NMS Risk Assessment Tool
Neuroleptic Malignant Syndrome Risk Assessment
This tool evaluates your risk of developing neuroleptic malignant syndrome (NMS) when taking metoclopramide with antipsychotic medications. NMS is a life-threatening condition that requires immediate medical attention.
Your Risk Assessment
Based on your inputs
Combining metoclopramide with antipsychotic medications isn’t just a minor drug interaction-it’s a potentially deadly mix. If you or someone you know is taking both, you need to understand the real danger: neuroleptic malignant syndrome (NMS). This isn’t a theoretical risk. It’s a life-threatening condition that has sent patients to the ICU-and sometimes killed them. The FDA has issued a clear warning: avoid metoclopramide if you’re on antipsychotics. Yet, many doctors still prescribe them together, often because they don’t realize how dangerous this combo really is.
What Metoclopramide Does to Your Brain
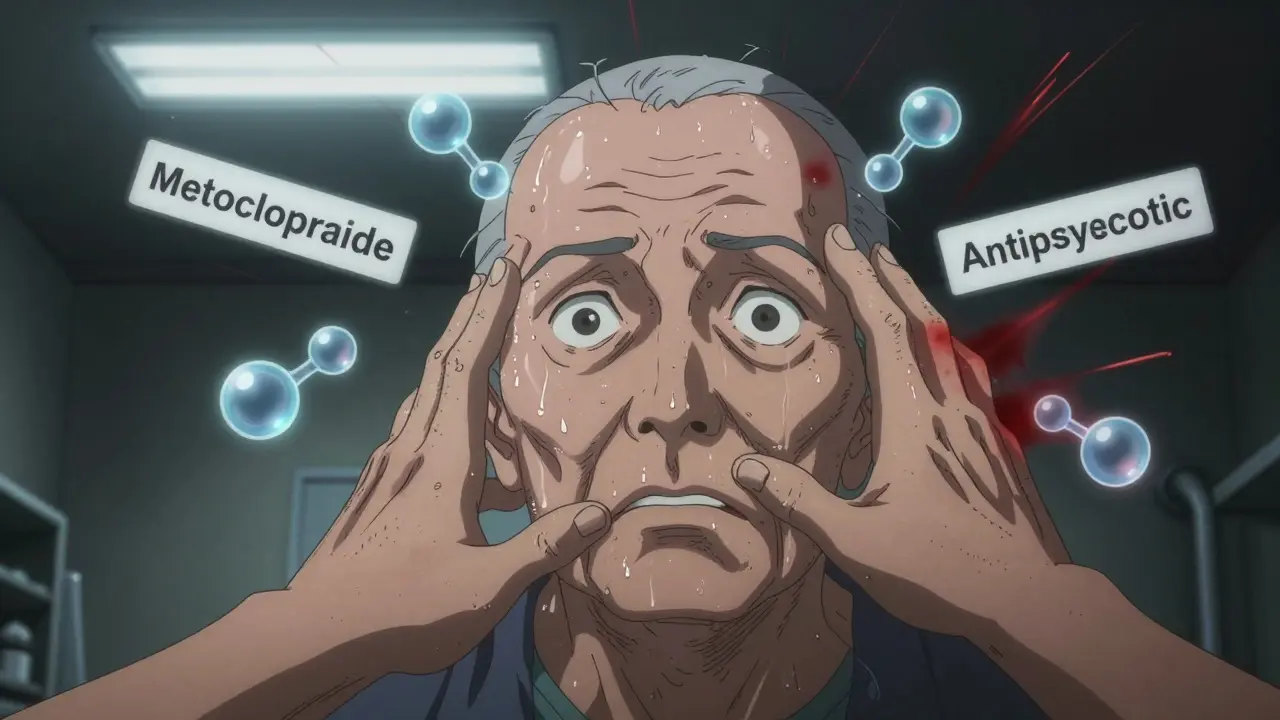
Metoclopramide, sold under brand names like Reglan and Gimoti, is commonly used for nausea, vomiting, and slow stomach emptying (gastroparesis). It works by blocking dopamine receptors in the gut to speed up digestion. But here’s the catch: dopamine isn’t just in your stomach. It’s also a key messenger in your brain, controlling movement, mood, and motivation. When metoclopramide crosses into the brain-which it does, especially in older adults or those with kidney problems-it blocks dopamine there too. That’s why it can cause tremors, stiffness, and involuntary movements. The FDA even gives it a Boxed Warning: long-term use can cause tardive dyskinesia, a permanent movement disorder.Why Antipsychotics Are the Problem
Antipsychotic drugs like haloperidol, risperidone, and olanzapine were designed to block dopamine in the brain. That’s how they reduce hallucinations and delusions in schizophrenia and bipolar disorder. But this same mechanism is what makes them dangerous when paired with metoclopramide. Both drugs are dopamine antagonists. When you take them together, they don’t just add up-they multiply. Your brain gets hit with double the dopamine blockade. This isn’t a mild side effect. It’s a pharmacological storm.Neuroleptic Malignant Syndrome: The Silent Killer
Neuroleptic malignant syndrome is the worst-case scenario of this dopamine blockade. It doesn’t happen often, but when it does, it’s fast and brutal. The classic signs are:- High fever-sometimes over 104°F (40°C)
- Severe muscle rigidity-so tight, your limbs feel like steel
- Confusion, agitation, or loss of consciousness
- Unstable blood pressure, fast heart rate, sweating
The Double Hit: Pharmacokinetics and Pharmacodynamics
It’s not just that both drugs block dopamine. Many antipsychotics also slow down how your body clears metoclopramide. Metoclopramide is broken down by an enzyme called CYP2D6. Drugs like risperidone, fluoxetine (Prozac), and paroxetine (Paxil) block this enzyme. So instead of being cleared quickly, metoclopramide builds up in your blood. Higher levels mean more dopamine blockade in the brain. This is a pharmacokinetic hit on top of the pharmacodynamic one. You’re getting more of the drug, and it’s hitting harder. That’s why people with kidney disease or genetic CYP2D6 deficiencies are at even greater risk. Their bodies can’t handle even small doses.
Who’s Most at Risk?
This isn’t a risk for everyone. But certain people are sitting on a ticking bomb:- Older adults (especially over 65)
- People with kidney problems
- Those on high-dose or long-term antipsychotics
- Patients with a history of movement disorders from any dopamine-blocking drug
- People taking SSRIs or SNRIs that inhibit CYP2D6
What Doctors Should Do-But Often Don’t
The FDA’s prescribing information for metoclopramide is crystal clear: “Avoid Reglan in patients receiving other drugs associated with NMS, including typical and atypical antipsychotics.” Yet, studies show this combo still gets prescribed. Why? Because many doctors think metoclopramide is “safe” since it’s been around since 1980. Or they assume the dose is too low to matter. It’s not. Even 5mg of metoclopramide can trigger NMS in vulnerable people. The right move? Switch to a safer antiemetic. Ondansetron (Zofran) works on serotonin, not dopamine. It won’t cause movement disorders. Promethazine (Phenergan) blocks histamine. Also safe. Prochlorperazine? That’s another dopamine blocker-avoid it too. If you need something for nausea and you’re on an antipsychotic, ondansetron is your best bet. It’s effective, widely available, and doesn’t touch dopamine.What You Should Do Right Now
If you’re taking metoclopramide and an antipsychotic:- Don’t stop either drug suddenly-this can cause withdrawal symptoms or rebound psychosis.
- Call your doctor or pharmacist immediately. Ask: “Is it safe for me to take these together?”
- Get a full list of all your medications, including over-the-counter and supplements.
- Ask if you can switch to ondansetron or another non-dopamine-blocking antiemetic.
- Watch for signs: fever, stiff muscles, confusion, fast heartbeat. If you notice any, go to the ER.
What Happens If You Ignore the Warning?
There are documented cases of people dying from NMS after being prescribed metoclopramide while on antipsychotics. One case study from 2019 involved a 72-year-old woman on risperidone who was given metoclopramide for nausea. Within 36 hours, she developed a fever of 105°F, rigid muscles, and kidney failure. She died before treatment could begin. Another case involved a 58-year-old man with bipolar disorder who developed NMS after just three days of metoclopramide. He survived, but suffered permanent brain damage. These aren’t rare outliers. They’re predictable outcomes of ignoring a clear, evidence-based warning.Alternatives That Actually Work
You don’t need metoclopramide to control nausea. Here’s what works better-and safer-if you’re on antipsychotics:- Ondansetron (Zofran): Blocks serotonin. No dopamine effect. Safe for long-term use.
- Promethazine (Phenergan): Blocks histamine. Good for motion sickness and nausea.
- Dexamethasone: A steroid sometimes used for chemo-induced nausea. Safe with antipsychotics.
- Probiotics and ginger: For mild nausea, especially in gastroparesis. No drug interactions.
Final Reality Check
Metoclopramide isn’t just risky-it’s outdated. The FDA has known since 2009 that it causes permanent movement disorders. The risk of NMS with antipsychotics has been documented in peer-reviewed journals for over 20 years. Yet, it’s still prescribed. Why? Because it’s cheap. Because some doctors never updated their knowledge. Because patients aren’t told the truth. You have the right to safe care. If your doctor says, “It’s fine,” ask them to show you the FDA label. Ask them why they’re choosing a drug with a Boxed Warning over a safer alternative. If they can’t answer, get a second opinion. Your brain and your life are worth more than convenience.Can metoclopramide cause neuroleptic malignant syndrome on its own?
Yes, though it’s rare. Metoclopramide alone has caused NMS, especially at high doses or in people with kidney problems. But the risk jumps dramatically when combined with antipsychotics. The FDA specifically warns against combining them because the interaction is so dangerous.
How long after starting both drugs can NMS occur?
NMS can develop as quickly as a few hours after the first dose, but most cases appear within 1 to 7 days. It can also happen after long-term use, especially if the dose of either drug is increased. Don’t wait for symptoms to get worse-act at the first sign.
Is it safe to take metoclopramide if I used to take antipsychotics?
No. Even if you stopped antipsychotics months ago, your brain may still be sensitive. A history of movement disorders from dopamine blockers increases your risk of NMS. The FDA advises avoiding metoclopramide entirely if you’ve ever had a reaction to antipsychotics or similar drugs.
What should I do if I’ve already taken both drugs together?
Stop metoclopramide immediately and contact your doctor. If you have symptoms like fever, stiff muscles, or confusion, go to the emergency room. Don’t wait. NMS is a medical emergency. Even if you feel fine, ask for a creatine kinase (CK) blood test-it can detect early muscle damage.
Are there any antipsychotics that are safer with metoclopramide?
No. All antipsychotics block dopamine receptors. Whether it’s haloperidol, olanzapine, quetiapine, or clozapine-they all carry the same risk when combined with metoclopramide. The interaction isn’t about the specific drug. It’s about the mechanism. Avoid the combo entirely.



13 Comments
Skye Kooyman
January 27, 2026Been on metoclopramide for gastroparesis for 3 years. Never knew it could cross the blood-brain barrier. My tremors made sense now. Thanks for the clarity.
rasna saha
January 27, 2026Thank you for posting this. My mom was on this combo and ended up in ICU last year. No one told us it was dangerous. Please share this with anyone you know on these meds.
Jessica Knuteson
January 29, 2026Another case of pharmaceutical inertia. We treat drugs like they’re immutable laws of nature instead of chemical tools with trade-offs. The FDA warning’s been there since 2009. Doctors still prescribe it like it’s aspirin. Capitalism doesn’t care if your brain melts as long as the script gets filled.
James Nicoll
January 30, 2026So we’re supposed to believe that a drug from 1980 is somehow more dangerous than the 12 new antipsychotics that came out last year with no long-term data? Classic. Also, why is everyone acting like ondansetron is a magic bullet? It’s expensive, causes headaches, and doesn’t work for half the people who try it. This post reads like a drug rep’s script.
Uche Okoro
January 30, 2026The pharmacodynamic synergy between dopaminergic antagonists is well-documented in the literature. The CYP2D6 polymorphism further exacerbates pharmacokinetic clearance deficits, resulting in supratherapeutic CNS concentrations. This is not anecdotal-it’s a class effect with a documented incidence rate of 0.02–0.05% in polypharmacy cohorts. The real issue is diagnostic delay due to non-specific symptomatology.
Ashley Porter
January 30, 2026My psych just switched me from risperidone to quetiapine last month. I was on Reglan for nausea. He didn’t mention the interaction. I’ve been having muscle stiffness since Tuesday. Should I be worried?
Peter Sharplin
January 30, 2026Yes, you should be worried. If you’re stiff, feverish, or confused, go to the ER now. If not, call your prescriber tomorrow and ask for a CK blood test. Don’t wait for symptoms to worsen. NMS isn’t something you recover from by resting. It’s a physiological cascade that can kill you in 48 hours. I’ve seen it. It’s not dramatic. It’s quiet. And then you’re gone.
John Wippler
February 1, 2026This is the kind of post that should go viral. Not because it’s scary, but because it’s true. We’ve been sold a bill of goods: cheap, old drugs are ‘safe’ because they’ve been around. Bullshit. Metoclopramide is a relic with a Boxed Warning that reads like a horror novel. And yet, it’s still the go-to for nausea because it’s $5 and the doctor’s too busy to look up alternatives. We need to stop normalizing dangerous shortcuts. Your brain isn’t a battery you can overcharge and still expect to work. This isn’t just medical advice-it’s a survival guide.
Kipper Pickens
February 2, 2026It’s worth noting that metoclopramide’s half-life extends significantly in renal impairment. In CKD stage 3+, plasma concentrations can reach 3x baseline. Combine that with CYP2D6 inhibition from SSRIs and you’ve got a perfect storm. The literature shows NMS incidence increases 17-fold in this subgroup. The FDA warning is conservative.
Aurelie L.
February 2, 2026My cousin died from this. No one warned us. The doctor said it was "just nausea."
Sally Dalton
February 3, 2026omg i had no idea!! i’ve been on zofran for months now and i feel so much better!! i just thought i was lucky, but now i realize it was because i avoided the dopamine trap!! thank you for saving me before i even knew i was in danger!!
Mohammed Rizvi
February 5, 2026Yeah sure, switch to ondansetron. At $150 a pill, good luck if you’re on Medicare. Meanwhile, metoclopramide costs $4. The real problem isn’t the drug-it’s a healthcare system that rewards profit over prevention. Your brain’s not the only thing at risk.
John Wippler
February 5, 2026And that’s why we need systemic change. Not just individual swaps. If the system made safe alternatives affordable, doctors wouldn’t have to choose between ethics and economics. But until then? Fight for your life. Ask for the label. Demand the test. Refuse the cheap pill that could kill you. Your life isn’t a cost-benefit analysis-it’s your life.