Ever wondered why a gut‑related condition like celiac disease sometimes shows up as a burning feeling in the throat? You’re not alone-many patients report unexplained heartburn while their doctor is busy investigating gluten‑related damage. This article unpacks the science behind the overlap, shows how doctors spot the connection, and offers practical steps you can take.
What Exactly Is erosive esophagitis?
Erosive Esophagitis is a form of esophageal inflammation where the lining of the esophagus develops visible breaks or ulcers. The damage usually stems from repeated exposure to stomach acid, bile, or other irritants. When the acid eats away at the mucosal cells, the result is red, raw patches that can bleed, cause pain, and lead to narrowing over time.
Typical triggers include gastroesophageal reflux disease (GERD), certain medications, and lifestyle habits like smoking or heavy alcohol use. Symptoms range from a classic sour taste and chest‑level pain to difficulty swallowing (dysphagia) and chronic cough.
What Is Celiac Disease?
Celiac Disease is an autoimmune disorder where ingestion of gluten-a protein found in wheat, barley, and rye-provokes an immune attack on the small‑intestine lining. The attack damages villi, the tiny finger‑like projections that absorb nutrients, leading to malabsorption, anemia, and a host of extra‑intestinal symptoms.
Key genetic markers (HLA‑DQ2 or HLA‑DQ8) are present in almost everyone with celiac disease, but the condition only manifests when gluten exposure triggers the immune response.
Shared Pathophysiology: How the Two Conditions Interact
At first glance, an esophageal ulcer and a small‑intestine autoimmune reaction seem unrelated. Yet research from the past few years highlights several overlapping mechanisms:
- Increased intra‑abdominal pressure: Celiac‑related malabsorption can lead to bloating and gas, pushing the stomach upward and worsening reflux.
- Altered gut‑brain signaling: Chronic inflammation in the gut can sensitize vagal pathways, heightening the perception of heartburn even with normal acid levels.
- Immune cross‑reactivity: Some studies suggest that antibodies targeting gluten (anti‑tTG) may also bind to esophageal tissue, modestly increasing inflammation.
While the direct cause‑and‑effect link is still under investigation, the clinical overlap is real enough that physicians often screen for celiac disease when patients present with refractory erosive esophagitis.
Symptoms That Overlap
Both conditions can produce a confusing mix of gastrointestinal signs. Here’s a quick look at the common ground:
| Symptom | Erosive Esophagitis | Celiac Disease |
|---|---|---|
| Heartburn / Burning Chest Pain | ✓ | ✓ (often due to reflux from bloating) |
| Regurgitation | ✓ | ✗ (but can occur with vomiting) |
| Chronic Cough or Throat Clearance | ✓ | ✓ (irritation from acid reflux) |
| Unexplained Weight Loss | ✗ (unless severe) | ✓ (malabsorption) |
| Iron‑Deficiency Anemia | ✗ | ✓ (loss of iron absorption) |
When you see heartburn paired with anemia, chronic fatigue, or nutrient deficiencies, it’s worth asking your doctor about celiac testing.
Diagnostic Pathway: Finding the Hidden Link
Because the two diseases affect different parts of the gastrointestinal tract, a thorough work‑up uses multiple tools.
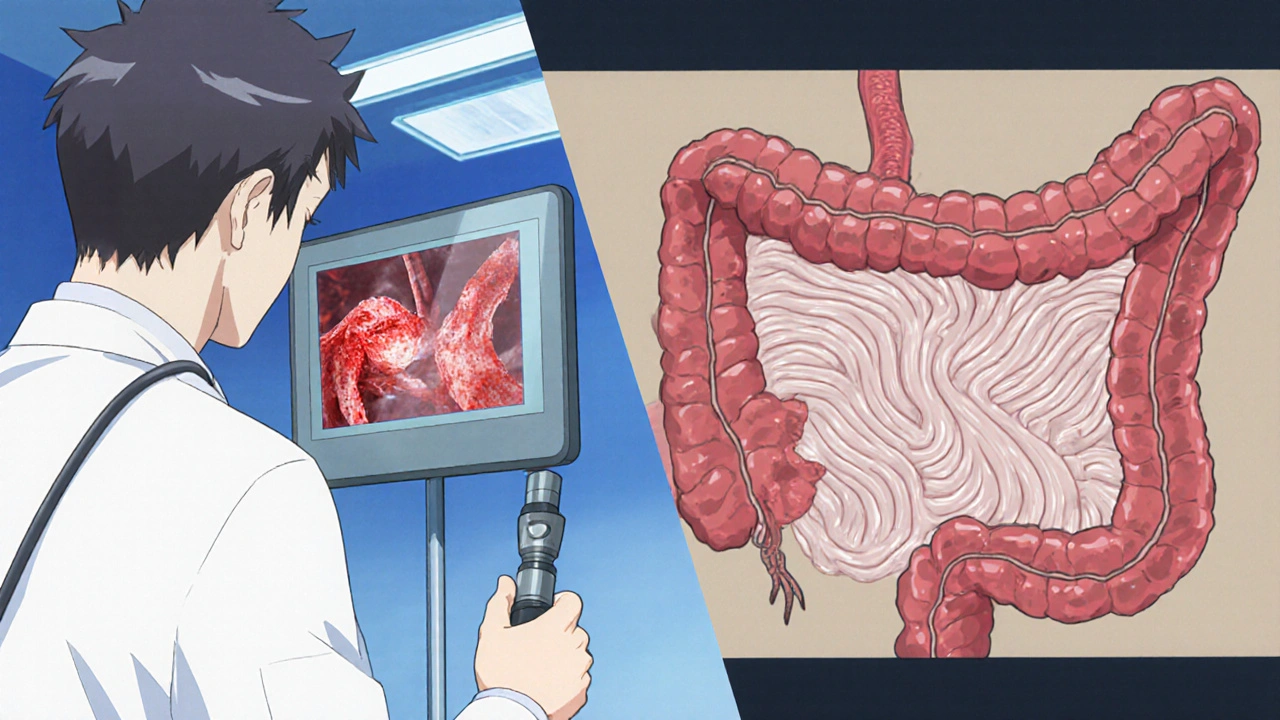
- Upper Endoscopy (EGD): Allows direct visualization of the esophagus for erosions and the duodenum for villous atrophy. Biopsies are taken from both sites.
- Endoscopy findings of erosive esophagitis often show red, friable mucosa.
- Duodenal biopsies showing flattened villi confirm celiac disease.
- Serologic Tests: Anti‑tissue transglutaminase IgA (tTG‑IgA) and endomysial antibodies are the first line for celiac screening. A normal tTG‑IgA with ongoing esophagitis may point back to reflux‑related causes.
- pH Monitoring: 24‑hour esophageal pH studies quantify acid exposure, helping differentiate pure GERD from other irritants.
- Histology: Biopsies from the esophagus are examined for basal cell hyperplasia and intra‑epithelial neutrophils-hallmarks of erosive esophagitis. Duodenal specimens are graded using the Marsh classification.
Importantly, gluten avoidance before testing can produce false‑negative serology, so doctors usually advise staying on a regular diet for at least six weeks prior to blood work.
Treatment Strategies: Addressing Both Conditions
Because the root causes differ, a combined approach often yields the best results.
- Acid Suppression: Proton Pump Inhibitors (PPIs) are the cornerstone for erosive esophagitis. Typical doses of omeprazole 20‑40 mg daily reduce acid exposure and promote healing.
- Gluten‑Free Diet (GFD): Complete elimination of wheat, barley, and rye reduces the autoimmune attack on the small intestine. Most patients notice symptom relief within weeks.
- Reading labels, avoiding cross‑contamination, and working with a dietitian are crucial for adherence.
- Lifestyle Modifications: Elevating the head of the bed, eating smaller meals, avoiding late‑night snacks, and limiting caffeine/alcohol help both reflux and bloating.
- Addressing Nutrient Deficiencies: Iron, calcium, vitamin D, and B‑vitamins often need supplementation while the gut recovers.
- Follow‑Up Endoscopy: After 8‑12 weeks of PPI therapy, a repeat endoscopy confirms healing of erosive lesions.
- If ulcers persist, consider a referral to a gastroenterologist for further evaluation (e.g., testing for eosinophilic esophagitis).
Patients who stay on a strict gluten‑free diet often see a reduction in reflux episodes simply because bloating and intra‑abdominal pressure decrease.

Red‑Flag Symptoms: When to Seek Immediate Care
Even with a solid treatment plan, some signs demand urgent attention:
- Bleeding that appears as black tarry stools or bright red blood.
- Sudden difficulty swallowing food or liquids. \n
- Severe, unrelenting chest pain that radiates to the back (possible perforation).
- Unexplained weight loss greater than 10 % of body weight.
If any of these occur, call emergency services or head to the nearest hospital.
Quick Takeaways
- Both erosive esophagitis and celiac disease can cause heartburn, but celiac adds malabsorption and systemic inflammation.
- Screen for celiac disease when esophagitis doesn’t respond to standard PPIs.
- Combine a gluten‑free diet with acid‑suppressing medication for the best symptom control.
- Endoscopy with biopsies is the definitive way to diagnose both conditions in one visit.
- Watch for red‑flag signs like bleeding or severe dysphagia and seek care immediately.
Frequently Asked Questions
Can a gluten‑free diet alone heal erosive esophagitis?
A gluten‑free diet reduces bloating and pressure on the stomach, which can lessen reflux episodes, but it rarely heals existing erosions. Most patients still need PPIs for the esophageal lining to recover.
How long does it take for the esophagus to heal after starting PPIs?
With twice‑daily dosing, visible healing usually appears within 8-12 weeks. Follow‑up endoscopy confirms that ulcers have closed.
Is it safe to take PPIs long‑term if I also have celiac disease?
Long‑term PPI use is generally considered safe for most adults, but doctors monitor for potential side effects like low magnesium or increased infection risk. Regular review of the dose is recommended.
What tests confirm celiac disease when I already have an endoscopy scheduled?
During the same upper endoscopy, doctors can take duodenal biopsies. If the villi are flattened (Marsh 3), that, combined with positive tTG‑IgA serology, confirms celiac disease.
Can I be allergic to gluten without having celiac disease?
Yes. Non‑celiac gluten sensitivity causes similar digestive upset but without the autoimmune intestinal damage or specific antibodies. Diagnosis is based on symptom improvement after gluten avoidance and exclusion of celiac disease.






8 Comments
Deja Scott
October 21, 2025I’ve dealt with relentless heartburn for years and finally learned that it wasn’t just GERD. The doctor ran a celiac panel after I mentioned anemia and the results changed everything. It turns out the bloating from gluten was pushing my stomach up, worsening the reflux. Since switching to a strict gluten‑free diet, my esophagitis healed much faster alongside the PPIs.
Natalie Morgan
October 30, 2025Interesting link between gut pressure and acid splash. Gluten avoidance can lower intra‑abdominal pressure and calm the esophagus. I’ve felt the difference after cutting out barley and rye
Mahesh Upadhyay
November 8, 2025It’s shocking how a simple grain can ignite a fire in the throat! My ulcer healed only after the gluten was gone.
Rajesh Myadam
November 17, 2025Reading this reminded me of my own journey. I was skeptical at first, but after a series of endoscopies showed both erosive lesions and flattened villi, the combined therapy made a huge difference. The most helpful part was the dietitian’s guidance on label reading, which prevented cross‑contamination and kept my iron levels stable.
Andrew Hernandez
November 27, 2025Gluten‑free plus PPI worked for me.
Ron Lanham
December 6, 2025First, let’s be clear: the coexistence of erosive esophagitis and celiac disease is not a coincidence, it is a convergence of pathophysiological pathways that demand comprehensive management. When the small intestine is inflamed by gluten, malabsorption leads to gas formation, which raises intra‑abdominal pressure and forces gastric contents upward, directly aggravating reflux. Moreover, the immune system, once primed to attack transglutaminase, can create cross‑reactive antibodies that bind to esophageal epithelium, adding a layer of inflammation that PPIs alone cannot resolve. This is why a patient who appears refractory to standard acid suppression often shows dramatic improvement once the gluten trigger is eliminated. The diagnostic work‑up should therefore be systematic: start with a thorough history, then proceed to serology, but only after confirming that the patient has been on a gluten‑containing diet for at least six weeks. Endoscopy offers a dual advantage-visual confirmation of erosions and the opportunity to biopsy the duodenum for villous atrophy, thereby confirming celiac disease in a single session. pH monitoring remains valuable to quantify acid exposure and differentiate pure GERD from reflux secondary to celiac‑related bloating. Treatment, however, must be two‑pronged. High‑dose PPIs are essential for mucosal healing, yet they should be tapered once the esophagus shows endoscopic resolution, provided the gluten‑free diet is strictly adhered to. Simultaneously, a dietitian‑guided gluten‑free regimen restores nutrient absorption, corrects anemia, and reduces abdominal distension, indirectly lowering reflux episodes. Patients often report a noticeable decline in heartburn frequency within weeks of eliminating gluten, underscoring the importance of dietary compliance. Finally, regular follow‑up-both clinical and endoscopic-is critical to monitor healing, adjust PPI dosing, and reassess for potential complications such as strictures or Barrett’s esophagus. In summary, the synergy between pharmacologic acid suppression and strict dietary exclusion addresses both the symptom and the underlying trigger, offering the best chance for sustained remission.
Sebastian Green
December 15, 2025I usually keep to myself, but this article gave me a clear checklist. I’ll ask my gastroenterologist about ordering both esophageal and duodenal biopsies next visit. Hope it helps me avoid unnecessary meds.
Wesley Humble
December 24, 2025From a clinical standpoint, the evidence supporting cross‑reactivity between anti‑tTG antibodies and esophageal tissue remains limited, warranting cautious interpretation. Nonetheless, the pragmatic recommendation to screen refractory erosive esophagitis patients for celiac disease is justified by the overlapping symptomatology and cost‑effectiveness of serologic testing. It is imperative to maintain the gluten challenge prior to serology to avoid false‑negative results, a nuance often overlooked in primary care settings. The integration of dietary therapy with proton pump inhibition reflects an evidence‑based, multimodal approach that aligns with current gastroenterological guidelines. 📚