When someone experiences their first episode of psychosis, everything changes - in an instant. Voices that shouldn’t be there. Paranoia that feels real. Thoughts that won’t stop spinning. It’s not just a bad day. It’s not stress. It’s not laziness. It’s a medical event - and the first 12 weeks after it starts are the most important of their life.
What Exactly Is First-Episode Psychosis?
First-episode psychosis (FEP) is when a person experiences psychotic symptoms for the very first time. This might include hearing voices others can’t hear, believing things that aren’t true (like being watched or controlled), speaking in ways that don’t make sense, or acting in ways that seem strange or withdrawn. It’s not rare. About 1 in 100 people will experience psychosis by age 30. Most cases start between ages 15 and 30.
For too long, people with FEP were told to wait - to see if it passed, to get a second opinion, to try therapy first. But research now shows that waiting doesn’t help. It hurts. Every week without treatment increases the chance of long-term disability. The brain is still changing during this early stage. With the right help, recovery isn’t just possible - it’s likely.
The Critical Window: Why Timing Matters
The science is clear: treatment within the first 12 weeks of symptoms leads to dramatically better outcomes. The World Health Organization calls this the “window of opportunity.” After six months without treatment, brain changes can become harder to reverse. People lose jobs. Drop out of school. Pull away from friends. Their confidence crumbles. And once that happens, it’s harder to get back.
The RAISE study, launched by the National Institute of Mental Health in 2008, compared two groups: one that got standard care and another that received coordinated specialty care (CSC). The results were striking. Those in CSC stayed in treatment longer, improved 25% more in quality of life, had 32% better symptom control, and were 40% more likely to be back in school or working after two years. That’s not a small difference. That’s life-changing.
Even more telling: people who got treatment within six months of symptoms started showing improvement within weeks. Those who waited over a year? They struggled to catch up - even with the same treatment later on.
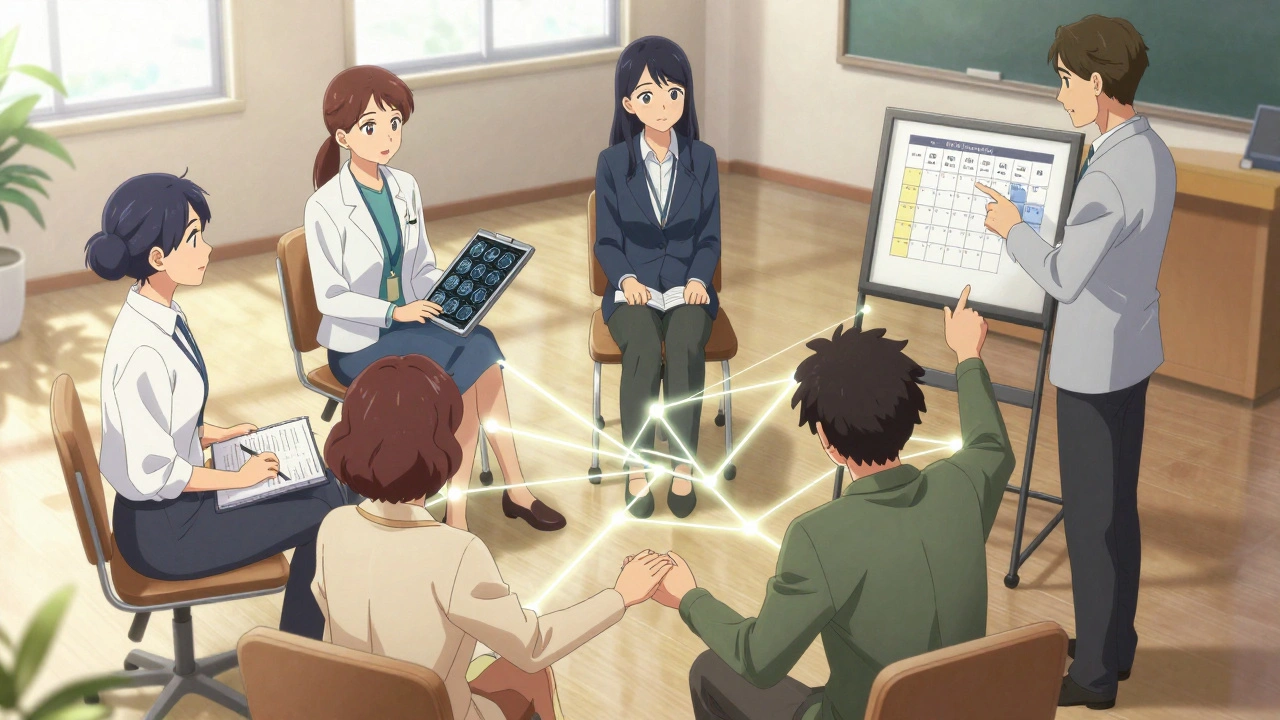
What Is Coordinated Specialty Care (CSC)?
CSC isn’t just one thing. It’s a team. A plan. A system designed specifically for first-time psychosis. It’s not a hospital stay. It’s not a single therapist. It’s five evidence-based parts working together:
- Case Management: A care coordinator helps with everything - appointments, housing, transportation, insurance. They check in 2-3 times a week during the early phase. No one gets lost in the system.
- Medication Management: Antipsychotic meds are started at the lowest effective dose. High doses? Avoided. First-generation drugs? Used only if needed. Second-generation drugs? Monitored closely for weight gain, blood sugar, and cholesterol. Metabolic checks start on day one.
- Recovery-Oriented Psychotherapy: This isn’t just talk therapy. It’s cognitive behavioral therapy (CBT) tailored for psychosis. People learn how to spot early warning signs, manage stress, and rebuild confidence. Weekly sessions for the first six months.
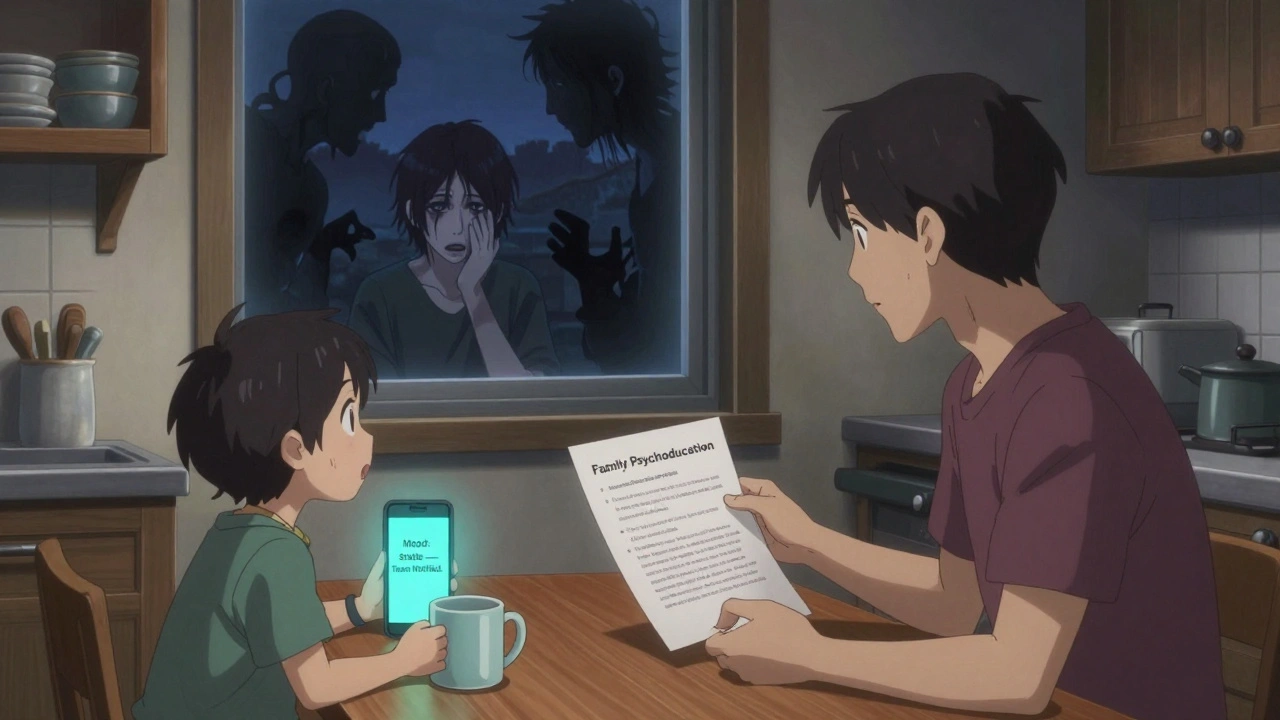
- Family Psychoeducation: Families aren’t visitors - they’re part of the team. Structured sessions teach them what psychosis is, how to respond without panic, and how to support without enabling. Studies show this cuts relapse rates by 25%.
- Supported Employment and Education: The goal isn’t just symptom control - it’s a life. The Individual Placement and Support (IPS) model helps people return to school or work. 50-60% find competitive jobs or enroll in classes. In traditional programs? Only 20-30% do.
CSC teams meet weekly. Everyone is trained in psychosis. No one is flying blind. Programs that follow this model exactly - called “high fidelity” - have success rates that standard care can’t match.
Why Family Support Isn’t Optional - It’s Essential
When someone has psychosis, families often feel helpless. They don’t know what to say. They’re scared of making things worse. Some try to reason with delusions. Others shut down. Both reactions make recovery harder.
Family psychoeducation changes that. It teaches families how to respond calmly when someone hears voices. How to ask open-ended questions instead of arguing. How to recognize early signs of relapse - like sleeping less, withdrawing, or talking in circles - before it turns into a crisis.
In the NAVIGATE trial, families who completed 8-12 sessions saw their loved ones stay in treatment longer and relapse less. But here’s the hard truth: only 55% of eligible families actually join. Barriers? Shame. Lack of time. Not knowing where to go. Some programs now offer telehealth sessions, mobile outreach, or even group workshops to make it easier.
And it’s not just about the person with psychosis. Parents, siblings, and partners are under stress too. They need support. They need to know they’re not alone.
What Doesn’t Work - And What Still Happens
Despite the evidence, too many people still get the wrong care. High-dose antipsychotics? Still used in 28% of cases - even though NICE guidelines say they offer no extra benefit and increase side effects. Isolation? Still common. People are told to “just rest” or “wait it out.”
Some clinics still treat psychosis like a chronic illness from day one - prescribing high doses, skipping therapy, ignoring education or jobs. That’s not recovery. That’s management. And it leads to long-term dependency.
Another problem: physical health gets ignored. People on antipsychotics are 4-7 times more likely to develop diabetes or heart disease. Yet only half of clinics check blood sugar or weight at baseline. That’s unacceptable. Recovery means a full life - not just fewer voices.
Barriers to Getting Help - And How Some Are Overcoming Them
CSC works. But only if you can get it. And right now, only 35% of U.S. counties have a certified program. In rural areas? It’s worse. 62% of rural counties have zero access. That means people drive hours, wait months, or give up.
Insurance is another hurdle. Only 31 states have Medicaid waivers that fully cover all CSC services. Many families pay out of pocket - or skip care entirely.
But some places are fixing this. Louisiana’s mobile crisis units now respond within 14 days. Washington State’s New Journeys program reduced the average delay in treatment from 78 weeks to just 26 weeks. Telehealth boosted family participation by 35% during the pandemic. Massachusetts trained over 300 clinicians using hands-on, competency-based programs.
And federal funding is growing. SAMHSA gave $25 million in 2023 to expand FEP programs. That’s helping about 12,000 people. But it’s not enough. Experts warn that without permanent funding, 80% of cases will still go untreated by 2027.
What’s Next? Digital Tools and New Hope
Technology is starting to help. The PRIME Care app, used in 22 CSC programs, lets people log mood, sleep, and symptoms daily. Alerts go to their care team if things start slipping. Early results show a 30% drop in hospitalizations.
Researchers are also looking for biological markers - brain scans, blood tests, voice patterns - that could catch psychosis before it fully develops. The National Institute of Mental Health is investing $50 million through 2026 to find them.
And the RAISE-2 study showed something powerful: extending CSC from two to four years kept people working and in school. Recovery isn’t a sprint. It’s a marathon - and the right support makes all the difference.
What You Can Do - Right Now
If you or someone you love is showing signs of psychosis - hearing voices, acting strangely, withdrawing - don’t wait. Don’t hope it passes. Go to the nearest mental health clinic. Ask: “Do you have a first-episode psychosis program?”
Call the National Alliance on Mental Illness (NAMI) helpline. They’ll connect you to local resources. Bring a family member. Write down symptoms. Note when they started. That information saves time.
And if you’re a teacher, coach, or friend - learn the signs. A 17-year-old who suddenly stops talking to friends? A college student who won’t sleep and thinks the professor is spying on them? These aren’t just “odd” behaviors. They’re red flags. Early action saves futures.
This isn’t about fixing someone. It’s about giving them back their life. And the best part? We already know how to do it.
What are the first signs of psychosis?
Early signs include hearing whispers or voices others don’t hear, believing things that aren’t true (like being followed or controlled), withdrawing from friends, sudden drops in school or work performance, trouble sleeping, speaking in confusing ways, or showing strong, odd emotions. These aren’t always dramatic - sometimes it’s just a person who seems “off” for weeks.
How soon should treatment start after symptoms appear?
Treatment should begin within 12 weeks of the first clear symptoms. The sooner, the better. Research shows that delays longer than six months can lead to irreversible changes in brain function and lower chances of returning to school, work, or normal social life. The window for best results is the first three to six months.
Is medication always necessary for first-episode psychosis?
Medication is usually part of treatment, but it’s not the only part. Antipsychotics are started at the lowest effective dose - often half of what’s used for chronic cases. High doses are avoided because they increase side effects without improving outcomes. Medication works best when paired with therapy, family support, and help returning to daily life.
Can family members really make a difference?
Yes. Family involvement reduces relapse by 25%. When families learn how to respond calmly, avoid arguments about delusions, and recognize early warning signs, the person with psychosis feels safer and more supported. Family psychoeducation is a proven part of coordinated specialty care - not optional.
Where can I find a coordinated specialty care program?
Check the Early Psychosis Intervention Network (EPINET) registry or call NAMI’s helpline (1-800-950-NAMI). Some states have state-run programs like New Journeys (Washington) or FEP Treatment Programs (Louisiana). If none are nearby, ask your local mental health clinic if they offer at least the core components: case management, low-dose meds, therapy, and family support.
Is first-episode psychosis the same as schizophrenia?
No. Psychosis is a symptom, not a diagnosis. First-episode psychosis can be caused by schizophrenia, bipolar disorder, severe depression, drug use, or even extreme stress. Only about 25-30% of people with FEP will later be diagnosed with schizophrenia. The goal of early intervention isn’t to label - it’s to help, no matter the cause.
Does CSC work for teenagers?
Yes. CSC is designed for ages 15-35. Teens respond even better than adults in some cases because their brains are still developing. Programs tailor therapy and school support to younger clients. Early intervention can prevent long-term disruption to education and social development.






8 Comments
Jay Everett
December 2, 2025Bro, this is the most hope I’ve felt about mental health in years 🙌 I’ve seen people vanish into the system and come out broken - but this? This is how you actually *save* someone. CSC isn’t just treatment - it’s a lifeline woven with dignity. The fact that they help people get back to school or work? That’s not clinical. That’s human. And the family stuff? My cousin heard voices for 18 months before anyone took it seriously. If we’d had this, she’d be graduating college right now, not on disability. We need this everywhere. Not just in cities. Not just for the lucky ones. For everyone.
मनोज कुमार
December 3, 2025FEP is a neurodevelopmental cascade triggered by synaptic pruning anomalies in dopaminergic pathways during late adolescence. Standard care fails because it treats symptoms not systems. CSC integrates neuroplasticity modulation via multimodal intervention. Evidence based. Period.
Laura Baur
December 4, 2025It’s so frustrating how we romanticize ‘early intervention’ while ignoring the structural violence that prevents it. Who exactly is supposed to drive 3 hours to a clinic when they’re unemployed, uninsured, and their mom works two jobs? You can’t ‘just get help’ when your county has zero resources and your insurance denies ‘experimental’ care. This article reads like a glossy brochure from a grant proposal - beautiful words, zero accountability. Where’s the funding? Where’s the policy? Where’s the outrage?
Steve Enck
December 4, 2025While the statistical outcomes cited are statistically significant, one must interrogate the epistemological foundations of the RAISE study’s operationalization of ‘recovery.’ Is returning to employment synonymous with therapeutic success? Or is this merely a neoliberal reconfiguration of mental health as productivity compliance? The medicalization of existential distress under the banner of ‘coordinated specialty care’ risks pathologizing normal developmental turbulence. Furthermore, the emphasis on pharmacological intervention - even at ‘low doses’ - presupposes a biomedical model that may be fundamentally incommensurate with phenomenological experience. We must ask: Who benefits from this framework? The patient? Or the institutional apparatus?
Joel Deang
December 5, 2025omg this is so real 😭 i had a friend go through this and they just got lost… like no one knew what to do. i tried to help but i was just a kid in college. the family didn’t even know where to start. if this was around when he was going through it… he’d be alive today. i’m crying rn. pls spread this. anyone reading this - if someone seems ‘off’ for more than a week? don’t wait. just call nami. seriously. it’s free.
Zed theMartian
December 6, 2025Oh, here we go. Another ‘miracle cure’ for psychosis wrapped in corporate jargon and Medicaid paperwork. Let me guess - next they’ll be selling CSC-branded stress balls and mindfulness apps. The truth? Psychosis isn’t a glitch to be fixed. It’s a radical rupture in perception. And if we keep trying to ‘normalize’ people back into a system that made them break in the first place… we’re not healing. We’re erasing. What if the voices aren’t symptoms? What if they’re messages? And what if the real illness is the world that can’t hear them?
Ella van Rij
December 7, 2025so… you’re telling me we spent 20 years telling people to ‘just rest’ and now we’re shocked they’re worse? 🤦♀️ congrats on reinventing the wheel with a fancy name and a PowerPoint. also, ‘low-dose meds’? that’s just calling it ‘chill meds’ now. and don’t get me started on ‘family psychoeducation’ - like, wow, teaching parents not to scream at their kid who’s hearing demons? groundbreakin'.
Roger Leiton
December 7, 2025This is so important. I work with teens in a high school and we’ve had 3 cases in the last year. One kid stopped talking, started wearing the same hoodie for 3 weeks, and scribbled ‘they’re watching through the walls’ in his notebook. We didn’t know what to do. No one in the school had training. I called NAMI on my lunch break. They connected us to a mobile CSC unit that came out within 10 days. He’s back in class now. Not ‘cured’ - but alive. And that’s everything. If you’re reading this and you’re a teacher, coach, or even just a friend - learn the signs. Don’t wait for a crisis. A whisper can become a scream. And sometimes, the only thing that saves someone is someone who noticed.