When your child misses a dose of medicine, it’s easy to panic. You might think, "I should just give double the next time to make up for it," or "It’s only been an hour-maybe it’s fine to give it now." But in pediatric care, those instincts can be dangerous. Giving too much medicine, even with good intentions, can lead to serious harm. The good news? There’s a clear, safe way to handle missed doses-and it doesn’t require guessing.
Never Double the Dose
This is the most important rule, and it applies to every single pediatric medication, no matter how small the dose seems. Doubling a missed dose increases the risk of severe side effects by 278% in children under 12, according to pediatric safety experts. Why? Because kids’ bodies process medicine differently than adults. Their livers and kidneys aren’t fully developed, so they can’t clear drugs as quickly. A double dose of antibiotics, pain relievers, or even asthma inhalers can cause vomiting, drowsiness, low blood pressure, or worse.Use the Time-Based Rule
The best way to decide what to do after a missed dose is to look at the time. Most pediatric medications follow a simple clock-based system:- Once-daily meds: If you miss it by less than 12 hours, give it. If it’s been more than 12 hours, skip it and wait until the next scheduled time.
- Twice-daily meds (every 12 hours): If you’re within 6 hours of the missed time, give it. After that, skip it.
- Three times a day (every 8 hours): If it’s been less than 3 hours since the missed dose, give it. Otherwise, skip it.
- Four times a day (every 6 hours): If you’re within 2 hours, give it. If it’s been longer, skip it.
- Every 2-4 hours (like some pain or fever meds): If you miss by more than 2 hours, skip it. Don’t try to catch up.
Special Cases: High-Risk Medications
Some medications are more dangerous if missed or doubled. These are called high-alert or red-category drugs. They include:- Chemotherapy drugs
- Seizure medications (like phenytoin or levetiracetam)
- Heart medications (like digoxin)
- Insulin and other diabetes drugs
- Strong painkillers (morphine, fentanyl)

Why So Many Parents Get It Wrong
A 2022 survey from the Children’s Hospital of Philadelphia found that 41% of parents couldn’t correctly tell when to give or skip a missed dose for a twice-daily medication. That number jumped to 68% for three-times-daily regimens. Why? Because instructions are often unclear. Many medicine labels just say, “Take as soon as you remember,” without saying what to do if it’s almost time for the next dose. Worse, 25% of high-risk medications don’t even include missed-dose instructions in their patient leaflets. Parents are left guessing. And when they’re tired, stressed, or juggling multiple kids and meds, they make mistakes. One parent on a parenting forum said, “The oncology team said 12 hours for chemo, but the antibiotic instructions just said ‘take as soon as remembered.’ I didn’t know which rule applied.”How to Avoid Missed Doses in the First Place
Prevention is always better than correction. Here’s how to cut down on missed doses:- Use a pill organizer with alarms. Simple, low-cost pill boxes with separate compartments for morning, afternoon, and night help. Add a phone alarm for each dose.
- Try the Pediatric Medication Safety Calculator app. Launched by the American Academy of Pediatrics in 2023, this free app asks for the medicine name, frequency, and time missed, then tells you exactly what to do. Beta users saw an 83% improvement in correct decisions.
- Use oral syringes, not spoons. The FDA says household spoons vary too much in size. A teaspoon might hold 3 mL or 7 mL-big difference when you’re giving 5 mL of liquid medicine. Oral syringes are precise and come free with most pediatric prescriptions.
- Color-code schedules. Families managing four or more meds benefit from color-coded charts. Boston Children’s Hospital found this cut missed doses by 44%.
- Teach-back method. Ask your nurse or doctor: “Can you show me how you’d give this medicine?” Then have you do it back. This simple trick reduces errors by 37%.
What to Do If You’ve Already Given a Double Dose
If you accidentally gave two doses by mistake, don’t wait. Call your pediatrician or poison control immediately. In Australia, call 13 11 26 (Poison Information Centre). Have the medicine bottle handy-note the name, strength, how much was given, and when. Do not induce vomiting unless told to. Most overdoses in children are treatable if caught early.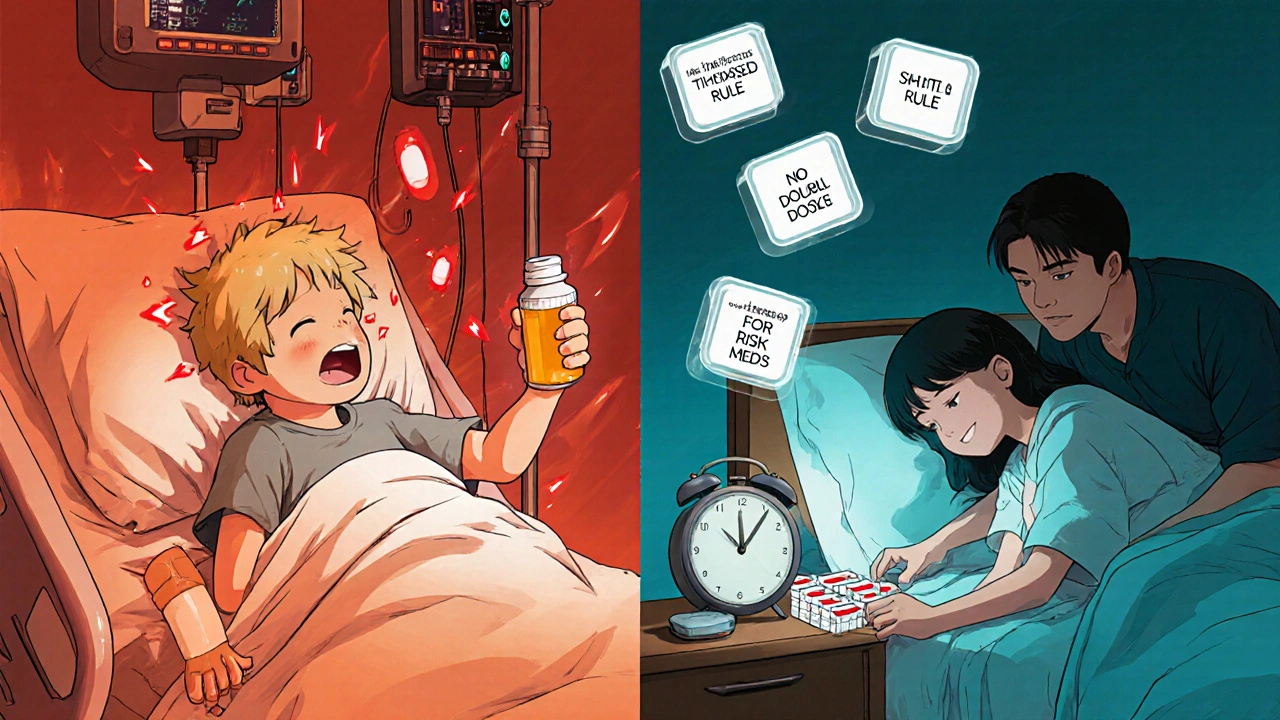
When to Seek Emergency Help
Call an ambulance or go to the ER if your child shows any of these signs after a possible overdose:- Unusual sleepiness or trouble waking up
- Fast or irregular heartbeat
- Vomiting that won’t stop
- Difficulty breathing
- Seizures or shaking
- Blue lips or skin
What’s Changing in Pediatric Medication Safety
The system is slowly improving. In 2022, the FDA began requiring all new pediatric medications to include clear missed-dose instructions on the label. New guidelines now require pictograms-simple pictures showing “give now” or “skip” for high-risk drugs. Smart dispensers that beep when a dose is due are being tested in hospitals and are reducing missed doses by 68%. AI tools that predict when a child is likely to miss a dose and send alerts to parents are in early trials. But for now, the safest tool is still your knowledge-and knowing when to call for help.Final Reminder: When in Doubt, Skip It
The safest choice when you’re unsure is always to skip the missed dose. It’s better to have a slightly lower level of medicine in the system than to risk overdose. Your child’s body can handle a short gap. Medications aren’t meant to be perfectly timed like clockwork-they’re meant to be safely managed. Missing one dose won’t ruin treatment. Doubling it might.What should I do if my child misses a dose of antibiotics?
If it’s been less than half the time until the next dose (e.g., under 6 hours for a twice-daily antibiotic), give it. If it’s been longer, skip it. Never double up. Missing one dose won’t stop the antibiotic from working, but doubling it could cause stomach upset, diarrhea, or worse.
Can I use a kitchen spoon to measure liquid medicine?
No. Kitchen spoons vary too much in size-one teaspoon could be 3 mL or 7 mL. Always use the oral syringe or measuring cup that came with the medicine. The FDA estimates that switching to syringes reduces dosing errors by 58%.
Is it okay to give a missed dose at bedtime if it’s close to the next one?
No. Giving a dose too close to the next one can cause the medicine to build up in your child’s system. For example, if the next dose is due in 1 hour and you gave the missed one, you’ve essentially given two doses 1 hour apart. That’s dangerous. Skip the missed one and stick to the schedule.
My child takes four different medications. How do I keep track?
Use a color-coded chart: assign each medication a color and write the times in matching colors. Apps like the AAP’s Pediatric Medication Safety Calculator can also help. Families using this method saw a 44% drop in missed doses. Ask your pharmacist to print a simple weekly schedule.
What if my child spits out or vomits the medicine right after taking it?
If your child vomits within 15-20 minutes of taking the dose, it’s usually safe to give another full dose. If it’s been longer than 20 minutes, assume the medicine was absorbed and don’t give more. If you’re unsure, call your doctor.
Are there apps that help track pediatric doses?
Yes. The American Academy of Pediatrics launched a free app called the Pediatric Medication Safety Calculator in 2023. It tells you exactly what to do if a dose is missed, based on the medicine and timing. It’s available on iOS and Android and has been shown to improve decision accuracy by 83%.
Should I wake my child up to give a missed dose at night?
Generally, no. If your child is asleep and you miss a nighttime dose, wait until their usual morning time to give the next one-unless it’s a high-risk medication like insulin or seizure medicine. In those cases, call your doctor. Sleep is important for recovery, and waking them up unnecessarily can cause stress and disrupt healing.
What if I’m traveling and miss a dose?
Follow the same time-based rules, but adjust for time zones. If you’re crossing time zones, keep your child on their home time zone schedule unless your doctor says otherwise. Pack extra doses in your carry-on, and always keep the medicine label with you. If you’re unsure, call your pediatrician or local pharmacy.






14 Comments
Skye Hamilton
November 29, 2025i just gave my 4yo amoxicillin at 11pm when it was supposed to be 8pm... and then i read this and panicked. like... am i a terrible mom now? the label just said 'take as soon as u remember' nothin bout windows or whatever. why is everything so complicated??
Maria Romina Aguilar
November 29, 2025I’ve noticed that the phrase 'never double the dose' is repeated, almost like a mantra... but I wonder: is this universally true? What about liquid medications with very low concentrations? The data seems to conflate all drugs into one category, which feels... reductive.
Brandon Trevino
November 30, 2025The 278% increase statistic is misleading. It’s not a controlled longitudinal study-it’s an extrapolation from ER admissions correlated with dosing errors. Correlation ≠ causation. Also, 'pediatric safety experts' is a vague credential. Name the study. Cite the journal. Otherwise this reads like fearmongering dressed as medical advice.
Denise Wiley
November 30, 2025I just want to say THANK YOU for writing this. I’ve been so scared every time my daughter misses a dose of her seizure med. I’ve cried over this. I’ve Googled until 3 a.m. And now? I feel like I actually know what to do. This isn’t just info-it’s peace of mind. You saved me tonight.
Hannah Magera
November 30, 2025I’m a new mom and this was super helpful. I didn’t know about the pill organizer trick or the color-coding. I’m gonna try the AAP app too-it sounds easy. Also, the part about not waking kids up at night made me feel better. I’ve been doing that and feeling guilty. Turns out it’s okay to let them sleep.
Austin Simko
December 1, 2025The FDA doesn’t care about your kid. They’re funded by pharma. The real reason they don’t put clear instructions on labels is because they want you to keep coming back for refills. This is all a profit scheme.
Nicola Mari
December 3, 2025It’s appalling that parents are allowed to make decisions about life-saving medication without formal training. If your child needs antibiotics, you should be required to pass a certification exam before the prescription is filled. This isn’t parenting-it’s reckless trial and error.
Sam txf
December 4, 2025You say 'skip the dose' like it's no big deal. But what if it's chemo? What if it's insulin? You think skipping one dose is harmless? That’s not how medicine works. You’re talking like it’s a missed yoga class. People die from this. And you’re just... shrugging?
George Hook
December 6, 2025I appreciate the thoroughness of this guide, but I think it’s missing a crucial layer: the emotional burden on caregivers. The fear of making a mistake, the guilt after a missed dose, the sleepless nights spent checking the clock-these aren’t just logistical problems. They’re psychological ones. We need more support systems, not just algorithms and apps. The system is failing families emotionally, not just medically.
jaya sreeraagam
December 7, 2025As a nurse in Mumbai, I’ve seen so many parents give half a tablet because they think 'less is safer' or double it because they think 'more will cure faster'. This article is gold. I’ve printed it and given copies to every family I see. Also, the color-coded chart? Genius. We use it here with stickers and crayons-kids love it. My little patient Raju now helps me pick the red pill for his asthma. It’s cute and it works.
Katrina Sofiya
December 9, 2025Thank you for sharing this with such clarity and compassion. I work in pediatric oncology, and I can tell you-this is exactly the kind of guidance families need. The fact that you included the poison control number and ER signs? That could save a life. Please keep writing. We need more voices like yours.
kaushik dutta
December 11, 2025The time-based thresholds are statistically valid but culturally inadequate. In many households, especially in collectivist societies, medication schedules are managed by extended family members who don’t speak English. The app assumes literacy, access to smartphones, and stable Wi-Fi. In rural India, a parent might have to walk 5km to refill a prescription. Algorithms don’t account for structural inequality. We need low-tech, multilingual, voice-based solutions-not another iOS app.
doug schlenker
December 13, 2025I’ve been reading all these comments and I just want to say-I get it. We’re all trying. We’re tired. We’re scared. We’re doing our best with limited info. I’m not a doctor, but I’ve given my son meds while half-asleep at 3 a.m. and I’ve panicked every time. This guide doesn’t make me feel stupid. It makes me feel seen. Thank you.
Olivia Gracelynn Starsmith
December 13, 2025The key takeaway is skip if unsure. That’s it. No need to overthink. Your child won’t die from one missed dose. They will die from a double one. Stick to the clock. Use the syringe. Call if it’s chemo or insulin. Everything else is noise.