The Magic of Misoprostol: A Game Changer in Cervical Ripening and Labor Induction
As an expecting mother, I know that the topic of labor induction and cervical ripening can be a bit overwhelming. There are so many different methods and medications, but one that has truly stood out to me is Misoprostol. Misoprostol has been a game-changer in the world of obstetrics, and I'm excited to share with you the benefits of this medication in cervical ripening and labor induction. In this article, we will discuss the following topics:
Understanding Misoprostol and how it works
First, it's important to understand what Misoprostol is and how it works. Misoprostol is a synthetic prostaglandin E1 analog, which means it mimics the effects of natural prostaglandins in the body. Prostaglandins play a crucial role in the process of labor, as they help to soften the cervix and stimulate uterine contractions. By using Misoprostol, we can effectively initiate this process when it is medically necessary to induce labor or prepare the cervix for delivery.
Efficiency and effectiveness of Misoprostol in cervical ripening
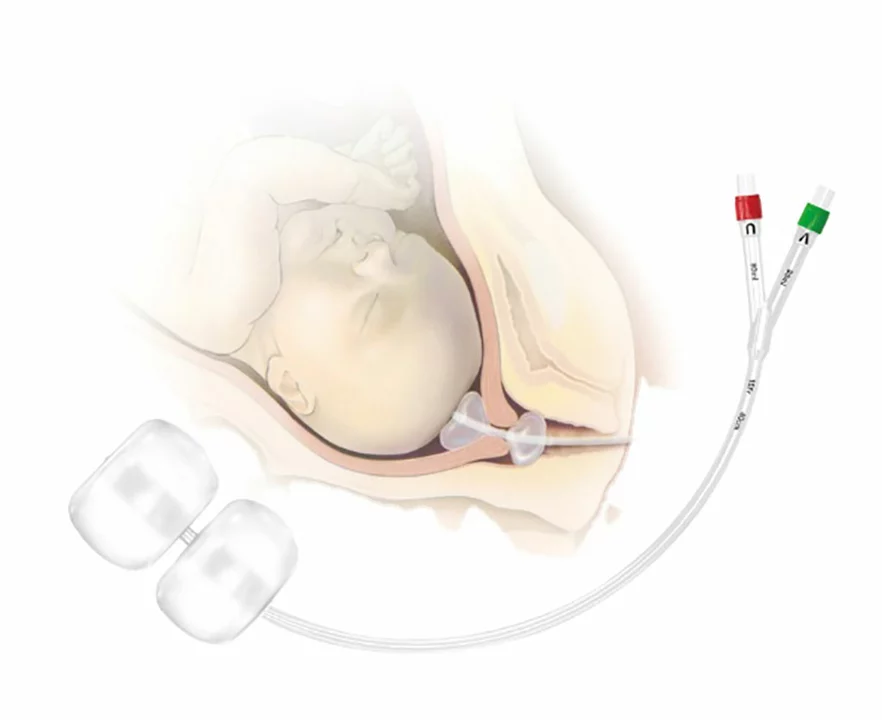
One of the most significant benefits of Misoprostol is its efficiency in ripening the cervix. Studies have shown that Misoprostol is more effective than other commonly used methods such as the use of a Foley catheter or the administration of dinoprostone. Furthermore, women who receive Misoprostol for cervical ripening often experience shorter times to active labor and delivery compared to other methods. This means that Misoprostol not only works well, but it also helps to speed up the process for expecting mothers.
Reduced need for additional interventions
Another important advantage of Misoprostol is that it reduces the need for additional interventions during labor. When Misoprostol is used for cervical ripening and labor induction, there is a decreased likelihood of requiring other methods such as oxytocin augmentation or the use of forceps or vacuum during delivery. This is not only beneficial for the mother's comfort but also for the overall safety and well-being of both the mother and baby during labor and delivery.
Lower risk of complications
Using Misoprostol for cervical ripening and labor induction also comes with a lower risk of complications compared to other methods. For example, there is a lower risk of uterine hyperstimulation, which is a condition where the uterus contracts too frequently and too strongly. This can lead to complications such as decreased fetal heart rate, placental abruption, and uterine rupture. By using Misoprostol, we can help to minimize these risks and ensure a safer labor and delivery for both mother and baby.
Cost-effectiveness of Misoprostol
Lastly, Misoprostol is a cost-effective option for cervical ripening and labor induction. This medication is less expensive than other commonly used methods such as dinoprostone or the insertion of a Foley catheter. By choosing Misoprostol, expecting mothers and their healthcare providers can help to reduce the financial burden associated with labor and delivery, making it a more accessible option for many families.
In conclusion, Misoprostol has proven to be a highly effective, safe, and cost-effective option for cervical ripening and labor induction. Its numerous benefits, such as efficiency, reduced need for additional interventions, lower risk of complications, and cost-effectiveness, make it a popular choice for expecting mothers and healthcare providers alike. As a mother-to-be, I feel confident in the use of Misoprostol to help ensure a smooth and safe labor and delivery for both myself and my baby.





19 Comments
diego suarez
May 29, 2023Thank you for sharing!
Eve Perron
June 3, 2023Reading through your post reminded me of how far obstetric practice has come, especially in the realm of pharmacologic cervical ripening; the introduction of misoprostol has truly reshaped our therapeutic arsenal. It is fascinating that a prostaglandin analog, once primarily used for gastric ulcer prophylaxis, now finds a pivotal role in labor induction. Multiple randomized controlled trials have demonstrated that misoprostol not only accelerates cervical effacement but also reduces the time to active labor compared with traditional agents such as dinoprostone. Moreover, the dosage flexibility-ranging from 25 µg to 50 µg administered vaginally-allows clinicians to tailor treatment to individual patient profiles, minimizing the risk of uterine hyperstimulation. Cost analysis consistently shows that misoprostol is markedly less expensive than its counterparts, a consideration that becomes especially salient in low-resource settings. Importantly, the side effect profile is relatively benign, with nausea and transient fever being the most commonly reported adverse events, and serious complications remaining rare. In addition, the ease of storage at room temperature eliminates the logistical challenges associated with temperature-sensitive preparations. When compared to mechanical methods like Foley catheter insertion, misoprostol offers a non‑invasive alternative that patients often prefer. The literature also suggests a reduced need for supplemental oxytocin, which can lower the overall intervention burden during labor. Ethical discussions have emerged around informed consent, emphasizing the necessity to discuss potential benefits and risks transparently. While some clinicians remain cautious due to the theoretical risk of uterine rupture, especially in women with prior cesarean deliveries, current evidence indicates that this risk is negligible when proper protocols are followed. Patient satisfaction scores tend to be higher when misoprostol is used, reflecting its efficacy and tolerability. As a community, we should continue to monitor emerging data, particularly regarding optimal dosing schedules for diverse populations. Ultimately, the integration of misoprostol into standardized labor induction pathways exemplifies evidence‑based medicine at its best. I appreciate you bringing this topic to light for expecting parents navigating their birth plans.
Josephine Bonaparte
June 9, 2023Solid points, and the data you cite really backs up the safety claims-no need for endless debate when the numbers speak for themselves.
Meghan Cardwell
June 15, 2023From a clinical workflow perspective, misoprostol streamlines the induction protocol by eliminating the need for serial cervical exams that are required with the Foley method, thereby freeing up nursing time and reducing patient discomfort.
stephen henson
June 21, 2023Love how this drug makes the whole process smoother 🙌
Manno Colburn
June 26, 2023i think its a great optoin but watch out for the dose. some docotrs use to high dose and cause problams.
Namrata Thakur
July 2, 2023It's wonderful to see a medication that is both affordable and effective-this can really help families who worry about medical costs.
Chloe Ingham
July 8, 2023Did you know that the pharmaceutical companies are hiding the true side‑effects? It's all a massive cover‑up, but misoprostol still wins because they can't control everything.
Mildred Farfán
July 14, 2023Oh great, another miracle drug-right, because everything with a fancy name is always flawless.
Danielle Flemming
July 20, 2023Honestly, reading this gave me hope! The blend of safety, speed, and cost‑effectiveness makes misoprostol a real lifesaver for many moms-to‑be, especially those juggling work and family budgets.
Anna Österlund
July 25, 2023While the enthusiasm is nice, let's not forget that over‑reliance on any single drug can backfire if protocols aren't followed.
Brian Lancaster-Mayzure
July 31, 2023Observational data also suggest that misoprostol reduces the overall length of hospital stay, which can be a significant factor for both patients and healthcare systems.
Erynn Rhode
August 6, 2023When we talk about the pharmacodynamics of misoprostol, it's essential to note that its rapid absorption via the vaginal mucosa leads to a more predictable cervix‑softening effect compared to oral routes. This bioavailability advantage is supported by multiple phase‑III trials that recorded a mean reduction of 6‑8 hours in induction‑to‑delivery intervals. Coupled with its low cost-often less than a few dollars per dose-misoprostol presents a compelling case for inclusion in universal prenatal care guidelines. Yet, the discourse must also address the nuanced risk of uterine tachysystole, especially when administered in high‑dose regimens. Clinicians are urged to adhere to evidence‑based dosing protocols, typically 25 µg every 4‑6 hours, to mitigate such concerns. The ease of storage and minimal refrigeration requirements further enhance its suitability for remote or under‑resourced clinics, where cold chain logistics pose a barrier to other prostaglandins. From a patient‑centered perspective, the non‑invasive nature of vaginal administration is often preferred over mechanical methods, leading to higher satisfaction scores in recent surveys. These multi‑dimensional benefits underscore why misoprostol is not merely a stop‑gap measure but a cornerstone of modern obstetric practice.
Rhys Black
August 12, 2023One must, of course, recognize the elegance of a drug that balances potency with simplicity-though, as with all medical interventions, the devil resides in the details of proper application.
Abhishek A Mishra
August 18, 2023Glad to see such clear information; it really helps demystify the process for expectant parents.
Jaylynn Bachant
August 23, 2023It's refreshing to see an honest appraisal-no hype, just facts.
Anuj Ariyo
August 29, 2023Overall, misoprostol's profile aligns well with the goals of safe, efficient, and accessible obstetric care.
Tom Lane
September 4, 2023Let's keep pushing for broader adoption where appropriate; every mom deserves the best options available.
Darlene Young
September 10, 2023Agreed-standardizing protocols will ensure that the benefits you outlined become the norm, not the exception.