Doctor Attitudes: How Provider Mindsets Shape Your Care and Treatment Outcomes
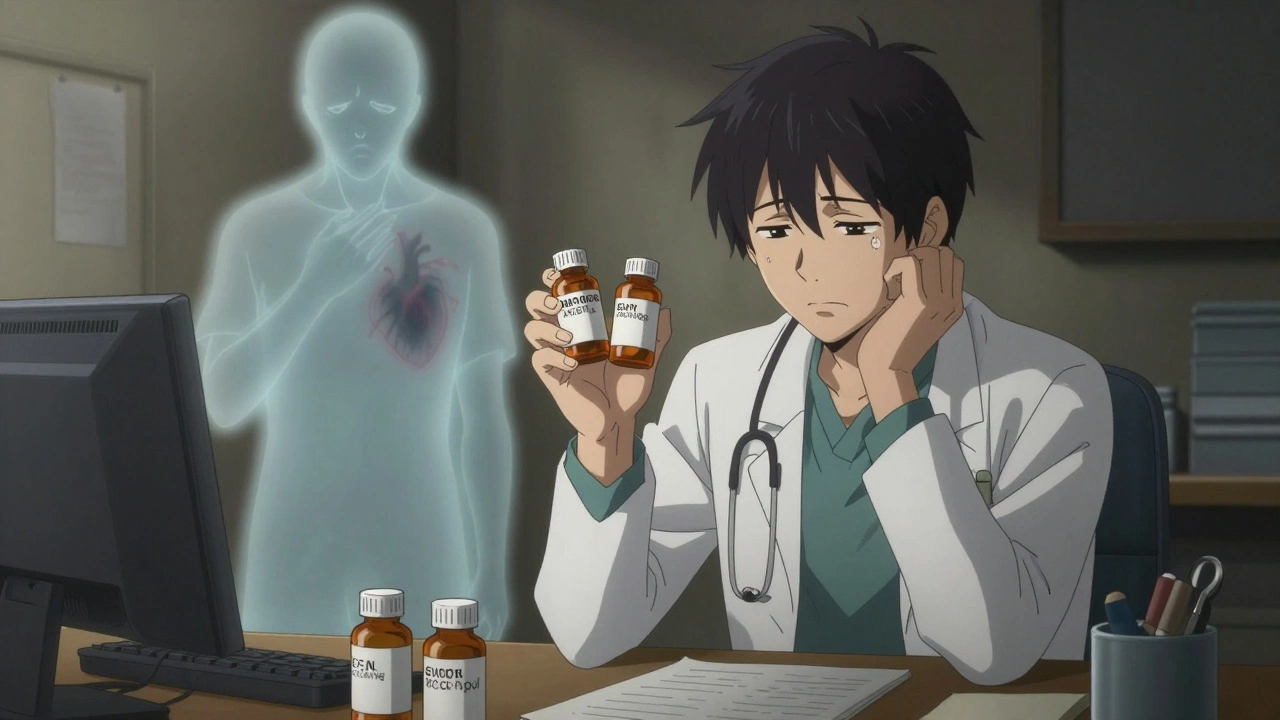
When you walk into a clinic, the doctor attitudes, the underlying beliefs, biases, and emotional responses healthcare providers bring to patient interactions. Also known as provider mindset, it shapes whether you’re heard, believed, or dismissed—even before a single test is ordered. It’s not just about what drugs are prescribed. It’s about whether your pain is taken seriously, whether your questions get real answers, or whether you’re labeled as "difficult" for asking for clarity. Studies show that when doctors assume patients won’t follow instructions, they prescribe less effectively. When they assume older adults can’t manage complex regimens, they skip key treatments. These aren’t just opinions—they’re decisions that change outcomes.
Provider bias, the unconscious preferences or stereotypes that influence clinical judgment. Also known as clinical bias, it shows up in how often certain groups get referred for specialists, how quickly pain is addressed, or whether a patient’s history is fully reviewed. A woman reporting chest pain is less likely to get a cardiac workup than a man with the same symptoms. A Black patient with high blood pressure is more likely to be told to "try harder" than given a new med. These aren’t isolated cases—they’re patterns baked into systems. And they directly connect to patient trust, the belief that your provider has your best interest at heart. Also known as therapeutic alliance, it’s the single biggest predictor of whether you’ll take your meds as directed, show up for follow-ups, or speak up when something feels wrong. If you don’t trust your doctor, you’ll stop taking the pills—even if they’re life-saving.
And it’s not all one-way. healthcare communication, how information is shared, understood, and acted on between providers and patients. Also known as patient-provider dialogue, it’s where doctor attitudes meet real-world results. A rushed visit where the doctor interrupts after 30 seconds? That’s not just bad manners—it’s a missed chance to catch early signs of kidney damage from a drug like trimethoprim, or to spot the emotional toll of plaque psoriasis on someone’s job. When communication breaks down, errors creep in. Missed doses. Wrong dosing. Avoided treatments. The posts below show how this plays out: from insurers forcing generic swaps that doctors resist, to nurses working night shifts and making mistakes because fatigue dulls judgment. Even the way a doctor reacts to a patient asking about St. John’s Wort or SGLT2 inhibitor side effects can determine whether that patient stays safe—or ends up in the ER.
You don’t have to accept silence or condescension as part of care. The right questions, the right documentation, and the right awareness of how attitudes shape treatment can shift the balance. The articles here don’t just list drugs or conditions—they show you how provider behavior affects your real-life outcomes. Whether it’s how a doctor responds to insurance rules, how fatigue changes decision-making at night, or why family support changes psychosis recovery, it all ties back to one thing: the human connection between provider and patient. What you’ll find below isn’t just medical info—it’s a map to getting the care you deserve.
Doctor Attitudes Toward Generic Drugs: What Providers Really Think
Many doctors still doubt generic drugs despite FDA approval and cost savings. This article explores why providers hesitate, what data they need, and how education is changing prescribing habits.
Continue Reading



