What Happens in Your Body During an IgE Food Allergy?
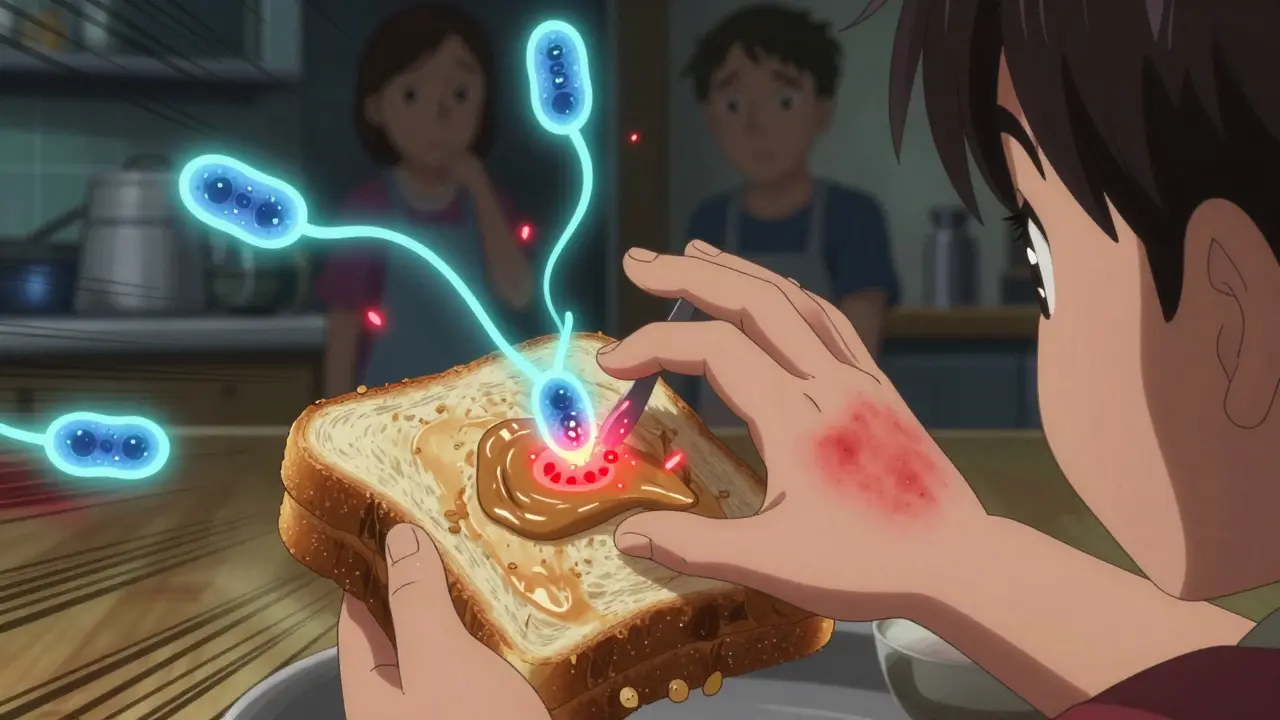
When someone has an IgE-mediated food allergy, their immune system gets confused. It sees a harmless food protein-like peanut, egg, or shellfish-as a threat. In response, it produces special antibodies called immunoglobulin E (IgE). These antibodies latch onto mast cells and basophils, which are like landmines scattered throughout the body, especially in the skin, lungs, and gut.
The first time you eat the food, nothing bad usually happens. But your immune system has now memorized it. The next time you eat even a tiny bit, the allergen snaps onto the IgE antibodies on those cells. That triggers them to explode, releasing histamine and other chemicals. Within minutes, you might get hives, swelling, vomiting, wheezing, or a drop in blood pressure. This is anaphylaxis-and it can kill.
Unlike delayed reactions that take hours or days (like lactose intolerance), IgE reactions are fast. They start in under two minutes for some people. That’s why you can’t wait to see if symptoms get worse. Every second counts.
What Foods Trigger the Most Reactions?
The top triggers change as you grow up. In babies and toddlers, milk and egg are the biggest culprits. About 2.5% of children under three react to milk. Egg affects nearly 2 in 100 kids. Peanuts are the third most common, hitting about 2.2% of young children.
By adulthood, the list flips. Shellfish becomes the number one trigger, affecting nearly 3% of adults. Tree nuts like almonds, walnuts, and cashews follow close behind. Surprisingly, sesame is rising fast-it’s now the ninth most common allergen in the U.S. and Australia.
Here’s the catch: some people can eat baked versions of these foods without a problem. A child who tolerates muffins with egg might outgrow the allergy faster. That’s because heat changes the protein structure, making it less likely to trigger IgE. But raw or lightly cooked versions? That’s when the danger kicks in.
How Do You Know If It’s a Real Allergy?
Many people think they’re allergic because they get a stomach ache after eating dairy. But that’s often lactose intolerance, not IgE. True IgE allergies involve multiple systems: skin (hives), breathing (wheezing), heart (low blood pressure), and gut (vomiting).
Doctors use a few tools to confirm. Skin prick tests show a raised bump if you’re allergic. A wheal bigger than 3mm compared to a control is a red flag. Blood tests measure IgE levels in kU/L. For peanut, a level above 14 kU/L means a 95% chance you’ll react if you eat it. But here’s the problem: these tests can give false positives. Someone might test positive but never react in real life.
The only sure way is a food challenge. You eat tiny, increasing amounts of the food under medical supervision. It’s risky-about 1 in 7 reactions need epinephrine-but it’s the gold standard. Many clinics now use open challenges when the history is clear, saving time and cost.
Can You Prevent Food Allergies Before They Start?
Yes-and the science has flipped old advice completely. For decades, parents were told to delay peanut, egg, and dairy until age 2 or 3. That made things worse.
The LEAP study in 2015 changed everything. Babies at high risk (with eczema or egg allergy) who ate peanut-containing foods between 4 and 11 months had an 81% lower chance of developing peanut allergy by age 5. That’s not a small drop. That’s life-changing.
Now, guidelines say:
- High-risk infants (severe eczema or egg allergy): Introduce peanut between 4-6 months, after seeing a doctor.
- Moderate-risk infants (mild eczema): Start around 6 months.
- Low-risk infants: No need to delay. Offer peanut and egg with other solids, like any other food.
Same goes for egg. The EAT study showed introducing cooked egg at 3 months cut egg allergy risk by 44% compared to waiting until 6 months.
But it’s not just about food. Damaged skin plays a huge role. Babies with eczema absorb allergens through cracks in their skin. That’s why using moisturizers like petroleum jelly daily from birth can cut food allergy risk by half, according to the BEEP trial. Keeping skin healthy is just as important as feeding the right foods.

What About Vitamin D, Probiotics, and Other Myths?
There’s a lot of noise out there. Some say probiotics prevent allergies. The Cochrane Review looked at 20+ studies and found no clear benefit. Don’t waste money on supplements claiming to prevent food allergies.
Vitamin D is different. Studies show babies with levels above 30 ng/mL have more regulatory T cells-cells that teach the immune system to calm down. Moms with vitamin D levels above 75 nmol/L during pregnancy had 30% lower odds of their babies becoming sensitized. That doesn’t mean take 10,000 IU a day. It means get your levels checked and stay within the normal range (50-125 nmol/L).
And yes, the “farm effect” is real. Kids raised on farms with animals and dirt have fewer allergies. Scientists are testing bacterial lysates-dead bacteria given as drops or sprays-to mimic that protective effect. Early results look promising, but it’s still experimental.
What If You Already Have a Food Allergy?
Avoidance is the rule. But avoidance isn’t always enough. Studies show 50-80% of kids with peanut allergy have at least one accidental exposure over five years. Cross-contamination in kitchens, shared utensils, or even airborne peanut dust can trigger a reaction.
So you need a plan. Epinephrine is the only thing that stops anaphylaxis. Auto-injectors like EpiPen or Auvi-Q deliver a dose in seconds. But here’s the shocking part: only half of people carry theirs all the time. And 40% of those who do use it wrong during a real reaction.
Practice with a trainer pen. Teach your kids, teachers, and coworkers how to use it. Make sure everyone knows the signs: swelling, trouble breathing, dizziness, vomiting. Don’t wait for a rash. Don’t give antihistamines first. Give epinephrine first. Then call emergency services.
Can You Outgrow a Food Allergy?
Some yes, some no. About 80% of kids outgrow milk and egg allergies by age 16. But only 20% outgrow peanut, and just 10% outgrow tree nuts. The odds improve if you can eat baked versions of the food. If your child tolerates muffins with egg, their chance of outgrowing it jumps to 75% within three years.
Component testing helps predict this. If your child’s IgE binds to Gal d 1 (a heat-sensitive egg protein), they’re more likely to outgrow it. If it binds to Gal d 2 (heat-stable), the allergy is more likely to stick.

New Treatments: Can You Build Tolerance?
Oral immunotherapy (OIT) is now FDA-approved for peanut allergy in kids 4-17. Palforzia is a powdered peanut product taken daily. After months of treatment, 67% of kids could handle the equivalent of two peanuts without a reaction. That’s not a cure-but it’s a shield. It reduces the risk of a deadly reaction from a crumb.
Sublingual immunotherapy (SLIT) works too, but slower. You hold a drop of allergen under your tongue. After a year or two, you might tolerate 3-4 peanuts. It’s less effective than OIT but safer.
Then there’s omalizumab (Xolair), an anti-IgE shot. It’s used with OIT to reduce side effects during dose increases. Studies show it cuts reaction rates in half and lets people reach their target dose faster.
Future treatments? Peptide vaccines, nanoparticle delivery, and drugs like dupilumab that block key immune signals. These aren’t ready yet, but they’re coming.
How to Prevent Anaphylaxis in Daily Life
Here’s what works:
- Always carry two epinephrine auto-injectors. One can fail. Two are non-negotiable.
- Teach your child to say “I have a food allergy” and to never accept food from others.
- Check food labels every time. Ingredients change. “May contain” warnings are not legally required but should be taken seriously.
- Use apps like “Fig” or “AllergyEats” to scan restaurant menus for allergens.
- Make sure schools have a written emergency plan. In Australia, schools with food allergy policies see 32% fewer ER visits.
- Wear medical alert jewelry. It saves time when you can’t speak.
And yes, the new Auvi-Q with voice instructions helps. In tests, 92% of people used it correctly when it spoke to them. Without voice guidance? Only 60% got it right.
What’s Next in Research?
Scientists are now asking: Can we prevent allergies before birth?
The PREPARE trial is testing whether moms who take 4,400 IU of vitamin D daily during pregnancy reduce their baby’s allergy risk. Right now, most prenatal vitamins have only 400 IU. We don’t know yet if more helps.
The EAT2 study is giving babies six allergens-milk, egg, peanut, sesame, fish, wheat-at 3 months to see if early multi-allergen exposure works even better than single-food introduction.
One thing’s clear: early exposure works. Skin protection helps. Epinephrine saves lives. And we’re getting better at predicting who’s at risk-and how to stop it before it starts.





11 Comments
Caleb Sutton
February 5, 2026This is all just a pharmaceutical scam to sell epinephrine pens. The real cause is glyphosate in our food supply. They don't want you to know.
Jamillah Rodriguez
February 5, 2026I read this and immediately thought about my cousin who broke out in hives after eating a cookie. Then she blamed the flour. Honestly, I think she just doesn't like baking.
Susheel Sharma
February 6, 2026The statistical underpinnings of the LEAP study are commendable, yet the extrapolation to general populations remains methodologically dubious. One must interrogate the confounding variables-socioeconomic stratification, microbiome diversity, and environmental epigenetics-before endorsing universal dietary mandates.
Janice Williams
February 6, 2026You're telling parents to feed peanut butter to infants? That's irresponsible. My child didn't eat anything until they were two, and they're perfectly healthy. You're just encouraging chaos.
Rachel Kipps
February 7, 2026i think this is really important info. i had no idea skin care could help prevent allergies. i'll start using more lotion on my baby. thanks for sharing.
Prajwal Manjunath Shanthappa
February 7, 2026The notion that 'early exposure' is a panacea is, frankly, a reductive fallacy. One must consider the ontological weight of immune development-not merely the temporal sequence of allergen introduction. The EAT study, while statistically significant, lacks the nuance of individual immune architecture.
Ed Mackey
February 8, 2026i carry two epi pens but i still forget to check the expiration date. maybe i'm just bad at this. but i'm trying.
Katherine Urbahn
February 10, 2026The FDA’s approval of Palforzia is a dangerous precedent. It normalizes the ingestion of a known lethal substance under the guise of 'therapy.' This is not medicine-it is corporate-enabled recklessness.
Alex LaVey
February 11, 2026I’m so glad this is getting more attention. My daughter has a severe nut allergy, and it’s been a journey. The key is community-teachers, friends, family all learning how to help. You’re not alone out there.
Jhoantan Moreira
February 13, 2026I love how science is finally catching up to what farmers have known for generations 😊 The farm effect is real-my kids grew up with goats and dirt, and they’ve never had an allergy. Maybe we’ve just been too clean for our own good.
Joseph Cooksey
February 15, 2026Let us not forget, in our enthusiasm for early allergen introduction, that the immune system is not a simple switch-it is a symphony of regulatory T cells, dendritic cell maturation, gut barrier integrity, and cytokine signaling cascades. To reduce this to 'feed peanuts at 4 months' is not only reductionist, it is dangerously simplistic; the complexity of immune tolerance cannot be distilled into a bullet point on a pediatric pamphlet. One must consider the epigenetic landscape, the maternal microbiome, the neonatal gut virome, the ambient particulate exposure, the vitamin D receptor polymorphisms-each variable a thread in the tapestry of allergic predisposition. To ignore this is to play God with a child's life using a flashlight in a hurricane.