When you're taking lithium for bipolar disorder, even small changes in your body can push you into dangerous territory. Lithium isn't like most medications. It works in a very narrow range-too little and it doesn't help your mood; too much and it can cause seizures, kidney damage, or even death. The problem isn't just the drug itself. It's what you take with it, what you eat, how much water you drink, and even the weather. This isn't theoretical. People have died from lithium toxicity after taking a common painkiller or starting a water pill without knowing the risk.
Why Lithium Is So Sensitive
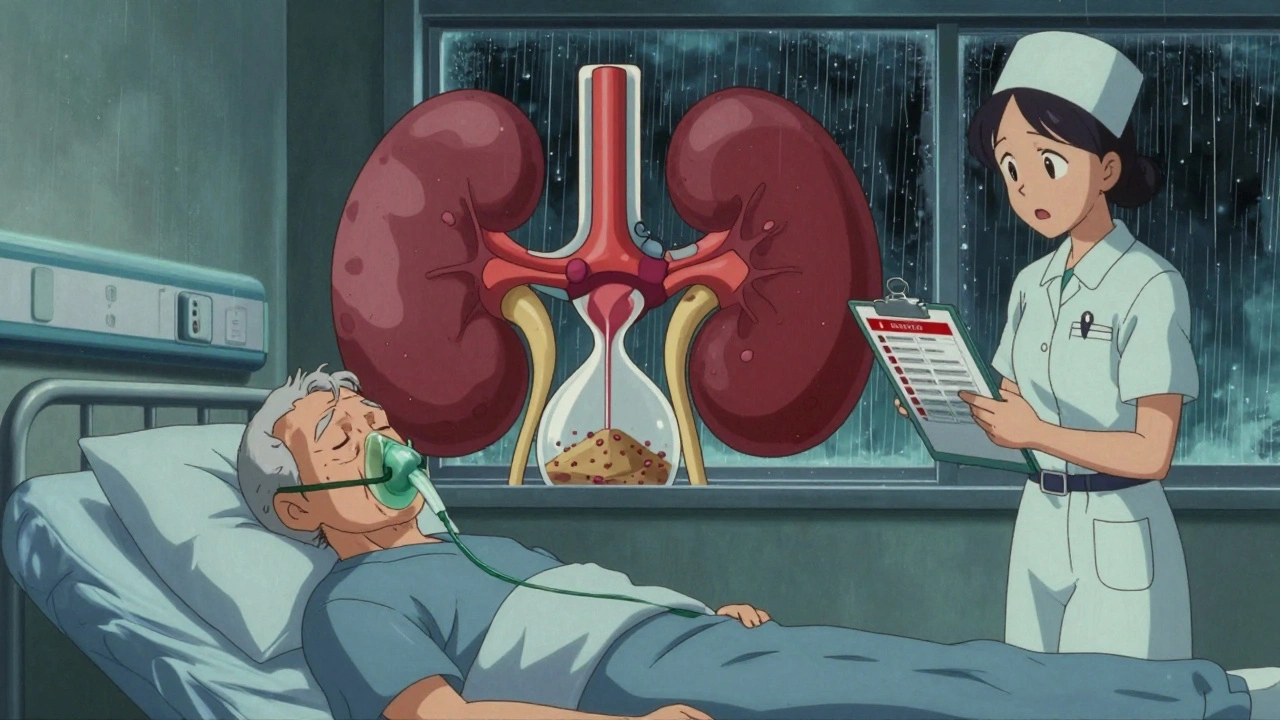
Lithium is cleared from your body almost entirely by your kidneys. About 95% of it leaves your system unchanged in your urine. That means anything that affects how well your kidneys work can change your lithium levels fast. Your kidneys don’t just filter blood-they also reabsorb lithium depending on how much salt and water is in your body. If your kidneys slow down, lithium builds up. If you lose fluids, lithium concentrates in your blood. It’s that simple, and that dangerous.Therapeutic levels are between 0.6 and 1.2 mmol/L. Go above 1.5 and you’re in the danger zone. Above 2.0 and you’re at risk of life-threatening toxicity. And it doesn’t take much to cross that line. A single dose of ibuprofen, a few days of not drinking enough water, or even eating less salt can push you over.
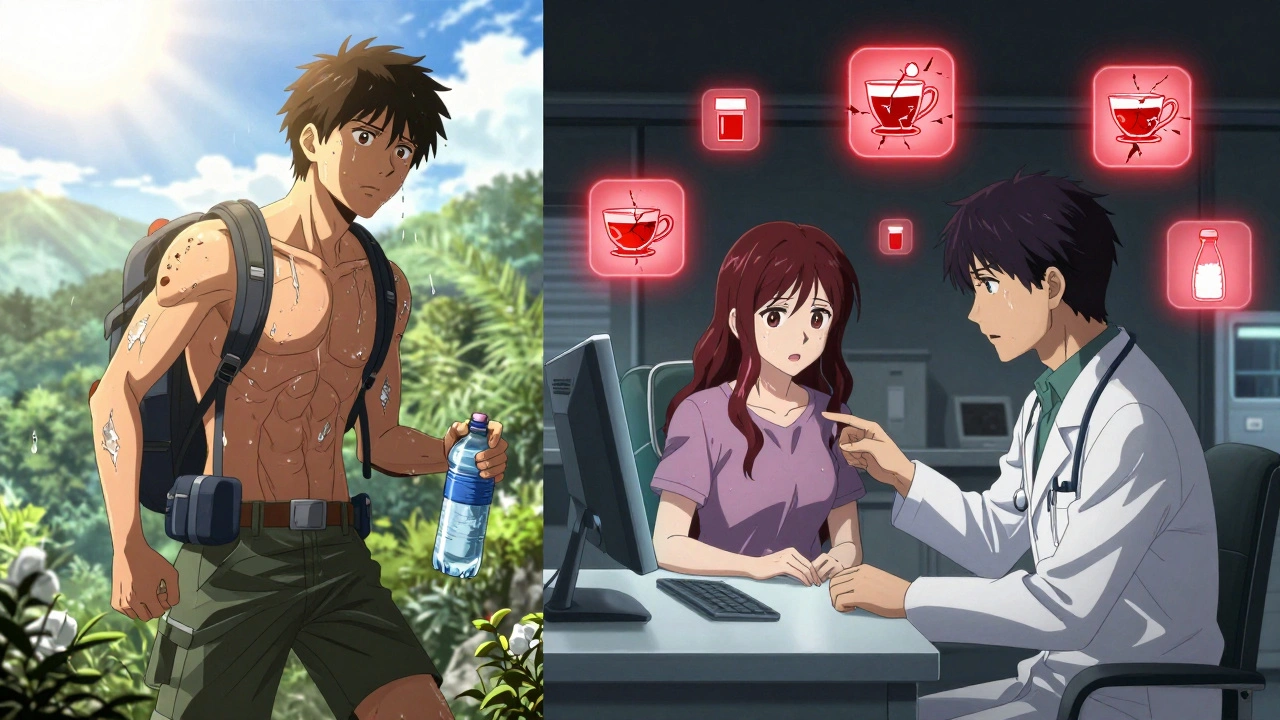
NSAIDs: The Silent Threat
Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, naproxen, and diclofenac are some of the most common medications people take for headaches, back pain, or arthritis. But for someone on lithium, they’re a red flag. These drugs block enzymes in the kidneys called cyclooxygenases, which help maintain blood flow to the filtering units. When those enzymes are blocked, kidney filtration drops by 25 to 50%. That means lithium isn’t flushed out as quickly-and levels rise.Not all NSAIDs are the same. Indomethacin can spike lithium levels by 30 to 60%. Ibuprofen? Around 25 to 40%. Celecoxib is a bit safer, but still risky, with increases of 15 to 30%. The effect usually shows up within the first week of taking the NSAID. It’s not rare. In fact, studies show NSAID use is one of the top reasons lithium toxicity occurs in older adults.
One fatal case in New Zealand involved a 72-year-old woman on lithium and an ACE inhibitor for blood pressure. She started taking an NSAID for joint pain. Her lithium levels weren’t checked for months. She ended up in the hospital with seizures and died. Her story isn’t unique. Many doctors don’t realize how quickly this interaction can turn deadly-especially in people over 65, who are 3.2 times more likely to experience lithium toxicity.
Diuretics: Water Pills That Can Dry You Out
Diuretics are another major concern. They’re prescribed for high blood pressure, heart failure, or swelling. But they interfere with lithium in two ways: by reducing kidney filtration and by changing how much sodium your body holds.Thiazide diuretics like hydrochlorothiazide are the worst offenders. They can increase lithium levels by 25 to 50% within 7 to 10 days. That’s enough to push someone from a safe level into toxicity. Loop diuretics like furosemide (frusemide) are less risky, but still dangerous-they can raise lithium by 10 to 25%. Even potassium-sparing diuretics like spironolactone have unpredictable effects.
Here’s the twist: some diuretics actually lower lithium levels. Osmotic diuretics like mannitol and carbonic anhydrase inhibitors like acetazolamide increase urine output without reducing kidney filtration. That means lithium gets flushed out faster, which can make your mood unstable. So it’s not just about avoiding diuretics-it’s about knowing which ones are safe and which aren’t.
And don’t forget herbal diuretics. Products marketed as “natural” weight-loss teas or supplements often contain ingredients like dandelion, parsley, or hibiscus. These can cause dangerous lithium spikes through dehydration. People think “natural” means safe. It doesn’t.
Dehydration: The Hidden Trigger
You don’t need to be sick to be at risk. Even mild dehydration-losing just 2 to 3% of your body weight in water-can raise lithium levels by 15 to 25%. That’s the equivalent of skipping water all day after a walk, flying long-haul, or having a stomach bug.When you’re dehydrated, your blood volume drops. Your kidneys respond by holding onto more sodium-and lithium rides along with it. You end up with more lithium in less fluid. That’s why doctors tell people on lithium to drink plenty of water, especially in hot weather, during illness, or after exercise. It’s not a suggestion. It’s a safety rule.
And salt matters too. If you suddenly cut back on salt-maybe you’re trying to eat healthier-your lithium levels can climb. Eating less sodium by 20 to 30 mmol per day can increase lithium concentration by 10 to 20%. On the flip side, eating more salt can lower lithium levels, which might make your mood worsen. Consistency is key. Don’t change your salt intake suddenly. Keep your diet steady.
What to Do If You Need Pain Relief or a Diuretic
Avoiding NSAIDs and diuretics isn’t always possible. Many people need them. The goal isn’t fear-it’s awareness and planning.- If you’re on lithium and need pain relief, talk to your doctor first. Acetaminophen (paracetamol) is usually the safest option. It doesn’t affect kidney filtration the way NSAIDs do.
- If a diuretic is necessary, your doctor might switch you to a loop diuretic like furosemide instead of a thiazide. But even then, you’ll need closer monitoring.
- Never start or stop any medication without telling your prescriber. That includes over-the-counter drugs, supplements, or herbal teas.
When co-use is unavoidable, here’s what works:
- Lower your lithium dose before starting the new drug.
- Check your lithium blood level within 5 to 7 days after starting the new medication.
- Repeat the test weekly for the first month.
- Watch for early signs of toxicity: diarrhea, dizziness, drowsiness, hand tremors, or blurred vision.
Many clinics now use electronic alerts to flag these interactions. But alerts aren’t foolproof. If your doctor didn’t check your lithium level after you started an NSAID, you’re at risk. Be your own advocate.
Who’s at Highest Risk?
Some people are more vulnerable than others:- People over 65-kidney function naturally declines with age.
- Those with kidney disease, heart failure, or diabetes.
- Anyone taking multiple medications that affect the kidneys.
- People who travel frequently or live in hot climates.
- Those who experience vomiting, diarrhea, or fever-any illness that causes fluid loss.
If you fit any of these categories, you need a plan. Ask your doctor for a written guide: what to avoid, when to check levels, what symptoms to watch for, and who to call if something feels off.
What to Do If You Think You’re Toxic
Early signs of lithium toxicity are easy to miss. They feel like the flu, fatigue, or stress:- Diarrhea (68% of early cases)
- Lightheadedness or dizziness (52%)
- Drowsiness or confusion (47%)
- Tremors in your hands
- Blurred vision or ringing in the ears
If you notice these, stop taking any new medications and drink water. But don’t wait. Call your doctor or go to the emergency room. Lithium toxicity can progress quickly. Seizures, coma, and permanent kidney damage are real risks.
There’s no antidote. Treatment is supportive: stopping lithium, IV fluids, and sometimes dialysis. The sooner you act, the better your chances.
Final Thoughts: Stay in Control
Lithium saves lives. But it demands respect. It’s not a medication you can take and forget about. You need to be active in your care. Know your numbers. Know your risks. Know what to avoid.Keep a list of all your medications-prescription, over-the-counter, and supplements. Bring it to every appointment. Tell every new doctor you’re on lithium. Drink water regularly, even if you’re not thirsty. Don’t change your salt intake without talking to your doctor. And if you’re ever unsure, err on the side of caution.
There’s no shame in asking questions. There’s only danger in staying silent.
Can I take ibuprofen if I’m on lithium?
It’s not recommended. Ibuprofen can raise lithium levels by 25-40%, increasing the risk of toxicity, especially in older adults or those with kidney issues. If you need pain relief, acetaminophen (paracetamol) is a safer choice. Always talk to your doctor before taking any NSAID.
How long does it take for NSAIDs to affect lithium levels?
Lithium levels can start rising within 2-3 days of starting an NSAID, with the full effect usually seen within 7-10 days. That’s why doctors recommend checking lithium blood levels within a week of starting a new NSAID and again weekly for the first month.
Do all diuretics raise lithium levels?
No. Thiazide diuretics like hydrochlorothiazide are the most dangerous and can raise lithium by 25-50%. Loop diuretics like furosemide cause smaller increases (10-25%). But osmotic diuretics (like mannitol) and carbonic anhydrase inhibitors (like acetazolamide) actually lower lithium levels, which can make your mood unstable. Always check with your doctor before starting any diuretic.
Can dehydration alone cause lithium toxicity?
Yes. Even mild dehydration-losing just 2-3% of your body weight in water-can increase lithium levels by 15-25%. This can happen during illness, after exercise, during long flights, or in hot weather. Drinking enough water is not optional-it’s part of your treatment plan.
Should I avoid salt if I’m on lithium?
No. Don’t cut back on salt unless your doctor tells you to. Reducing sodium intake can raise lithium levels by 10-20%. Eating too much salt can lower them, which might make your symptoms return. The key is consistency. Keep your salt intake steady-don’t suddenly go low-salt or high-salt.
How often should lithium levels be checked?
If you’re stable, checks every 3-6 months are typical. But if you start a new medication like an NSAID or diuretic, levels should be checked within 5-7 days and then weekly for the first month. After that, your doctor will decide if more frequent checks are needed based on your risk factors.
Are herbal diuretics safe with lithium?
No. Herbal diuretics-like dandelion, parsley, or green tea extracts in weight-loss teas-can cause dangerous lithium spikes through dehydration. They’re not regulated, and their effects aren’t studied in people on lithium. Avoid them entirely unless your doctor approves.
What should I do if I get sick with vomiting or diarrhea?
Stop taking lithium until you’ve spoken to your doctor. Vomiting and diarrhea cause rapid fluid loss, which can spike lithium levels. Drink small sips of water or electrolyte drinks. Don’t wait for symptoms to get worse-call your prescriber right away.






10 Comments
Norene Fulwiler
December 4, 2025I knew someone who went to the ER after taking Advil for a headache while on lithium. They didn’t even realize it was dangerous. I’ve been on lithium for 12 years and I keep a list of every med I take-prescription, OTC, even supplements-and I show it to every new doctor. It’s not paranoia, it’s survival.
Also, if you’re traveling, pack extra water. I once got stuck in a 10-hour flight delay in Phoenix and my tremors started. I drank two liters of water and called my psychiatrist. Don’t wait until you’re dizzy.
Lithium saved my life, but it’s not a passive drug. You gotta be its manager, not just its user.
Laura Saye
December 5, 2025The biochemical elegance of lithium’s renal handling is, in a way, tragically beautiful-its near-total dependence on glomerular filtration and sodium-dependent tubular reabsorption renders it exquisitely vulnerable to homeostatic perturbations.
It’s not merely a pharmacokinetic concern; it’s a metaphysical one. The body becomes a fragile vessel, and the mind, a prisoner of ion gradients. We are, in essence, electrochemical beings, and lithium reminds us of that with terrifying precision.
When you take a diuretic, you’re not just altering fluid volume-you’re rewriting the narrative of your neurochemistry. And no algorithm, no alert, no EHR flag can substitute for the quiet vigilance of self-awareness.
Perhaps the real toxicity isn’t the lithium-it’s the illusion of control we mistake for competence.
Michael Dioso
December 7, 2025Ugh, another ‘lithium scare’ post. Look, if you can’t handle a little ibuprofen, maybe you shouldn’t be on lithium at all. My cousin’s been on it for 20 years and he takes Aleve like candy. He’s fine. You people act like this drug is radioactive.
And don’t even get me started on ‘herbal diuretics.’ Dandelion tea? That’s what your grandma drank for bloating. You think Big Pharma is hiding something? Nah, you’re just overthinking it.
Also, salt? Who cares? Eat what you want. If your levels go up, get them checked. Simple. Stop scaring people with this doomsday nonsense.
Juliet Morgan
December 9, 2025I’m so glad this exists. I was diagnosed 3 years ago and I was terrified. I didn’t know what to ask my doctor. This post? It’s the first thing I showed my mom.
My biggest fear was forgetting to drink water when I was stressed. Now I have a water bottle with time markers on it. I drink before I’m thirsty. I even set alarms.
You’re not weak for needing this info. You’re smart for seeking it. Keep going. You’re not alone.
William Chin
December 9, 2025It is imperative to underscore the clinical significance of renal clearance dynamics in the context of lithium pharmacokinetics. The sodium-lithium countertransport mechanism in the proximal tubule is a well-documented pathway through which homeostatic deviations precipitate toxicological outcomes.
Furthermore, the concomitant administration of nonsteroidal anti-inflammatory agents constitutes a pharmacodynamic interaction of paramount concern, particularly in geriatric populations exhibiting age-related reductions in glomerular filtration rate.
It is the professional responsibility of the prescribing clinician to ensure comprehensive patient education regarding these interactions, as failure to do so may constitute a breach of the standard of care.
Katie Allan
December 9, 2025I’ve worked with patients on lithium for over 15 years. The most dangerous thing isn’t the drug-it’s the silence. People don’t tell their doctors about the cold medicine they took, or the weight-loss tea, or the extra coffee because they think it’s ‘just a little.’
But it’s not just a little. It’s life or death.
Please, if you’re on lithium, make a list. Write it down. Bring it to every appointment. Even if you think it’s not important. It is.
You’re not being difficult. You’re being responsible.
Deborah Jacobs
December 11, 2025Lithium is like a high-strung cat that only purrs when you pet it just right. Too hard? It hisses. Too soft? It walks away. And if you forget to feed it? It knocks over the whole damn shelf.
I used to think drinking less water on hot days was ‘being tough.’ Then I got dizzy after a hike and my hands shook like I’d had three espressos. My doc said my lithium level had jumped to 1.7. I cried. Not from fear-from guilt.
Now I carry a water bottle everywhere. I eat my salt. I don’t touch NSAIDs. And I talk to my therapist about how weird it feels to be this careful about my own body.
It’s not control. It’s love.
James Moore
December 11, 2025Let me tell you something-this whole ‘lithium is dangerous’ thing is just another way for the medical-industrial complex to profit off fear! You think your doctor really cares? They get paid to prescribe, not to explain! And don’t get me started on the FDA-they’re in bed with Big Pharma!
And why do they say acetaminophen is ‘safe’? Because it’s cheaper! Ibuprofen is natural! It’s from willow bark! But they patent acetaminophen and make billions!
My uncle in Ohio took lithium for 40 years, drank beer, ate salted peanuts, took Advil every Sunday-he lived to 89! So what’s the real danger? The drug? Or the lies they feed you to keep you scared and dependent?
Wake up! Question everything! The truth is out there-just not in your doctor’s office!
Lucy Kavanagh
December 13, 2025Did you know the government puts lithium in the water supply to calm people down? That’s why they’re so scared you’ll take NSAIDs-they don’t want you to realize how much control they have!
My neighbor’s cousin’s ex-boyfriend’s therapist said the FDA knows NSAIDs cause lithium toxicity but covers it up because they want you to stay dependent on psychiatry.
And the salt thing? That’s a trick. Salt makes you thirsty so you drink more water, which flushes out the lithium… but only if you’re not being watched. They track your water intake through your phone.
Don’t trust anyone. Not your doctor. Not this post. Not even me. Just… stay inside. And drink bottled water. Only from glass bottles. Plastic is contaminated.
Stephanie Fiero
December 13, 2025OMG YES. I was on a road trip and forgot to drink water for 12 hours. Started feeling weird, thought I was getting sick. Called my doc at 2am. They told me to go to ER. My level was 1.8. They pumped me full of IV fluids.
Now I have a little card in my wallet that says ‘I’m on lithium. Do not give me NSAIDs or diuretics.’ I show it to EMTs. I even gave one to my barista so she knows not to give me the ‘herbal detox’ tea.
It’s embarrassing but worth it. I’m alive because I asked for help.
Also, I keep a journal. If I feel off, I write it down. Then I show it to my doctor. It’s not just meds. It’s my body talking. I listen.