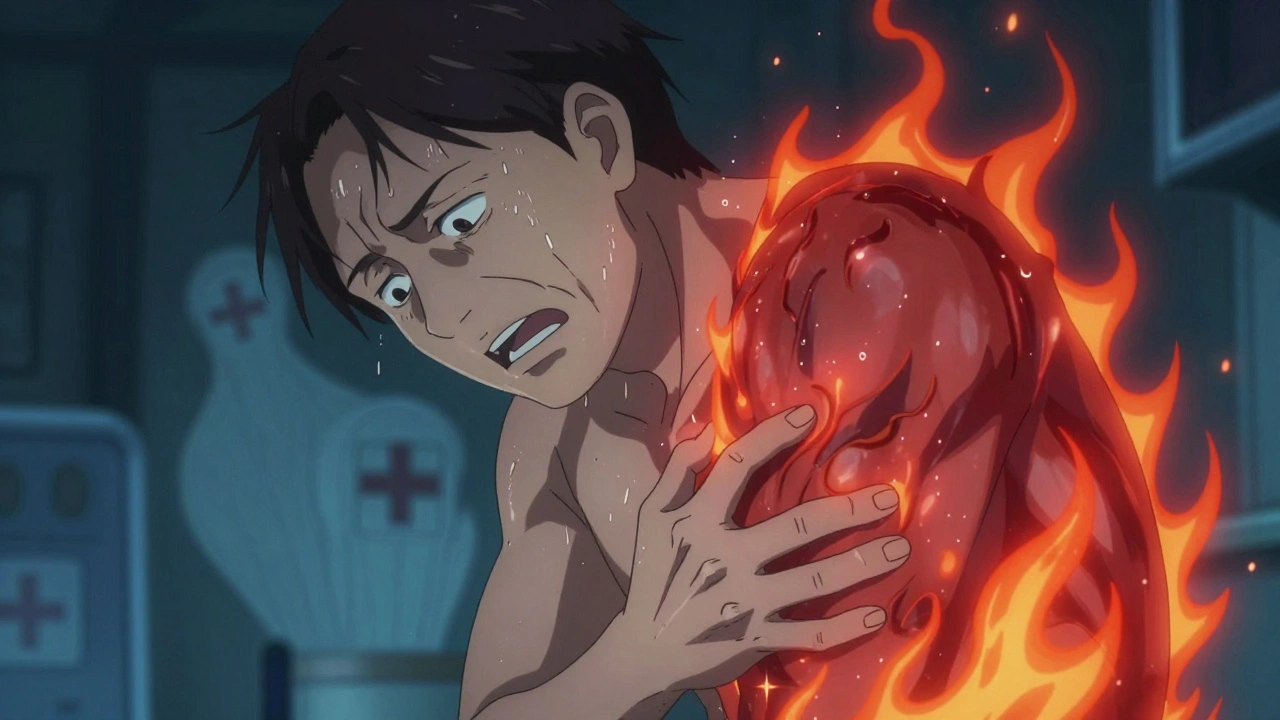
Shingles isn’t just a rash. It’s a sharp, burning pain that can turn your skin into something that feels like it’s on fire-even the lightest touch hurts. If you’ve ever had it, you know it doesn’t just go away after a few days. For many, the pain lingers for months, sometimes years. That’s why getting treatment fast matters more than almost anything else.
What Causes Shingles?
You didn’t catch shingles from someone else. You already had the virus inside you-chickenpox. Years later, the varicella-zoster virus, which stayed quiet in your nerve tissue, wakes up. It travels along the nerve pathways and bursts out as a painful, blistering rash, usually on one side of your body or face. It’s not contagious like chickenpox, but if you’ve never had chickenpox or the vaccine, you can catch the virus from someone with shingles-and then get chickenpox, not shingles.
The risk goes up sharply after 50. One in three people will get it in their lifetime. People with weak immune systems-those on chemotherapy, with HIV, or taking long-term steroids-are at even higher risk. And the older you are, the worse it tends to be.
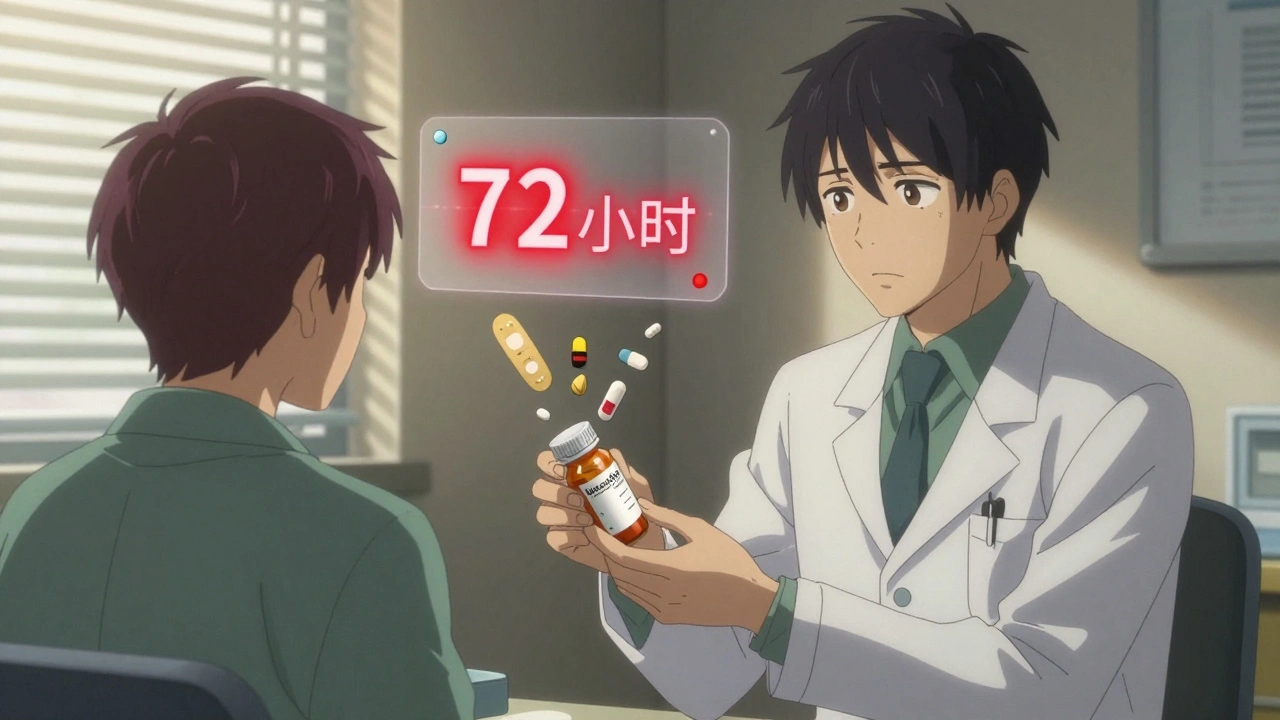
Why Timing Is Everything With Antivirals
Antiviral drugs don’t cure shingles. But they can stop it from getting worse. The three main ones-acyclovir, famciclovir, and valacyclovir-work best when started within 72 hours of the first sign of rash. After that, the virus has already spread too far in your nerves. Delay treatment even by a day or two, and you lose a lot of the benefit.
Here’s how they’re typically dosed:
- Valacyclovir (Valtrex): 1,000 mg three times a day for 7 days
- Famciclovir (Famvir): 500 mg three times a day for 7 days
- Acyclovir (Zovirax): 800 mg five times a day for 7 to 10 days
Valacyclovir is often preferred because it’s easier to take-fewer pills per day. Studies show it reduces acute pain by about 30% and heals blisters 2 to 3 days faster than no treatment. Some data suggests it may do slightly better than acyclovir at easing pain, but all three are similarly effective at clearing the rash.
Here’s the catch: if you wait more than 72 hours, the benefit drops off fast. That’s why if you feel tingling, burning, or itching on one side of your body-especially before the rash appears-don’t wait. Call your doctor right away. Even if the rash hasn’t shown up yet, early treatment can make a real difference.
Can Antivirals Prevent Long-Term Pain?
This is where things get messy. Many people hope antivirals will stop post-herpetic neuralgia (PHN)-the nerve pain that sticks around after the rash heals. But the evidence isn’t clear-cut.
A major Cochrane review says acyclovir doesn’t reduce PHN at six months. Other studies, including one published in 2011, say early antiviral use lowers the risk. And real-world patient reports? About 62% of people on PatientsLikeMe say they avoided chronic pain because they started treatment early. But 38% still got PHN.
The truth? Antivirals help reduce the severity and length of the initial outbreak, which in turn lowers your chances of PHN. But they’re not a guarantee. People over 60 have a 30% chance of developing PHN, even with treatment. That’s why prevention-like the Shingrix vaccine-is so important. It cuts shingles risk by over 90% and makes outbreaks milder if they do happen.
Managing the Pain: Beyond Antivirals
Antivirals treat the virus. But they don’t fix the nerve damage. That’s where pain management comes in-and it needs to be multi-layered.
Anticonvulsants like gabapentin (Neurontin) or pregabalin (Lyrica) calm overactive nerves. Doctors usually start low-300 mg of gabapentin once a day-and slowly increase to 1,800-3,600 mg daily. Side effects? Drowsiness, dizziness, swelling. But for many, it’s the only thing that brings relief.
Tricyclic antidepressants like amitriptyline (25-75 mg at night) work wonders for nerve pain, even if you’re not depressed. They help regulate pain signals in the brain. Many patients report better sleep and less burning after just a few days.
Topical treatments are gentler and great for localized pain:
- Lidocaine patches (5%): Apply for 12 hours on, 12 off. Safe for daily use. No systemic side effects.
- Capsaicin cream (0.075%): Made from chili peppers. It burns at first-then numbs. Use 3-4 times daily. It takes weeks to work, but some find it life-changing.
For severe pain in the first week, doctors may prescribe short-term opioids. But they’re not great for nerve pain and carry addiction risks. Most experts avoid them unless absolutely necessary.
Shingles and the Eyes: A Hidden Danger
If the rash appears near your eye-even just on your forehead-you’re at risk for herpes zoster ophthalmicus (HZO). This can lead to corneal damage, glaucoma, or even vision loss.
The Zoster Eye Disease Study (ZEDS), published in late 2023, found something groundbreaking: long-term, low-dose valacyclovir (500 mg daily) reduced new or worsening eye disease by 26% at 18 months. It also cut flare-ups by 30% and lowered the need for pain meds like gabapentin by 22-25%.
That’s why experts now recommend extended antiviral therapy for anyone with eye involvement. It’s not standard everywhere yet-but it should be. If you have shingles near your eye, ask your doctor about long-term treatment. Don’t wait until vision problems start.
What About Steroids?
Some doctors add corticosteroids like prednisone to antivirals, hoping to reduce inflammation and pain faster. The idea makes sense. But studies are mixed. The Mayo Clinic says it’s controversial because steroids weaken your immune system-exactly what you don’t want when fighting a viral infection.
Right now, steroids aren’t routinely recommended. But in severe cases, especially with intense pain or facial swelling, some specialists still use them short-term. It’s a personal call between you and your doctor.
Cost and Practicality
A 7-day course of antivirals costs $85-$150 without insurance. But early treatment saves money in the long run. One study found it cuts overall healthcare costs by $487 per person by preventing hospital visits, nerve pain meds, and complications.
Most insurance covers valacyclovir and famciclovir. Generic acyclovir is cheaper but harder to take because of the frequent dosing. If cost is a barrier, ask your doctor about samples or patient assistance programs.
What to Do If You Think You Have Shingles
Don’t guess. Don’t wait. Here’s your action plan:
- Look for pain, burning, tingling, or itching on one side of your body or face-before the rash appears.
- Check for red patches or fluid-filled blisters in a band-like pattern.
- Call your doctor immediately. Say: “I think I have shingles.”
- If the rash is near your eye, go to an eye doctor or ER right away.
- Start antivirals within 72 hours if prescribed.
- Use pain relief as directed-don’t tough it out.
- Keep the rash clean and covered to avoid infection.
Most people recover fully. But the pain can linger. That’s why early action isn’t just helpful-it’s essential.
Prevention Is the Best Treatment
The Shingrix vaccine is the most effective tool we have. It’s two shots, given 2-6 months apart. It’s over 90% effective at preventing shingles and works well even in people over 70. The CDC recommends it for all adults 50 and older-even if you’ve had shingles before or got the old Zostavax vaccine.
It’s not a cure. But it’s the closest thing we have to one.
Can shingles go away without antivirals?
Yes, shingles can resolve on its own in 3 to 5 weeks. But without antivirals, the pain is usually worse, the rash takes longer to heal, and your risk of long-term nerve pain (PHN) goes up. Antivirals don’t cure it, but they make the experience significantly less severe.
Is shingles contagious?
You can’t catch shingles from someone else. But if you’ve never had chickenpox or the chickenpox vaccine, you can catch the varicella-zoster virus from a person with shingles-and then develop chickenpox. The virus spreads through direct contact with the open blisters. Once the rash crusts over, you’re no longer contagious.
How do I know if I have post-herpetic neuralgia?
If the pain lasts more than 90 days after the shingles rash has healed, you likely have PHN. It feels like burning, stabbing, or electric shocks in the same area where the rash was. The skin may be extremely sensitive-even light clothing can hurt. PHN is more common in people over 60 and those with severe initial pain.
Why is valacyclovir preferred over acyclovir?
Valacyclovir is converted to acyclovir in the body but is absorbed better and lasts longer. That means you take it only three times a day instead of five. Fewer pills mean better adherence. Studies show it reduces pain slightly better than acyclovir, though both clear the rash equally well.
Can I use over-the-counter painkillers for shingles?
NSAIDs like ibuprofen or acetaminophen can help with mild discomfort and fever, but they don’t touch nerve pain. For the deep, burning pain of shingles, OTC painkillers usually aren’t enough. You’ll need prescription nerve pain meds like gabapentin or amitriptyline.
Should I get the Shingrix vaccine after having shingles?
Yes. Having shingles once doesn’t protect you from getting it again. The CDC recommends Shingrix for everyone 50 and older, even if you’ve had shingles. Wait until the rash has fully healed before getting vaccinated-usually about a month after symptoms start.
Are there natural remedies that work for shingles?
Cool compresses, oatmeal baths, and calamine lotion can soothe itching and discomfort. Some people try lysine supplements or essential oils, but there’s no strong evidence they help. Antivirals and prescribed pain meds are the only treatments proven to change the course of the disease. Don’t skip medical treatment for unproven remedies.




11 Comments
Mark Curry
December 4, 2025Been there. Got the rash, the pain, the sleepless nights. Started antivirals day two-still hurt like hell, but at least the blisters dried up in a week. PHN? Lucky me, I dodged it. Shingrix saved my life after. Don’t wait. Just get the shot.
Michael Dioso
December 4, 2025Oh please. You think antivirals are magic? I had shingles in ’19 and skipped them. Took 6 weeks, yeah-but I didn’t need some lab-made chemical to tell my body how to heal. Nature’s got a plan. Modern medicine just likes to sell pills.
Kylee Gregory
December 6, 2025I appreciate the breakdown on pain meds. Gabapentin made me feel like a zombie, but it was the only thing that stopped the electric shocks. I wish more doctors talked about the trade-offs instead of just prescribing. Also-capsaicin cream? Holy hell, it burned like Satan’s breath… but after two weeks? Worth it.
Annie Grajewski
December 7, 2025so like… if you’re over 50 and didn’t get shingrix… you’re basically just a walking time bomb? 😅
James Moore
December 8, 2025Let’s be real-this whole ‘shingles is just chickenpox coming back’ narrative is a corporate lie designed to sell vaccines. The varicella-zoster virus has been in our DNA since before Columbus. It’s not ‘waking up’-it’s being triggered by stress, toxins in the water, 5G towers, or government mind-control chips. And you think a $150 pill fixes that? Wake up. The CDC’s been lying to you since ’02. I’ve had three outbreaks. No antivirals. Just cold showers, raw garlic, and prayer. I’m 71. Still standing.
Rupa DasGupta
December 10, 2025OMG I had shingles and my ex sent me a meme like ‘lol u got the pain dragon’ and then ghosted me… I cried for 3 days 😭😭😭
aditya dixit
December 10, 2025Valacyclovir’s dosing schedule is indeed more practical. I’ve seen patients miss doses with acyclovir simply because five times a day is unsustainable-especially for elderly or working individuals. Adherence is a silent factor in clinical outcomes. Also, the ZEDS study on long-term low-dose valacyclovir for ocular involvement is compelling. It’s not yet standard, but it should be. Prevention of corneal scarring is worth the cost.
Jimmy Jude
December 12, 2025EVERYONE IS WRONG. Shingles is not a virus-it’s your soul screaming because you’ve been living a lie. That burning pain? It’s the universe telling you to quit your job, forgive your mother, and start meditating. I healed mine with sound baths, crystal grids, and a 40-day juice cleanse. No pills. No doctors. Just vibes. If you’re still taking antivirals… you’re still asleep.
Lucy Kavanagh
December 13, 2025Did you know the FDA approved these antivirals because Big Pharma bribed the doctors? I have a cousin who works at the WHO-she says the 90% efficacy of Shingrix? Fabricated. The real stats are hidden. And that ‘eye study’? They only followed people for 18 months-what about 5 years? They don’t want you to know that the vaccine causes neurological damage in 1 in 10,000. But hey, go ahead and get it. I’ll be over here, drinking apple cider vinegar and watching the skies.
Mark Ziegenbein
December 15, 2025It’s fascinating how society has pathologized a natural immune response and turned it into a pharmaceutical goldmine. The fact that we’re still debating whether steroids help or hurt reveals a deeper truth-we don’t understand neuroinflammation. We just throw molecules at it and call it medicine. Valacyclovir reduces viral replication. But does it address the central sensitization of the dorsal root ganglia? No. That’s why gabapentin remains the real hero. And yet, no one talks about the epigenetic triggers. Stress. Trauma. The collapse of social cohesion. Shingles is the body’s protest against modern life.
Laura Saye
December 16, 2025I’ve been managing PHN for 3 years. Gabapentin helped, but the lidocaine patches? Lifesaver. I apply them before bed. No more screaming into my pillow. I wish someone had told me earlier that nerve pain isn’t ‘all in your head’-it’s in your nerves. And yes, Shingrix is the best thing we’ve got. I got it after my outbreak. I’m not taking chances again. You’re not weak for needing help. You’re smart for asking for it.