Why Nighttime Is the Riskiest Time for Medication Errors
It’s 3 a.m. You’ve been on duty for 14 hours. Your eyes feel heavy. The IV pump beeps. You grab the wrong vial. One mistake. One tired moment. And suddenly, a patient’s safety is at risk.
This isn’t hypothetical. In hospitals across Australia, the U.S., and Europe, medication safety at night is a silent crisis. Research shows that errors spike during night shifts-not because staff are careless, but because human biology fights back. When you’re tired, your brain doesn’t work the same way. Memory slips. Focus fades. Even simple tasks like reading a label or checking a dosage become risky.
A 2023 review of 38 global studies found that 82% of medication errors and near-misses were tied to fatigue. Nurses on night shifts make 38% more mistakes than those working days. The reason? Sleep deprivation cuts cognitive performance by 25-30%. That’s like having a blood alcohol level of 0.05%-legally impaired in many countries.
What Happens to Your Brain When You’re Sleep-Deprived
Your brain doesn’t just get "a little slower" when you haven’t slept. It starts failing in predictable ways.
- Short-term memory drops-so you forget what dose you just gave.
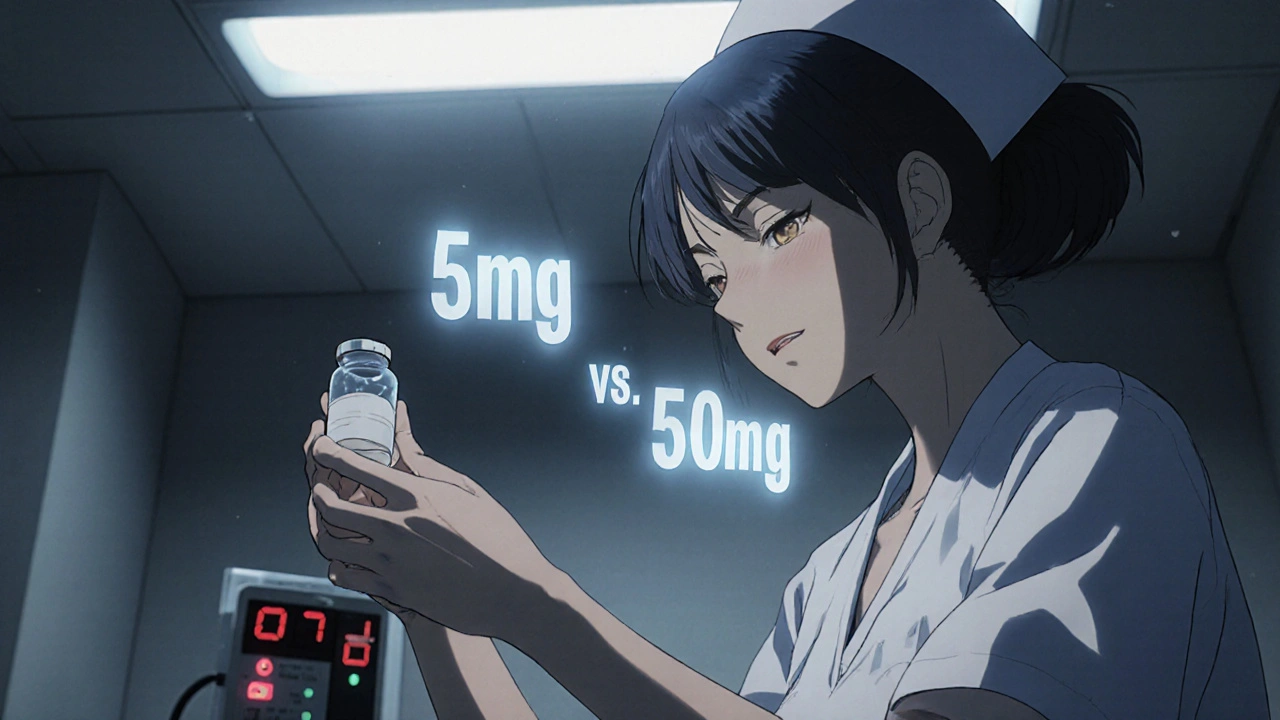
- Attention wanders-you scan a label but don’t register the difference between 5mg and 50mg.
- Reaction time slows-you miss an alarm or delay checking a patient’s chart.
- Language skills weaken-you mishear a doctor’s order or misread a handwritten note.
Studies from the American College of Obstetricians and Gynecologists show that after just one night without sleep, these skills decline by up to 30%. Speed is hit harder than accuracy-so you rush, and that’s when mistakes happen.
And it’s not just nurses. Surgeons who slept less than six hours had patients with 2.7 times more complications. Anesthesiologists who worked through the night showed a 23% drop in vigilance and 18% drop in memory during simulated procedures.
The Medications That Make Fatigue Worse
Some of the drugs you take to stay awake-or to sleep-can make things worse.
Many healthcare workers rely on over-the-counter sleep aids or antihistamines for relief. But diphenhydramine (found in Benadryl or Unisom) causes drowsiness in 50-60% of users. Zolpidem (Ambien) leaves 15-20% of people groggy the next day. Benzodiazepines like diazepam cause residual sedation in 30% of users. Even some antidepressants like trazodone can make you too sleepy to work safely.
And it’s not just nighttime meds. Narcotic painkillers like oxycodone cause sedation in 25% of people. If you’re taking any of these, even as a patient, you’re at higher risk of making an error while on shift.
The CDC’s National Institute for Occupational Safety and Health (NIOSH) says: if you’re overly sleepy at work, check your meds. Switching from diphenhydramine to loratadine (Claritin) can cut drowsiness without losing effectiveness. Don’t assume it’s just "being tired." Sometimes, it’s the medicine you’re using to cope.
System Failures Make Fatigue More Dangerous
It’s easy to blame the person. But the real problem is often the system.
Many hospitals still rely on handwritten orders, unclear labels, and high patient loads. Nurses on 12-hour shifts have a 15% higher error rate. Rotating shifts disrupt circadian rhythms so badly that workers report higher rates of depression, diabetes, and heart disease.
Even when rules exist-like the ACGME’s 2003 work-hour limits-many providers still can’t catch up on sleep during the day. One night of lost sleep takes three days to fully recover from. And if you’re working back-to-back nights? You’re running on empty.
And here’s the kicker: fatigue doesn’t just affect your actions. It affects your communication. A 2018 study found a 33% drop in effective communication during fatigue. That means you might not ask clarifying questions. You might miss a warning from a colleague. You might not double-check because you’re too tired to speak up.
What Actually Works to Prevent Nighttime Errors
There’s no magic fix. But some strategies have proven results.
1. Strategic napping-not just any nap. A 20-40 minute nap before or during a night shift improves alertness by 12-15%. It’s not a cure-all, but it helps. Longer naps (90 minutes) don’t help much more, and waking from deep sleep can leave you groggy for up to 30 minutes.
2. Caffeine timing-drink coffee early in your shift, not at 4 a.m. Caffeine takes 30 minutes to kick in. If you drink it right before a critical task, you’ll be sharper when you need to be.
3. Double-check systems-alarms, barcode scanners, and mandatory second verification reduce errors by 18%. Don’t skip the second person. Even if you’re sure, let someone else confirm. That’s not distrust-it’s safety.
4. Lighting and movement-bright lights help reset your internal clock. Walk around every hour. Stretch. Get fresh air if you can. Movement boosts alertness better than another cup of coffee.
5. Schedule changes-the most effective fix? Give people more time to sleep. Limit consecutive night shifts. Avoid rotating shifts too fast. Let people recover. This isn’t luxury-it’s patient safety.

What You Can Do Right Now
You don’t need to wait for policy changes to protect yourself and your patients.
- Before your night shift, get at least 4-5 hours of sleep-even if it’s during the day.
- Don’t rely on sleeping pills to recover. They don’t restore deep sleep cycles like natural sleep.
- Keep a log: if you’ve had less than 5 hours of sleep in the past 24 hours, flag yourself for extra caution.
- Ask for help. If you’re too tired to double-check a dose, say so. Your team will understand.
- Review your own medications. Talk to your doctor about switching to non-sedating options if you’re on diphenhydramine, trazodone, or similar drugs.
- Use technology. If your hospital has electronic prescribing or barcode scanning, use it every time-even if it’s slow.
One nurse in Sydney told me: "I used to think I was fine on three hours of sleep. Then I almost gave a patient 10 times the right dose. I didn’t even see the extra zero. That’s when I started napping before shifts. I didn’t think it would matter. It saved a life."
The Bigger Picture: Fatigue Isn’t a Personal Failure
Healthcare systems treat fatigue like a personal problem: "Just push through." But fatigue is biological. It’s not weakness. It’s physics.
When you’re sleep-deprived, your brain is literally less capable. No amount of willpower fixes that. And when we blame individuals, we ignore the real problem: systems that demand more than human biology can give.
The cost? $20 billion a year in preventable harm. Thousands of avoidable injuries. Lives lost.
Change doesn’t come from guilt. It comes from design. Better schedules. Better tools. Better support. And yes-better sleep.
Until then, protect yourself. Protect your patients. And never assume you’re "fine." If you’re tired, you’re not just at risk-you’re a risk.
14 Comments
Erika Sta. Maria
November 21, 2025So let me get this straight-sleep is the enemy of healthcare? 😂 Like, if we just stopped being human, we’d be perfect? I’ve seen nurses down 5 energy drinks and still miss a code blue because they were too busy checking their TikTok notifications. Fatigue? Nah. It’s just lazy people who think caffeine is a personality trait. 🤷♀️
Debanjan Banerjee
November 23, 2025The data here is solid. The 2023 meta-analysis cited is peer-reviewed and replicated across multiple jurisdictions. The cognitive decline equivalent to 0.05% BAC is not hyperbole-it’s from the Journal of Clinical Sleep Medicine. What’s missing is the implementation framework. Hospitals need mandatory fatigue risk assessments, not just ‘naps encouraged’ posters. We need policy, not pep talks.
Darragh McNulty
November 25, 2025This hit me right in the soul 😭 I worked nights for 3 years and almost gave a patient 10x insulin because I misread the decimal. I thought I was fine. I wasn’t. Napping before shifts changed everything. Now I bring a sleep mask and earplugs. No shame. Safety > ego. 💪😴
Daisy L
November 27, 2025America’s healthcare system is a dumpster fire on wheels-and you’re telling me the solution is… naps? 🤦♀️ We’ve got nurses working 36-hour shifts because insurance companies won’t pay for adequate staffing. Stop blaming the workers. Blame the CEOs who think ‘efficiency’ means turning humans into robots with caffeine IVs. #FixTheSystem
Anne Nylander
November 27, 2025Y’all just need to nap more!! 🌞 I started napping 20 mins before my night shift and OMG-my brain came back to life!! I didn’t miss a single med check all month. Try it!! You’ll be shocked!!
Noah Fitzsimmons
November 28, 2025Oh wow, so tired nurses are the problem? Shocking. Next you’ll tell me oxygen is flammable. Look, I’ve seen your kind-overworked, underpaid, and now suddenly it’s ‘biology’? I’ve worked 18-hour days since I was 19. No one handed me a nap blanket. You want safety? Stop whining and grow a spine.
Eliza Oakes
November 28, 2025I’m calling BS on this whole ‘fatigue is biological’ thing. If you’re tired, you’re just not disciplined enough. I’ve seen nurses sleepwalk through code blues and then cry about ‘system failures.’ Wake up. It’s not the system. It’s you. And if you can’t handle it, get out. We don’t need emotional baggage in the OR.
Corra Hathaway
November 29, 2025I love this post!! 🥹 You’re so brave for saying this out loud!! I’ve been there-almost gave a patient the wrong antibiotic because I was so tired I thought ‘amoxicillin’ and ‘azithromycin’ were the same thing. 😳 Now I always say ‘I need a second pair of eyes’ and guess what? My team says THANK YOU. It’s not weakness-it’s wisdom. 💖
Shawn Sakura
November 29, 2025I appreciate the intent here. However, the suggestion to use barcode scanners is only viable in institutions with adequate funding. In rural hospitals, we’re still using paper med sheets and handwritten orders. Technology isn’t the answer if the infrastructure doesn’t exist. We need investment-not just awareness.
Paula Jane Butterfield
December 1, 2025As someone who immigrated from the Philippines and now works in a U.S. ER, I’ve seen how different cultures handle fatigue. In my home country, we rely on community support-older nurses watch out for younger ones. Here? Everyone’s too busy to notice. Maybe the real fix isn’t naps or caffeine… it’s compassion.
Simone Wood
December 2, 2025The real issue? The ACGME’s 2003 rules are a joke. 16-hour shifts? Please. I’ve had residents pass out in the supply closet. And now you want me to believe ‘double-checking’ is the solution? We’re understaffed, overworked, and the hospital’s EHR crashes every third shift. This is performative safety. It’s not fixing anything.
Swati Jain
December 4, 2025Let’s be real-napping doesn’t fix systemic rot. You think a 20-minute snooze erases 14 hours of sleep debt? That’s like putting a Band-Aid on a hemorrhage. And don’t get me started on ‘non-sedating’ meds-loratadine doesn’t help if you’re on trazodone for PTSD and your psychiatrist won’t switch you. This is band-aid advice from people who’ve never pulled a double shift.
Florian Moser
December 5, 2025This is one of the most important posts I’ve read all year. The stats are clear. The solutions are practical. The real tragedy? We already know what works-we just don’t fund it. If we treated fatigue like a fire hazard, we’d have mandatory rest protocols. We don’t. Because we don’t value nurses as human beings. We value output.
jim cerqua
December 5, 2025I’ve been in this game 27 years. I’ve seen nurses cry in the break room because they gave the wrong dose. I’ve seen patients die because someone was too tired to read a 5mg vs 50mg label. And you know what? The system doesn’t care. They’ll replace you with a temp agency nurse who doesn’t even know the patient’s name. This isn’t about caffeine or naps. It’s about a culture that treats human life as disposable. And until we admit that-we’re all just spinning our wheels.