When you pick up a new prescription, the small booklet that comes with it isn’t just filler. It’s your first line of defense against accidental overdose. Most people glance at the dosage instructions and toss the guide aside. But if you know where to look, that same guide can tell you exactly what happens if you take too much - and what to do about it.
Start with the Boxed Warning
Every medication guide with serious overdose risks has a Boxed Warning - the strongest warning the FDA requires. It’s usually the first thing you see after the title, printed in a bold black border. This isn’t just a caution. It’s a red flag that says: take this seriously.For example, opioid painkillers like oxycodone or fentanyl patches always carry a Boxed Warning about respiratory depression. Benzodiazepines like alprazolam warn about fatal interactions with alcohol or other sedatives. If you see this box, you’re holding a drug that can stop your breathing if misused.
Find the Overdosage Section
Skip ahead to the section labeled Overdosage. It’s usually near the end of the guide, after side effects and storage instructions. This isn’t a vague warning. It’s a technical breakdown of what happens when too much is taken.Here’s what you’ll find:
- Specific symptoms tied to the drug - like drowsiness, slowed breathing, or loss of consciousness
- Dosage amounts that have caused overdose in clinical studies
- How quickly symptoms appear after ingestion
- Whether the overdose risk increases with age, liver disease, or other medications
For instance, the guide for acetaminophen (Tylenol) will tell you that taking more than 7.5 grams in a day can cause liver failure - and symptoms may not show up for 24 hours. That’s why waiting until you feel sick is too late. The guide gives you the numbers before you cross the line.
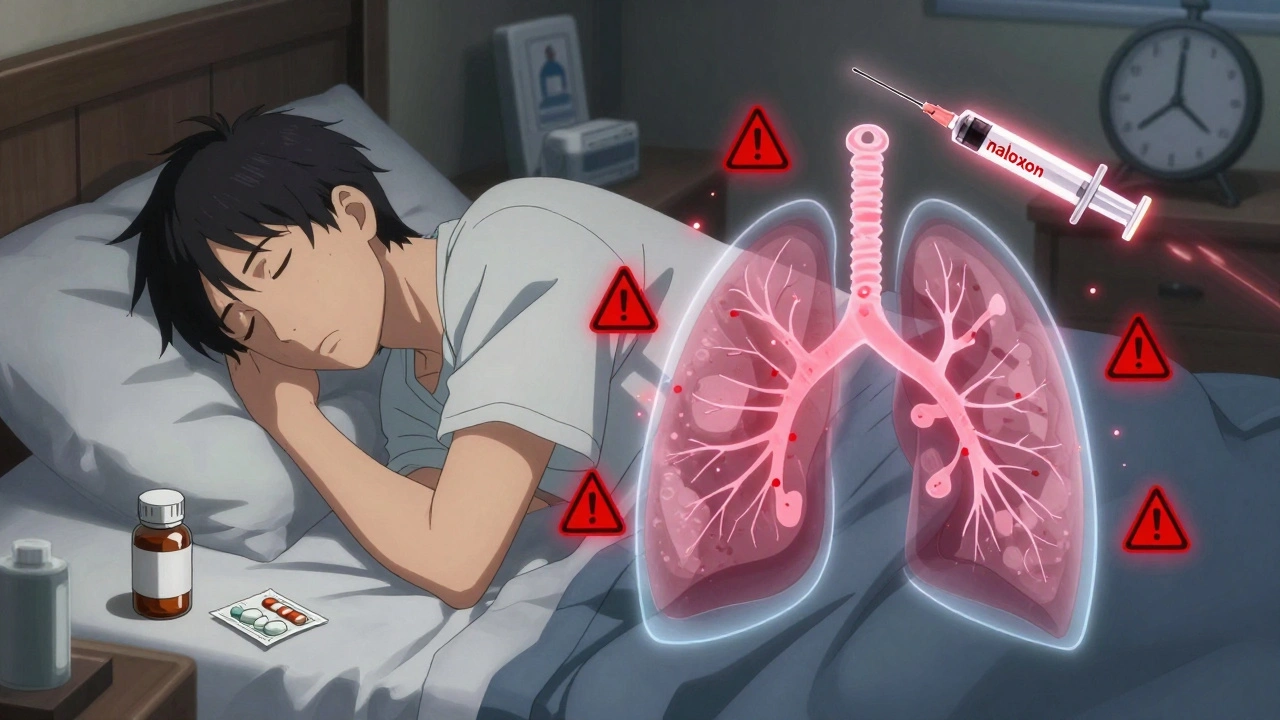
Look for Antidote Information
Right after the Overdosage section, you’ll often find a subsection called Management of Overdose or Antidotes. This is where the guide tells you what can reverse the effects.Naloxone is listed as an antidote for opioids - and it’s not just mentioned. The guide will specify:
- How much naloxone is needed (e.g., 0.4 mg to 2 mg IV or intranasal)
- Whether repeat doses are required
- That naloxone wears off faster than some long-acting opioids, meaning you still need emergency care even after it works
For acetaminophen overdose, the guide will name N-acetylcysteine (NAC) as the antidote and note that it’s most effective if given within 8 hours. It might even mention that NAC is available in hospitals - not pharmacies - so calling 911 is critical.
Understand the Contraindications
The Contraindications section tells you when you should never take the drug. But it also reveals hidden overdose risks. For example:- If you have severe liver disease, your guide for certain antidepressants will say: “Not recommended.” That’s because your body can’t clear the drug, so even a normal dose builds up to toxic levels.
- If you’re on MAO inhibitors, your guide for tramadol will warn you that combining them can cause serotonin syndrome - a deadly overdose-like reaction.
These aren’t just “don’t take if allergic” notes. They’re red flags for dangerous combinations you might not even realize are risky.
Check the Warnings and Precautions Section
This is where the guide gets detailed. Look for:- Drug Interactions - especially with alcohol, sleep aids, or other painkillers
- Special Populations - warnings for seniors, pregnant people, or those with kidney issues
- Dependence and Withdrawal - if stopping suddenly can cause seizures or rebound symptoms
Take gabapentin, for example. Its guide warns that combining it with opioids increases the risk of respiratory depression - even if you’re taking both as prescribed. That’s not obvious. But it’s in black and white in the guide.
Know What’s Missing
Medication guides don’t cover everything. They won’t tell you:- How to get naloxone without a prescription (but they might hint that it’s available over the counter)
- Where to find local harm reduction services
- What to do if you’re helping someone else who overdoses
That’s why reading the guide is only half the battle. If you’re on a high-risk medication, talk to your pharmacist. Ask: “If I take too much, what’s the exact antidote? Where can I get it?” Most pharmacists keep naloxone on hand and will give it to you free of charge.

Real-Life Example: A Prescription That Almost Killed Someone
A 68-year-old man in Sydney was prescribed oxycodone for chronic back pain. He also took melatonin for sleep. He didn’t read the guide. One night, he took an extra pill because his pain was worse. He fell asleep and didn’t wake up. His daughter found him with slow, shallow breathing.She called emergency services. Paramedics gave him naloxone - which worked. But the guide for oxycodone had clearly stated: “Concurrent use with CNS depressants (including sleep aids) may result in profound sedation, respiratory depression, coma, or death.” That line was there. He just didn’t see it.
He survived. But he didn’t need to risk it.
What to Do After Reading the Guide
Don’t just read - act:- Keep the guide with your meds - not in a drawer.
- Highlight the Boxed Warning and Overdosage section with a yellow marker.
- Write down the antidote name and where to get it (pharmacy, hospital, or community program).
- Give a copy to a family member or roommate - especially if you live alone.
- Ask your pharmacist: “Is there a naloxone kit I should have on hand?”
Medication guides are designed to protect you. But they only work if you read them. Not once. Not when you’re feeling fine. Read them when you first get the prescription - before you take the first pill.
Why This Matters More Than Ever
In 2025, overdose deaths from prescription drugs are still rising - not just from opioids, but from combinations of sedatives, painkillers, and psychiatric meds. Many of these deaths happen because people didn’t know the risks were built into their own prescriptions.You don’t need to be an expert to save your own life. You just need to know where to look.
Where do I find the overdose warning in my medication guide?
Look for the Boxed Warning first - it’s the only section with a black border. Then go to the section titled “Overdosage.” That’s where you’ll find specific symptoms, dangerous doses, and how fast effects can appear. These sections are required by the FDA for high-risk medications.
Can I get the antidote for my medication without a prescription?
For opioids, yes - naloxone is available over the counter at most pharmacies in Australia and doesn’t require a prescription. For other drugs like acetaminophen, the antidote (NAC) is only available in hospitals. Always ask your pharmacist what’s accessible and whether you should keep a kit at home.
What if I don’t understand the medical terms in the guide?
Pharmacists are trained to explain these guides in plain language. Don’t be shy - ask them to walk you through the overdose and antidote sections. You can also request a simplified version. Many pharmacies offer printed summaries for patients with low health literacy.
Are all medications required to have overdose information?
Only medications the FDA or TGA (Therapeutic Goods Administration) classify as high-risk must include a full Overdosage section. That includes opioids, benzodiazepines, insulin, anticoagulants, and some psychiatric drugs. Lower-risk meds like antibiotics or antihistamines may not have detailed overdose info - but they still list warnings in the “Warnings and Precautions” section.
Should I carry my medication guide with me?
Carrying the full guide isn’t practical, but you should carry a card with the drug name, dosage, and antidote. For example: “Oxycodone 10mg - Antidote: Naloxone. Do not combine with alcohol or sleep aids.” Keep this in your wallet or phone notes. If you’re ever found unconscious, this could save your life.



14 Comments
Louis Llaine
December 7, 2025Wow, a whole essay on reading the tiny booklet that comes with your pills. I just Google ‘what happens if I take 10 oxycodone’ and call it a day. 🤷♂️
Kyle Oksten
December 7, 2025This is exactly the kind of practical, life-saving info that gets buried under corporate fluff. The Boxed Warning isn’t a suggestion-it’s a last stand. If you’re not reading it, you’re gambling with your autonomic nervous system. And no, ‘I’ll just be careful’ isn’t a strategy. It’s a death sentence waiting for a bad night.
Sam Mathew Cheriyan
December 8, 2025lol u guys dont get it… the gov only makes these guides so they can track who’s read em. when u overdose, they check if u read the box. if u did, u get billed $20k. if u didnt? free ER. its all a money trap. also, naloxone is made by big pharma so they can sell more later. 🤫
Ernie Blevins
December 10, 2025So you're telling me the only reason people die is because they're too lazy to read? That's it? No systemic failures? No drug companies hiding risks? No doctors overprescribing? Just… bad readers? Wow. That's a nice little blame-the-victim narrative you got there.
Nancy Carlsen
December 10, 2025This is so important!! 🙌 I just gave my dad a printed copy of the guide with the overdose section highlighted and wrote ‘CALL 911 FIRST, THEN NALOXONE’ in big letters. He cried. We’re all just trying to survive this mess. 💙
Jennifer Anderson
December 12, 2025my mom took her med guide to her book club. they all started highlighting stuff and now they’re all asking pharmacists questions. it’s wild how simple this is but nobody does it. we need more of this.
Kyle Flores
December 12, 2025Reading this made me think of my cousin who passed last year. He had the guide. He even had the naloxone kit. But he was too scared to use it because he didn’t want to ‘embarrass’ himself. We need to normalize this stuff. It’s not weakness to prepare. It’s wisdom.
Ryan Sullivan
December 12, 2025While the intent of this piece is laudable, the pedagogical execution lacks epistemological rigor. The conflation of FDA-mandated labeling with individual agency constitutes a reductive fallacy, effectively absolving structural pharmaceutical malfeasance under the guise of patient responsibility. One cannot mitigate systemic risk through individual literacy alone.
Olivia Hand
December 14, 2025I’ve read this guide three times and still don’t understand why NAC is IV-only in hospitals but not available as a pill. Is there a pharmacokinetic reason, or is this just bureaucratic inertia? And why isn’t there a home version?
Desmond Khoo
December 14, 2025Y’all are overthinking it. Just keep the guide next to your meds. Highlight the scary parts. Tell someone what to do if you pass out. Boom. You just saved your life. 🎯❤️
Jane Quitain
December 16, 2025i just started reading my meds guide after my anxiety got worse and i realized i had no idea what i was taking… thank you for this. i feel less alone now. 🥺
Helen Maples
December 17, 2025There is no excuse for not reading the Overdosage section. This is not optional. This is not ‘nice to know.’ This is non-negotiable medical literacy. If you can’t read, get help. If you won’t read, don’t blame the system when you end up in the ER. You have agency. Use it.
Ashley Farmer
December 19, 2025My sister has bipolar disorder and takes lithium. I printed out the overdose section and laminated it. We keep it on the fridge. She says it makes her feel safer. That’s all we need sometimes-just a little reminder that we’re not alone.
Sadie Nastor
December 19, 2025i read this and just started crying. i’ve been taking gabapentin for years and never knew it could kill me if i mixed it with sleep meds. i’m gonna call my pharmacist tomorrow. thank you for writing this. 🤍