Sedative Combination Risk Calculator
Your Medication Selection
Risk Assessment
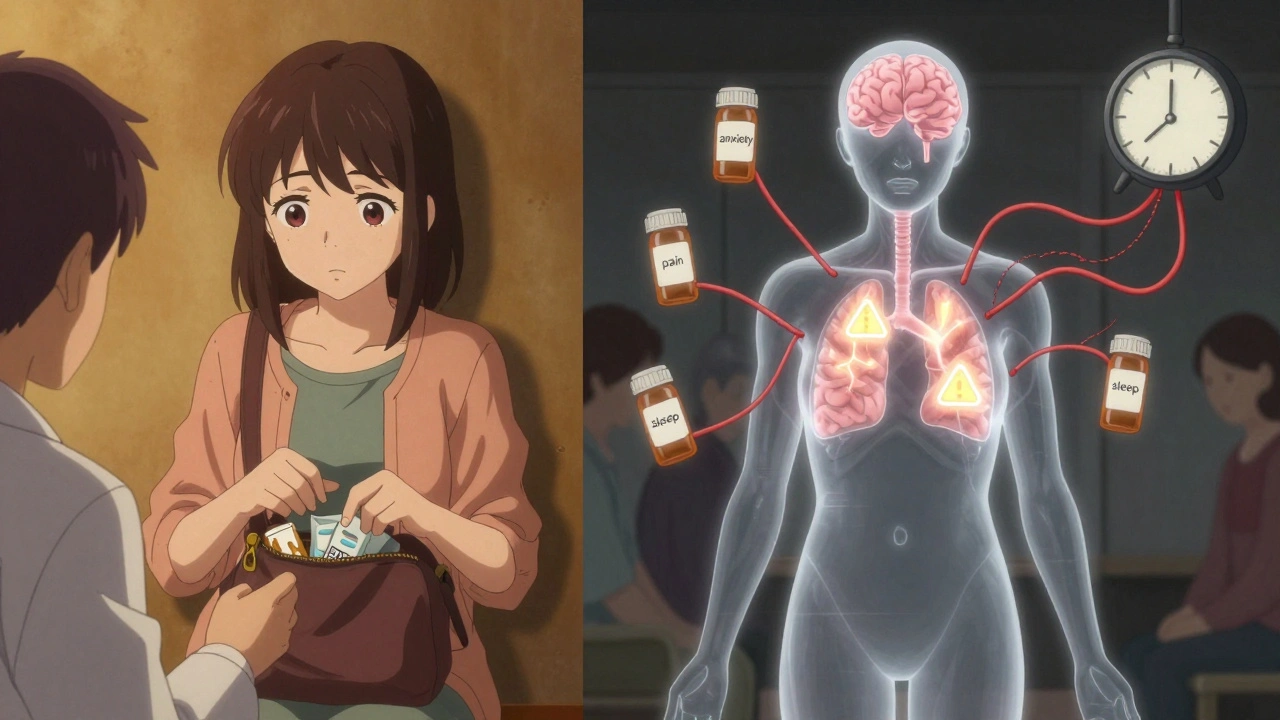
Putting together multiple sedatives might seem like a simple fix for sleep problems, anxiety, or chronic pain-but it’s one of the most dangerous things people do with their medications without even realizing it. The brain doesn’t treat each drug separately. When you mix opioids, benzodiazepines, alcohol, or sleep pills, they team up to slow your breathing, your heart, and your brain in ways that can kill you-even if you’re taking each one exactly as prescribed.
What Happens When Sedatives Combine?
Sedatives work by boosting GABA, a brain chemical that calms down nerve activity. Think of it like hitting the brakes on your nervous system. One sedative? That’s manageable. Two or three? It’s like slamming the brake pedal with your foot, your elbow, and your knee all at once. The result isn’t just stronger sedation-it’s a dangerous drop in breathing rate, blood pressure, and oxygen levels.
When someone takes an opioid like oxycodone with a benzodiazepine like Xanax, the risk of fatal overdose jumps 2.5 to 4.5 times higher than using opioids alone. That’s not a small increase. It’s the difference between a bad side effect and a trip to the emergency room-or worse. Even alcohol, which many people think of as harmless in moderation, can turn deadly when mixed with prescription sleep aids. One study found that nearly 13% of people on long-term opioids were drinking alcohol within two hours of taking their pain meds. That’s not a coincidence. It’s a ticking time bomb.
The Real-World Signs You’re in Danger
You don’t need to be unconscious to be in trouble. Early signs of CNS depression are easy to miss because they feel like just being tired or groggy:
- Breathing slower than 12 breaths per minute (normal is 12-20)
- Heart rate dropping below 50 beats per minute
- Confusion, slurred speech, or trouble remembering things
- Dizziness so bad you can’t stand without holding on
- Pupils that stay wide open even in bright light
- Extreme drowsiness-even after a full night’s sleep
When oxygen levels fall below 90%, your brain starts to suffer. Below 85%, you’re at risk of permanent damage. In some cases, breathing slows to just 4-6 breaths per minute. That’s not sleep. That’s a medical emergency. And it can happen within 15 to 20 minutes of taking the last dose.
Who’s Most at Risk?
This isn’t just about drug abusers. It’s about real people-often older adults, people with chronic pain, or those managing anxiety and depression-who are simply following their doctor’s orders.
People over 65 are especially vulnerable. Their bodies process drugs slower. Their brains are more sensitive. A single combination of three or more CNS depressants triples their risk of falling and breaking a hip. One study showed elderly patients on multiple sedatives had 3.4 times more hip fractures than those not taking them.
Women are also more likely to be prescribed these combinations. Studies show they’re 1.7 times more likely than men to be on multiple sedatives. Why? Often because they’re more likely to be diagnosed with anxiety, insomnia, or chronic pain-and prescribed multiple medications to treat each condition separately, without anyone looking at the full picture.
People with depression or a history of substance use are at even higher risk. One study found that nearly 40% of those with a substance use disorder were also taking sedatives, often without telling their doctor. Depression itself increases the risk of dangerous combinations by more than double. It’s a cycle: pain leads to anxiety, which leads to sleep problems, which leads to more pills-and no one stops to ask if all these pills are safe together.

Why Doctors Still Prescribe Dangerous Mixes
It’s not that doctors are careless. It’s that the system is broken. Most primary care doctors aren’t trained to see the big picture of drug interactions. They treat insomnia with a sleep aid. They treat anxiety with a benzodiazepine. They treat pain with an opioid. Each prescription makes sense on its own. But when they’re stacked together, the result is a perfect storm.
Even worse, many patients don’t tell their doctors about over-the-counter sleep aids, herbal supplements like valerian root, or even occasional alcohol use. They don’t think it counts. But it does. Valerian can double the effect of benzodiazepines. Alcohol? It’s not just a drink-it’s a powerful CNS depressant.
And here’s the scary part: most electronic health records still don’t warn doctors about these combinations. In 2020, over 10% of patients on long-term opioids were still getting benzodiazepines prescribed alongside them-even after the FDA and CDC warned against it.
What You Can Do to Stay Safe
You don’t have to live in fear. But you do need to be proactive.
- Make a full list of everything you take. Not just prescriptions. Include supplements, OTC sleep aids, alcohol, and even cannabis. Write it down. Bring it to every appointment.
- Ask your doctor: “Am I on any drugs that could dangerously interact?” Don’t wait for them to bring it up. Most won’t.
- Never mix alcohol with any sedative. Not even one drink. Not even if you’re “just having a glass of wine to relax.”
- Ask about alternatives. For anxiety, is there a non-addictive therapy or medication? For sleep, could cognitive behavioral therapy help instead of a pill?
- Get a medication review every 6 months. Especially if you’re over 65 or on more than three medications. Deprescribing-carefully reducing or stopping unnecessary drugs-has been shown to cut fall risk by 32% and cognitive decline by 27%.
The Future Is Changing-But Not Fast Enough
There’s progress. The FDA now requires black box warnings on opioids and benzodiazepines. Some hospitals are using AI-powered clinical tools that flag dangerous combinations before a prescription is even written. By 2025, most major electronic health systems will have mandatory alerts for these combinations.
But until then, the burden is on you. You’re the only one who knows everything you’re taking. You’re the only one who can ask the hard questions. And you’re the only one who can say no to a prescription that doesn’t feel right.
Combining sedatives isn’t just risky. It’s a silent killer. And the people most at risk aren’t the ones you expect. They’re the ones quietly taking their pills, hoping to feel better-without realizing they’re walking a tightrope over a cliff.
What to Do If Someone Shows Signs of Overdose
If someone is breathing fewer than 8 times a minute, is unresponsive, or has blue lips or fingernails:
- Call emergency services immediately.
- If you have naloxone (Narcan), give it-even if opioids aren’t confirmed. It won’t hurt if they’re not involved.
- Stay with them. Keep them awake if possible. Lay them on their side to prevent choking.
- Don’t give them coffee, cold showers, or let them “sleep it off.” Those don’t work. Only medical help does.
Can I safely take one benzodiazepine and one sleep medication together?
No. Even two sedatives from the same class-like a benzodiazepine and a non-benzodiazepine sleep aid such as zolpidem-can combine to dangerously slow your breathing. The risk isn’t just theoretical. Emergency rooms see this exact mix all the time, and it’s one of the leading causes of accidental overdose in people over 50.
Are herbal sleep aids like melatonin or valerian root safe to mix with prescription sedatives?
Melatonin is generally low-risk on its own, but valerian root can double the effect of benzodiazepines and other CNS depressants. Even natural doesn’t mean safe. Many people don’t realize herbal supplements can interact with medications. Always tell your doctor about every supplement you take.
Why do doctors keep prescribing these combinations if they’re so dangerous?
Doctors often treat symptoms one at a time, not the whole person. A patient with pain, anxiety, and insomnia might get three different prescriptions from three different specialists. No one connects the dots. Many doctors also assume patients aren’t drinking alcohol or taking OTC meds. Without full transparency, it’s easy to miss the danger.
Is it safe to take sedatives only on weekends or when I’m really stressed?
No. Sedatives don’t care if you take them daily or just occasionally. The risk of respiratory depression doesn’t disappear on weekends. In fact, people who take them only on weekends are often less likely to warn their doctors-and more likely to mix them with alcohol, which makes the danger even higher.
Can I just stop taking my sedatives if I’m worried?
Don’t quit cold turkey. Stopping benzodiazepines or opioids suddenly can cause seizures, severe anxiety, or even death. Talk to your doctor about a safe tapering plan. Deprescribing should be slow and supervised. It’s not about quitting-it’s about replacing dangerous combinations with safer, sustainable options.


14 Comments
Audrey Crothers
December 12, 2025This hit me hard. I’ve been taking Xanax and melatonin for years, thinking it was harmless. Now I’m terrified. I didn’t know valerian root could double the effect. I’m calling my doctor tomorrow. 😳
Adam Everitt
December 14, 2025so like… if the brain is a car, then sedatives are like stomping on the brake pedal with both feet, a knee, and your weird uncle’s elbow? kinda makes sense. kinda. i dunno man. 🤷♂️
wendy b
December 14, 2025It is deeply concerning that the medical establishment continues to operate in silos, perpetuating polypharmacy as a default intervention strategy rather than adopting a holistic, systems-based approach to patient care. The lack of pharmacovigilance integration in EHRs is not merely an oversight-it is a systemic failure of clinical governance.
Nathan Fatal
December 15, 2025Let’s be real: this isn’t about bad doctors or lazy patients. It’s about a healthcare system that rewards volume over vigilance. Doctors get paid to prescribe, not to pause and ask, ‘Is this actually helping?’ And patients? They’re told to trust the system. But when your meds are quietly shutting down your breathing, trust doesn’t save you. Knowledge does. Read this post again. Then talk to your doctor. No excuses.
nikki yamashita
December 16, 2025You’re not alone. I was in the same boat. Now I do CBT for sleep and yoga for anxiety. No pills. Better sleep. Better mood. Seriously, try it. You got this 💪
sandeep sanigarapu
December 17, 2025Respectfully, this is a global issue. In India, many elderly patients take multiple sedatives without awareness. The cultural stigma around mental health prevents open dialogue. Education must begin at the community level. A simple pamphlet in local languages can save lives.
Robert Webb
December 18, 2025I’ve seen this happen to my dad. He was on oxycodone for back pain, zolpidem for sleep, and a little wine every night to ‘take the edge off.’ He didn’t think it was a problem because ‘he followed the prescriptions.’ Then one night, he didn’t wake up. Not because of an overdose-he was just ‘too tired.’ They found his oxygen levels at 82%. He’s okay now, but it changed everything. If you’re taking more than one CNS depressant, even if it’s ‘just a little,’ please, please, please get a full med review. It’s not paranoia. It’s survival.
Rob Purvis
December 19, 2025Wait-so alcohol + benzos + sleep meds = triple threat? And people think it’s ‘just one glass’? I’ve seen ER reports where people died from this exact combo. It’s not a myth. It’s a statistic. And it’s happening every single day. Please, if you’re reading this and you’re doing this-stop. Don’t wait for a scare. Just stop. And tell your doctor. No judgment. Just life.
Laura Weemering
December 20, 2025…and yet, the pharmaceutical industry continues to profit from this. Who benefits? Not you. Not your grandma. The corporations. The FDA’s black box warnings? A PR move. The real fix? Ban all sedative combos. Period. And hold doctors accountable. This isn’t ‘unintended consequence’-it’s corporate negligence dressed up as ‘standard of care.’
Stacy Foster
December 22, 2025They’re lying to us. The government knows. The doctors know. They’re letting us die slowly so they can sell us more pills. And the EHRs? They’re coded to ignore these interactions on purpose. It’s all part of the Great Pharma Cover-Up. Wake up. This isn’t medicine. It’s mass poisoning.
Reshma Sinha
December 22, 2025As a clinical pharmacist, I see this daily. Polypharmacy in elderly patients is epidemic. Deprescribing isn’t just ‘reducing meds’-it’s restoring autonomy. We need mandatory interdisciplinary reviews for patients on ≥3 CNS depressants. It’s not optional. It’s ethical.
Lawrence Armstrong
December 22, 2025My cousin OD’d on this combo. I gave him Narcan. He lived. But he still takes the pills. I don’t know what to do anymore. 😔
Donna Anderson
December 23, 2025im so glad i read this. i was gonna take my sleeping pill after wine tonight… now im not. thank u. seriously. 🙏
Nathan Fatal
December 23, 2025You’re welcome. That’s exactly why I wrote this. One person changing one habit can save a life. You just did. Now go tell someone else.