Every year, millions of people are told their liver looks abnormal on an ultrasound - but no one can tell them if it’s just fat, or if it’s starting to scar. That’s where FibroScan and serum scores come in. They’re the two main ways doctors now check for liver scarring without sticking a needle into your liver. And they’re not just alternatives to biopsy - they’re changing how liver disease is caught, tracked, and managed.
What FibroScan Actually Measures
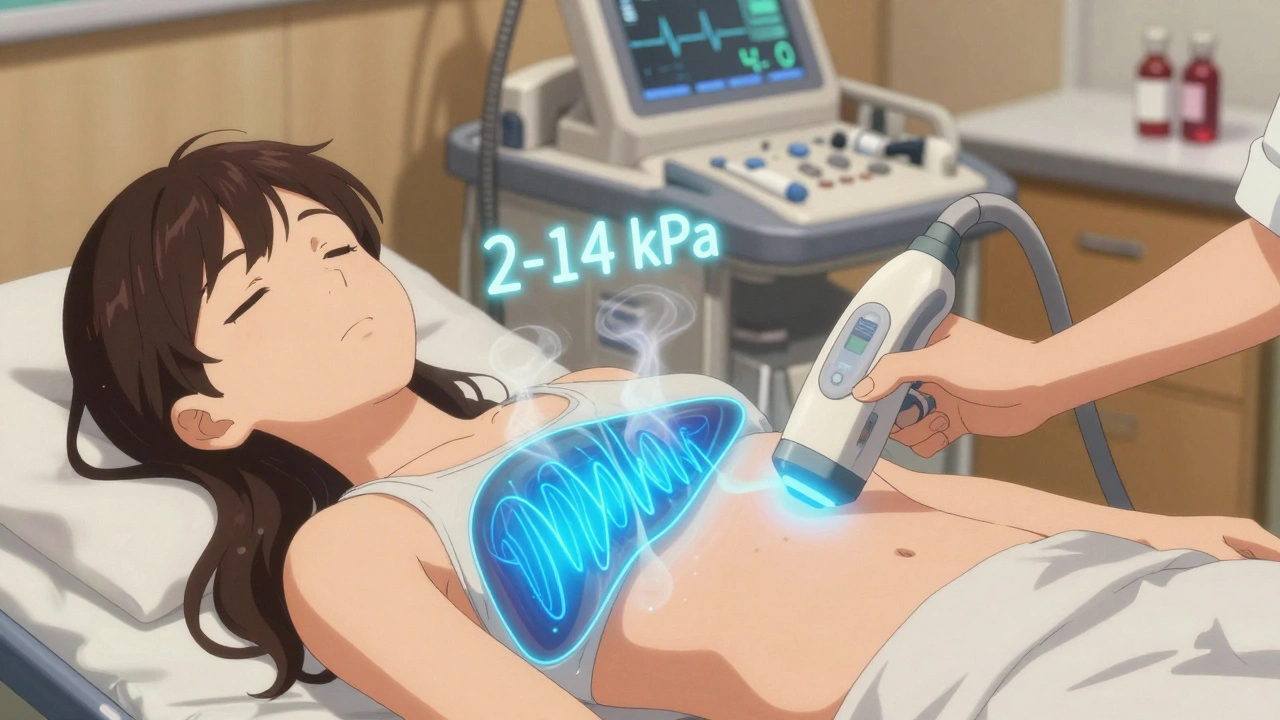
FibroScan is a handheld device that looks like an ultrasound machine but doesn’t use sound waves the same way. Instead, it sends a quick, painless pulse - like a gentle tap - through your skin and into your liver. This pulse creates a shear wave, and the machine measures how fast it moves. The stiffer the liver, the faster the wave travels. That stiffness is a sign of fibrosis - scarring.
The result? A number in kilopascals (kPa). Normal liver stiffness is between 2 and 7 kPa. Above 7, you’re moving into early scarring. Above 12, it’s advanced fibrosis. Above 14, cirrhosis is likely. But here’s the catch: those numbers mean nothing without context.
Obesity can throw off the reading. So can recent meals, alcohol the night before, or even a bad cold. A 2023 study found that in patients with BMI over 30, FibroScan failed to get a reliable reading in up to 15% of cases. That’s why newer models like the FibroScan 630 come with an XL probe - designed for larger body types. Still, even with the right probe, if your liver is swollen from inflammation, the machine might think it’s scarred when it’s not.
On top of stiffness, FibroScan also measures fat in the liver through something called CAP - Controlled Attenuation Parameter. CAP scores range from 100 to 400 dB/m. A score above 260 means you have moderate fat buildup. Above 290? You’ve got severe fatty liver. But again, CAP overestimates fat in obese patients. One study showed it flagged 81% of people with mild fat as having severe fat. That’s why doctors don’t rely on CAP alone.
Serum Scores: Blood Tests That Predict Scarring
If FibroScan is a direct scan, serum scores are like a math problem made from your blood work. You don’t need a machine - just a routine blood test. Three scores are most commonly used: FIB-4, APRI, and ELF.
FIB-4 uses four things: your age, AST (a liver enzyme), ALT (another liver enzyme), and your platelet count. Plug them into a simple formula, and you get a number. If it’s below 1.3, your chance of advanced fibrosis is less than 5%. That’s powerful. It means you can rule out serious scarring without any extra tests. If it’s above 2.67? You’re in the high-risk zone. But here’s the twist: FIB-4 is terrible at catching early scarring in people under 35. Its accuracy drops sharply in younger adults.
APRI is even simpler. Just AST and platelets. A score above 2.0 suggests cirrhosis. It’s cheap, fast, and available everywhere. But it’s not precise. Many people with normal livers get false positives. That’s why it’s mostly used to rule out cirrhosis - not to confirm it.
ELF is the most advanced serum test. It measures three proteins directly linked to liver scarring: hyaluronic acid, procollagen III, and tissue inhibitor of metalloproteinases. It’s more accurate than FIB-4 or APRI, especially in people with obesity or diabetes. But it’s not routinely ordered. It costs more, and not all labs offer it. Still, when FibroScan and FIB-4 disagree, ELF is often the tiebreaker.
Which One Is Better? The Real Answer
There’s no single winner. The best approach is using them together.
Think of it like a filter. First, use FIB-4 to screen everyone at risk - people with type 2 diabetes, obesity, high cholesterol, or heavy alcohol use. If FIB-4 is low (<1.3), you’re done. No need for FibroScan. That’s how you avoid unnecessary testing for 30-40% of patients.
If FIB-4 is borderline (1.3-2.67), then you move to FibroScan. That’s where the real diagnostic power kicks in. FibroScan gives you a clear number, not a probability. You can track it over time. If your LSM drops from 10 kPa to 7 kPa after losing weight or starting a new medication? That’s real progress.
But here’s what most people don’t realize: FibroScan misses nearly half of advanced fibrosis cases. A 2023 study found that 54% of patients with biopsy-proven stage F3 or F4 fibrosis had FibroScan results below the threshold. That’s a false negative rate of over 50%. Relying on FibroScan alone means you’re letting serious scarring slip through.
Meanwhile, FIB-4 misses advanced fibrosis in 83% of cases. So if you only use FIB-4, you’re missing most people who need help.
The truth? Neither test is perfect. But together? They’re powerful. A 2020 study showed combining FIB-4 and FibroScan reduced the need for liver biopsies by 70%. That’s huge. Biopsies are invasive, risky, and expensive. Avoiding them isn’t just convenient - it saves lives.
When to Be Wary
There are red flags that make either test unreliable.
- If your AST is more than twice the upper limit of normal - that means active liver inflammation. FibroScan will overestimate scarring.
- If you ate within the last 3 hours - food slows down liver movement and messes with the wave speed.
- If you have heart failure - fluid buildup in the liver can mimic stiffness.
- If you’re under 35 - FIB-4’s accuracy plummets. Use ELF or FibroScan instead.
- If you’re obese and your FibroScan failed twice - don’t push it. Try ELF or an MRI if available.
And don’t ignore conflicting results. One patient I read about had a FibroScan of 8.5 kPa (mild scarring) but a FIB-4 of 3.1 (high risk). The biopsy? Stage F3 - advanced fibrosis. Both tests were wrong in different ways. That’s why experts say: never trust one test alone.
What’s New in 2025
The field is moving fast. In April 2024, Echosens launched FibroScan 730 - the first model with AI-powered reliability scoring. It doesn’t just give you a number. It tells you how confident the result is. That’s a game-changer. Early data shows it cuts technical failures by 22%.
On the serum side, a new score called FIB-5 was introduced in early 2024. It adds glucose levels to FIB-4’s formula. In diabetic patients - who are at highest risk for liver scarring - FIB-5 was 89% accurate at spotting advanced fibrosis. That’s better than FIB-4 in this group.
And while MRI-based elastography (MRE) is still the gold standard for accuracy (95% for detecting stage F2 or higher), it costs 10 times more than FibroScan and isn’t widely available. For now, FibroScan and serum scores are the only practical tools for mass screening.
Real-World Impact
Primary care doctors in the UK and US are starting to automate FIB-4 into their electronic health records. One clinic in Manchester saw screening rates jump from 12% to 67% just by making FIB-4 a pop-up alert when a patient’s blood work comes in. That’s how you catch liver disease early - before symptoms appear.
Meanwhile, hospitals are using FibroScan to monitor patients on new weight-loss drugs like semaglutide. In a 2024 trial, patients on semaglutide saw their FibroScan scores drop by an average of 2.1 kPa in six months. That’s not just weight loss - that’s actual liver healing.
The goal isn’t to replace biopsy. It’s to use biopsy only when needed. Right now, too many people get biopsies because no one knows what to trust. The solution isn’t one test. It’s a smart sequence: FIB-4 first, FibroScan second, ELF if needed, biopsy last.
And that’s the future. No needles. No waiting weeks for results. Just a simple scan and a blood test - done in one visit - that tells you whether your liver is safe… or if it’s time to act.
Can FibroScan detect fatty liver?
Yes. FibroScan measures liver fat using the CAP score, which ranges from 100 to 400 dB/m. A CAP score above 260 indicates moderate fat buildup, and above 290 means severe fatty liver. But CAP can overestimate fat in obese patients, so results should be interpreted with caution and alongside other tests.
Is FIB-4 accurate for young adults?
No. FIB-4 becomes much less reliable in people under 35. Its accuracy drops from 85% to around 67% in younger adults because liver enzymes and platelet counts naturally fluctuate in this group. For younger patients with suspected liver disease, FibroScan or the ELF test are better choices.
Why do FibroScan results sometimes fail?
FibroScan can fail due to obesity, recent meals, acute liver inflammation, or technical issues. In practice, 10-15% of tests don’t produce reliable results. Using the XL probe for patients with BMI over 28 helps, but even then, some cases still fail. If results are inconsistent, doctors may recommend ELF or MRI instead.
Can serum scores replace a liver biopsy?
Not always. Serum scores like FIB-4 and APRI are excellent for ruling out advanced fibrosis, especially when results are low. But they’re not reliable enough to confirm it. FibroScan is better for staging, but even it can miss cases. Biopsy is still needed when results conflict, or when treatment decisions depend on precise fibrosis stage.
How often should I get tested for liver fibrosis?
If you have NAFLD, diabetes, obesity, or heavy alcohol use, get screened every 2-3 years if your first test is low risk. If you’re in the intermediate risk range (FIB-4 between 1.3 and 2.67), repeat FibroScan annually. If you’re high risk or have abnormal results, follow-up every 6-12 months or as advised by your doctor.
Are noninvasive tests covered by insurance?
In the UK, FibroScan is covered by the NHS for patients with chronic liver disease. In the US, Medicare and most private insurers cover FibroScan with a referral, but reimbursement is lower than for biopsies. FIB-4 is usually covered as part of routine blood work. ELF testing is less commonly covered and may require pre-authorization.
Bottom line: Liver fibrosis doesn’t cause symptoms until it’s advanced. But with the right combination of blood tests and FibroScan, you can catch it early - and stop it before it turns into cirrhosis or liver cancer. You don’t need a biopsy to know your liver’s health. You just need to know which tests to ask for.





9 Comments
Walker Alvey
December 3, 2025So let me get this straight-we’ve replaced the needle with a fancy tap and a math equation and call it progress? The liver’s not a math problem. It’s an organ that’s been screaming for decades and now we’re giving it a score. Brilliant.
Souvik Datta
December 4, 2025This is actually one of the most balanced explanations I’ve read on liver fibrosis screening. The combination of FibroScan and serum markers like FIB-4 and ELF creates a layered safety net-especially for people who can’t access biopsies. It’s not perfect, but it’s a massive leap from the old ‘wait until it’s too late’ model. Keep sharing this kind of clarity.
Jack Arscott
December 6, 2025FibroScan is a game changer 🙌 No needles, no stress, just a quick scan. My doc used it after my fatty liver diagnosis and I actually felt hopeful for the first time. CAP scores are sketchy but still useful if you know the limits. 🍎🍷
Matt Dean
December 7, 2025If you’re still relying on FIB-4 for anyone under 40, you’re doing medicine wrong. It’s like using a ruler to measure a hurricane. And CAP? That’s just a fancy way of saying ‘your BMI is high so we’re calling it severe fatty liver.’ Lazy. Use ELF. Or better yet-stop drinking and lose weight.
Dennis Jesuyon Balogun
December 7, 2025The ELF panel is the gold standard in clinical hepatology, yet its adoption remains pathologically low due to systemic underfunding of diagnostic infrastructure in low-resource settings. The cost-benefit analysis is skewed by reimbursement models, not clinical utility. We are optimizing for billing, not outcomes. This is structural failure disguised as innovation.
Grant Hurley
December 9, 2025i just got my fibroscan last week and the number was 8.2 kpa… doc said ‘eh, watch it’ and gave me a pamphlet. honestly? i didn’t even know what kpa meant till i read this. thanks for breaking it down. also… i had a burrito 2 hours before. hope that didn’t mess it up 😅
Shannon Gabrielle
December 10, 2025So let me get this straight-American medicine spends billions on fancy machines to avoid doing the one thing that actually works: telling people to stop eating garbage and drink water. We’ve turned a public health crisis into a diagnostic revenue stream. Congrats.
ANN JACOBS
December 11, 2025It is of paramount importance to recognize that while non-invasive modalities such as FibroScan and serum biomarkers represent significant advancements in the early detection of hepatic fibrosis, they are, by their very nature, surrogate markers-indirect indicators that must be interpreted within the broader clinical context. The integration of patient history, metabolic profile, and longitudinal monitoring remains indispensable to accurate diagnosis and effective intervention. We must not mistake technology for truth.
Nnaemeka Kingsley
December 12, 2025man i never knew fibroscan could measure fat too. my cousin got tested and they said he got 310 cap. he was scared but then his doc said its not always right. so now he just eating less sugar and walking daily. small steps right?