network of glands that release hormones directly into the bloodstream to regulate metabolism, growth, reproduction and stress responses. includes the pituitary, thyroid, adrenal glands, pancreas and gonads. Hormones act as messengers, telling cells when to grow, store energy or respond to stress. Because the liver clears many hormones from circulation and manufactures hormone‑binding proteins, the two systems are tightly linked.
Hormone Disruption in Liver Failure
When liver function drops, several hormonal pathways become unbalanced. Below are the most clinically relevant changes.
Insulin and Glucose Regulation
Insulin is a pancreatic hormone that lowers blood glucose by promoting cellular uptake and storage. clearance relies heavily on liver enzymes. In liver failure, insulin stays longer in the bloodstream, causing a paradox: high insulin levels but impaired signaling (insulin resistance). At the same time, the liver’s reduced ability to store glycogen leads to episodes of hypoglycemia, especially after fasting.
Thyroid Hormones
The liver converts the inactive thyroxine (T4) into the active triiodothyronine (T3). With damaged liver cells, this conversion falters, creating a pattern known as "low‑T3 syndrome." Patients often feel cold, sluggish and may gain weight despite a normal thyroid gland. The liver also produces thyroid‑binding globulin, so low levels reduce the total circulating thyroid hormone pool.
Sex Hormones
Estrogen and testosterone are metabolized by the liver. In chronic liver disease, estrogen clearance drops, leading to higher circulating estrogen. Men may develop gynecomastia, loss of libido and testicular atrophy. Women can experience irregular periods or worsening of estrogen‑related symptoms like bloating.
Cortisol and Stress Response
Cortisol is a steroid hormone released by the adrenal glands that helps the body respond to stress and regulate metabolism. is partially deactivated by the liver. When the liver falters, cortisol clearance slows, raising circulating levels. This can worsen insulin resistance, increase blood pressure and promote muscle wasting.
Growth Hormone and IGF‑1
Growth hormone (GH) from the pituitary stimulates the liver to produce insulin‑like growth factor‑1 (IGF‑1). In liver failure, IGF‑1 drops dramatically, leading to muscle loss, poor wound healing and lower overall anabolic tone. Elevated GH levels may be seen as the pituitary tries to compensate.

Acute vs Chronic Liver Failure: Hormonal Profile Comparison
| Hormone | Acute Failure | Chronic Failure |
|---|---|---|
| Insulin | Sharp rise, transient hypoglycemia | Persistent hyperinsulinemia with insulin resistance |
| Thyroid (T3) | Rapid drop, "low‑T3 syndrome" within days | Chronically low T3, normal T4 |
| Estrogen | Modest increase due to reduced clearance | Significant elevation, especially in men |
| Cortisol | Elevated stress response, may spike >2× | Consistently high, contributing to catabolism |
| IGF‑1 | Drop of 30‑40% within a week | Severe deficiency, often <10% of normal |
Clinical Signs That Point to Endocrine Disruption
Because hormones act system‑wide, patients with liver failure may notice odd symptoms that don’t fit a classic liver picture. Recognizing these clues helps clinicians intervene early.
- Sudden drops in blood sugar after an overnight fast or during illness.
- Persistent fatigue, cold intolerance or unexplained weight gain - hallmarks of low‑T3.
- Gynecomastia, reduced facial hair or erectile difficulties in men.
- Irregular menstrual cycles, heavy bleeding or worsening pre‑menstrual mood swings in women.
- High blood pressure, facial rounding or “moon face” from excess cortisol.
- Muscle wasting and poor wound healing indicating low IGF‑1.
Managing Hormonal Imbalances
Treating hormone issues in liver failure requires a two‑pronged approach: stabilising liver function where possible, and directly adjusting hormone levels.
Optimising Liver Support
Medical therapies such as lactulose for encephalopathy, albumin infusions for circulatory support, and antiviral or steroid treatments for underlying hepatitis can improve hepatic clearance. When the liver regains even modest function, hormone homeostasis often follows.
Targeted Hormone Replacement or Suppression
- Insulin: Use of short‑acting insulin or glucose infusions during acute hypoglycemia; consider metformin cautiously if insulin resistance dominates.
- Thyroid: Low‑dose liothyronine (T3) can bypass the conversion block, but monitor cardiac status closely.
- Sex Hormones: Anti‑estrogen agents (e.g., tamoxifen) or testosterone replacement may be needed for severe gynaecomastia or libido loss, always under specialist guidance.
- Cortisol: If cortisol excess drives complications, low‑dose metyrapone can reduce production; otherwise, manage stress and avoid exogenous steroids.
- IGF‑1: Recombinant IGF‑1 therapy is experimental; focus on nutrition and resistance exercise to boost natural production.
Monitoring Strategy
Regular labs every 4-6 weeks-fasting glucose, insulin, TSH/T3, estradiol/testosterone, cortisol, and IGF‑1-help track trends. Imaging (ultrasound or elastography) informs liver progression, while endocrine imaging is rarely needed unless a tumor is suspected.
Nutrition and Lifestyle Tips
Food choices can either ease or worsen hormonal stress on the liver.
- Prioritise protein sources (lean meat, legumes, dairy) to supply amino acids for albumin and IGF‑1 synthesis.
- Include complex carbs (whole grains, starchy vegetables) to maintain glycogen stores and avoid hypoglycemia.
- Limit simple sugars and fructose, which increase insulin resistance and fat buildup.
- Consume omega‑3 rich fish or flaxseed to modulate inflammation and support hormone balance.
- Avoid excessive alcohol, herbal supplements with unknown liver toxicity, and high‑dose vitamin A.
- Stay active with low‑impact resistance training to preserve muscle mass and improve insulin sensitivity.
When to Seek Professional Help
If you notice any of the clinical signs listed above, schedule a check‑up promptly. Early endocrine assessment can prevent complications like severe hypoglycemia, cardiac arrhythmias from thyroid imbalance, or bone loss from prolonged cortisol excess.
Frequently Asked Questions
Can liver failure cause diabetes?
Yes. Impaired insulin clearance and resistance often lead to higher blood sugar levels. Some patients develop overt diabetes, especially in chronic liver disease.
Why do men with liver disease develop breast tissue?
The liver’s reduced ability to break down estrogen lets this hormone accumulate, stimulating breast tissue growth.
Is low‑T3 syndrome reversible?
Often, yes. Improving liver function through medication, nutritional support or transplantation restores T4‑to‑T3 conversion.
Should I take extra thyroid hormone if my T3 is low?
Only under doctor supervision. Direct T3 supplementation can help, but dosing must consider heart health and liver status.
How often should hormone labs be checked in chronic liver failure?
Every 4-6 weeks for the first few months, then every 2-3 months once stable. Frequency may increase if symptoms change.





20 Comments
Ian Banson
October 4, 2025Liver failure basically turns your body into a hormonal disaster zone.
marcel lux
October 4, 2025The cascade of endocrine disruption you outlined really shows how intertwined the liver is with metabolism. It’s fascinating to see insulin resistance paired with hypoglycemia in the same scenario. Managing both sides can be a real challenge for clinicians.
Charlotte Shurley
October 5, 2025When the liver can’t clear hormones, you’ll see elevated estrogen in men and low‑T3 in many patients. The symptoms you listed match what we see in practice.
Steph Hooton
October 6, 2025Indeed, the reduction in IGF‑1 production can lead to profound muscle wasting – a condition often overlooked in routine assessments. Moreover, the chronic elevation of cortisol exacerbates insulin resistance, creating a vicious cycle. The clinical implications are far‑reaching, and early detection is paramount.
Judson Voss
October 7, 2025Honestly, most patients don’t even realize their hormone levels are off until they show severe symptoms. It’s a classic example of silent deterioration.
Jessica Di Giannantonio
October 8, 2025Wow, the way you laid out the hormone shifts is eye‑opening! It really drives home how vital comprehensive monitoring is.
RUCHIKA SHAH
October 9, 2025Liver failure messes up hormone clearance and production it causes insulin spikes and low thyroid hormones
Justin Channell
October 10, 2025Great summary 😊 It really helps to visualise the hormonal domino effect when the liver is compromised
Basu Dev
October 11, 2025In clinical practice, the interplay between hepatic insufficiency and endocrine dysregulation is a multi‑layered puzzle that demands a systematic approach. First, the liver’s role in insulin clearance means that hyperinsulinemia can coexist with paradoxical insulin resistance, which complicates glucose management strategies. Second, the impaired conversion of T4 to T3 generates the low‑T3 syndrome, a condition frequently misdiagnosed as primary hypothyroidism, leading to inappropriate levothyroxine dosing. Third, estrogen metabolism is markedly reduced, resulting in elevated estradiol levels that manifest as gynecomastia in men and menstrual irregularities in women. Fourth, cortisol clearance slows, raising circulating cortisol and thereby reinforcing catabolic pathways, muscle wasting, and hypertension. Fifth, the hepatic synthesis of thyroid‑binding globulin declines, further lowering the total thyroid hormone pool. Sixth, growth hormone levels may rise as a compensatory mechanism, yet the downstream production of IGF‑1 by the liver plummets, undermining anabolic signaling. Seventh, in acute liver failure, these hormonal shifts occur abruptly, whereas in chronic disease they evolve insidiously, often escaping early detection. Eighth, nutritional status interplays with these endocrine changes; malnutrition exacerbates hormone deficiencies while hormone abnormalities can hinder nutrient utilization. Ninth, therapeutic interventions must therefore be multifaceted: adjusting insulin regimens, considering low‑dose T3 supplementation, monitoring estrogen levels, and addressing cortisol excess with appropriate pharmacologic agents when indicated. Tenth, regular laboratory surveillance, including fasting glucose, HbA1c, free T3, estradiol, cortisol, and IGF‑1, is essential for tracking disease progression. Eleventh, patient education about symptom recognition-such as sudden weight loss, cold intolerance, or sexual dysfunction-empowers earlier clinical contact. Twelfth, interdisciplinary collaboration among hepatologists, endocrinologists, and nutritionists optimizes outcomes. Thirteenth, emerging research on hepatokines suggests additional layers of hormonal regulation that may become therapeutic targets in the future. Fourteenth, clinicians should remain vigilant for drug‑induced hormonal disturbances, as many medications are metabolized by the liver. Fifteenth, ultimately, integrating hormonal assessment into the broader management of liver failure offers a more holistic view of patient health and can improve quality of life.
Krysta Howard
October 11, 2025Spot‑on breakdown! The cascade you described explains why we see such diverse presentations. Addressing each hormonal axis is non‑negotiable for proper care :)
Elizabeth Post
October 12, 2025I agree, especially on the point about regular monitoring. Keeping an eye on IGF‑1 and cortisol can really make a difference in patient outcomes.
Brandon Phipps
October 13, 2025Judson’s comment hits the nail on the head-most patients are blissfully unaware until the symptoms become severe. It’s a silent creep that we need to fight with proactive screening and patient education. By integrating endocrine labs into routine liver panels, clinicians can catch imbalances early, reducing the risk of complications like refractory hypoglycemia or uncontrolled hypertension. Moreover, interdisciplinary case reviews can help identify subtle signs that might be missed in a single‑specialty setting. In short, awareness and early intervention are the twin pillars of effective management.
yogesh Bhati
October 14, 2025That long-winded explination from Basu is irectly on pnt but i think you could also add how diet plays a role . It s often neglected .
Akinde Tope Henry
October 15, 2025Krysta nailed the urgency-hormone monitoring isn’t optional.
Brian Latham
October 16, 2025Sure, but do we really need that many labs? It feels like overkill.
Barbara Todd
October 17, 2025I’m not convinced that extra testing changes outcomes dramatically.
nica torres
October 17, 2025Adding a dietician to the team can really fill the gap you mentioned, Yogesh.
Dean Marrinan
October 18, 2025Oh great, another concise reminder that we all need to read the whole thing twice. 🙄
Oluseyi Anani
October 19, 2025From a pathophysiological standpoint, the liver’s inability to deconjugate steroid hormones is a key driver of the hypercortisolemia observed in chronic hepatic insufficiency, which in turn aggravates gluconeogenesis and peripheral insulin resistance, creating a self‑reinforcing loop that accelerates catabolism.
Jeremy Wolfe
October 20, 2025Let’s keep the momentum going-aggressive monitoring and early endocrine intervention can truly shift the prognosis for these patients. We owe it to them to act decisively.