Allergic Conjunctivitis Symptom Severity Calculator
Symptom Assessment
Rate each symptom on a scale of 1-5 (1 = mild, 5 = severe). This tool helps estimate overall symptom severity for allergic conjunctivitis.
Your Symptom Severity Assessment
When spring rolls around, many people reach for a tissue to wipe away runny noses and itchy throats. What’s less obvious is how those same triggers can inflame the eyes, leading to a surge in Allergic Conjunctivitis. This article untangles the link between seasonal allergens-especially pollen-and the rise in eye‑related allergy cases, showing you why the pattern matters for patients, clinicians, and public‑health planners.
Key Takeaways
- Seasonal pollen peaks are the strongest driver of allergic conjunctivitis spikes worldwide.
- Prevalence varies by region, age, and local vegetation, with Australia seeing a 28% rise over the past decade.
- Environmental controls cut symptom severity by up to 45% when combined with appropriate medication.
- Topical antihistamine eye drops provide rapid relief, while allergen‑specific immunotherapy offers long‑term disease modification.
- Early diagnosis and integrated nasal‑eye treatment reduce the risk of chronic eye complications.
Understanding the Core Entities
Allergic conjunctivitis is an inflammatory condition of the conjunctiva triggered by an immune response to airborne allergens. The hallmark signs are redness, itching, tearing, and a gritty sensation. It often co‑occurs with allergic rhinitis, forming the classic “allergic rhinoconjunctivitis” syndrome.
Seasonal allergy refers to hypersensitivity reactions that flare during specific times of the year, most commonly in spring and early fall when pollen counts soar.
Pollen are microscopic grains released by trees, grasses, and weeds. Their size (10‑100µm) allows them to settle on the ocular surface, where they activate mast cells.
Mast cells line the conjunctival tissue and, upon allergen exposure, release histamine, prostaglandins, and leukotrienes, leading to the classic eye symptoms.
Antihistamine eye drops block histamine receptors on the ocular surface, providing quick symptom relief within minutes.
Mast cell stabilizers prevent degranulation, reducing inflammation over several hours of regular use.
Allergen‑specific immunotherapy (AIT) gradually desensitizes the immune system by exposing patients to increasing amounts of the offending allergen.
How Seasonal Allergens Drive Conjunctivitis Prevalence
Data from the Global Allergy and Asthma Platform (2023) show that regions with high tree‑pollen counts experience a 1.7‑fold increase in allergic conjunctivitis cases during peak months. In Sydney, the average birch‑pollen season (mid‑September to early October) aligns with a 28% rise in eye‑related allergy clinic visits compared to non‑pollen months.
The mechanism is straightforward: airborne pollen settles onto the tear film, where it is recognized by IgE antibodies bound to conjunctival mast cells. This triggers a cascade of mediators-histamine, prostaglandin D2, leukotriene C4-causing vasodilation, increased vascular permeability, and nerve irritation. The result is the itchy, watery eyes that define the condition.
Importantly, the severity of conjunctival symptoms often mirrors nasal symptom scores. Studies using the Total Ocular Symptom Score (TOSS) reported a Pearson correlation of 0.73 with the Total Nasal Symptom Score (TNSS) during peak pollen days, underscoring the linked nature of the two organ systems.

Epidemiology: Who Is Most Affected?
Globally, roughly 20% of the population experiences some form of allergic conjunctivitis, but prevalence spikes to 30‑35% in high‑pollen zones. Age‑specific trends reveal:
- Children (5‑12years): 25% prevalence-often the first sign of atopic disease.
- Adolescents (13‑18years): 28%-increased outdoor activities boost exposure.
- Adults (19‑65years): 32%-cumulative sensitization and occupational exposures play a role.
- Seniors (>65years): 22%-lower exposure but higher likelihood of comorbid dry‑eye syndrome.
Urban dwellers tend to report higher symptom scores, likely due to the “urban heat island” effect that prolongs pollen season by 2‑3weeks.
Diagnosing Allergic Conjunctivitis
Diagnosis hinges on a clear history of seasonal symptom onset, bilateral eye involvement, and the presence of accompanying allergic rhinitis. Clinicians typically perform:
- Slit‑lamp examination to assess conjunctival hyperemia and papillary reaction.
- Skin‑prick testing or serum-specific IgE to identify the offending pollen type.
- Exclusion of infectious causes (e.g., bacterial conjunctivitis) through Gram stain when purulent discharge is present.
A positive skin‑prick test to grass pollen, combined with characteristic ocular findings, confirms the diagnosis in >90% of cases.
Management Strategies: From Quick Relief to Long‑Term Control
Effective treatment blends environmental control, pharmacotherapy, and, when needed, immunotherapy.
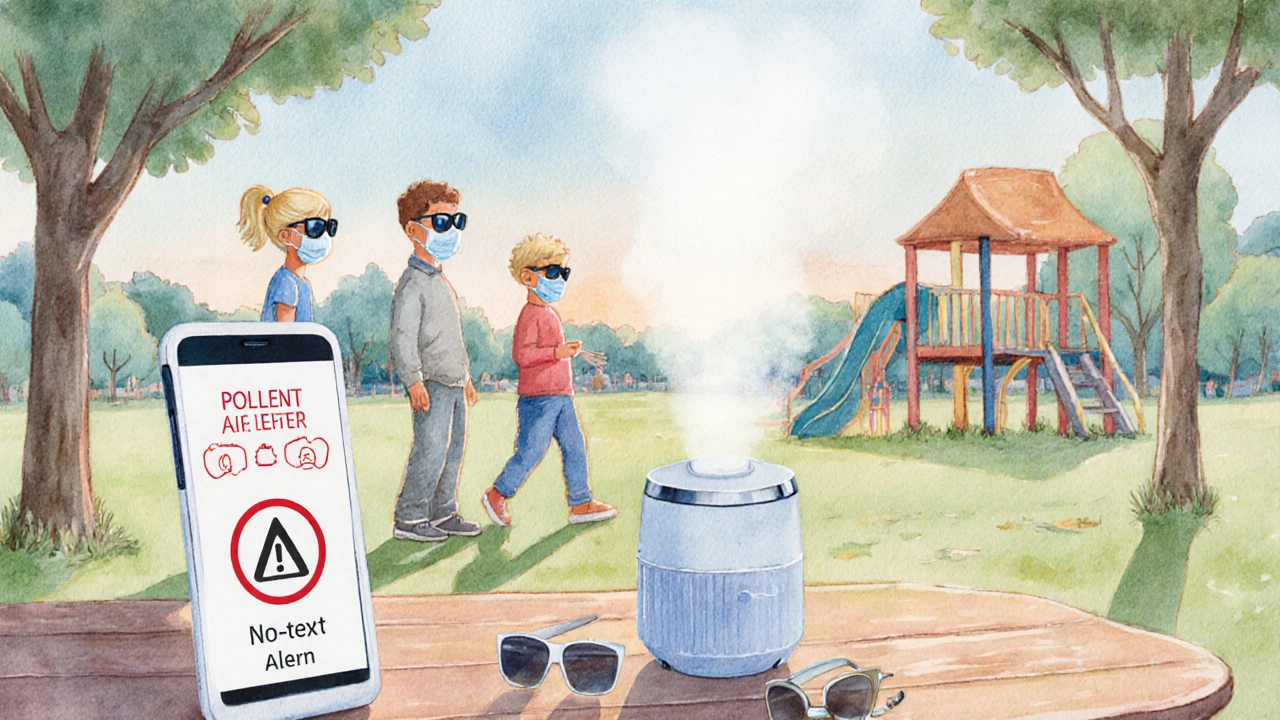
Environmental Controls
Simple steps can slash exposure by up to 45%:
- Keep windows closed on high‑pollen days; use HEPA filters.
- Wear wrap‑around sunglasses outdoors to shield the conjunctiva.
- Shower and change clothes immediately after returning home.
Pharmacologic Options
| Medication | Primary Action | Onset of Relief | Typical Duration of Use |
|---|---|---|---|
| Antihistamine eye drops | Blocks H1 receptors | 5‑10minutes | PRN (as needed) or daily during season |
| Mast cell stabilizers | Prevents degranulation | 30‑60minutes | Daily throughout pollen season |
| Combination antihistamine/mast‑cell | Dual action | 5‑15minutes | Daily during season |
| NSAID eye drops | Inhibits prostaglandin synthesis | 15‑30minutes | Short courses for flare‑ups |
| Oral antihistamines | Systemic H1 blockade | 30‑45minutes | Daily during season |
For most patients, a first‑line combination antihistamine/mast‑cell drop (e.g., olopatadine) offers rapid relief and a prophylactic effect.
Allergen‑Specific Immunotherapy (AIT)
AIT is the only disease‑modifying option. A 2022 meta‑analysis of 12 randomized trials showed a 38% reduction in conjunctival symptom scores after three years of sublingual grass‑pollen drops. The protocol involves daily low‑dose exposure, gradually increased under specialist supervision.
When to Escalate Care
If symptoms persist despite optimal topical therapy, consider:
- Adding a short course of topical corticosteroids (max 2weeks) to break severe inflammation.
- Referral to an allergist for AIT evaluation.
- Screening for co‑existing dry‑eye disease, which can exacerbate ocular irritation.
Public Health Perspective: Reducing the Seasonal Burden
From a community standpoint, tracking pollen forecasts and issuing public alerts can lower clinic visits. In Melbourne, an integrated pollen‑alert app reduced emergency eye‑clinic presentations by 12% during the 2024 season.
Schools can mitigate impact by scheduling outdoor activities for late morning when pollen counts dip slightly, and by providing anti‑pollen wipes for children with known sensitivities.
Practical Checklist for Patients and Providers
- Verify pollen type via local aerobiology reports.
- Implement daily environmental controls during peak weeks.
- Start a combination antihistamine/mast‑cell eye drop before symptoms appear.
- Re‑assess after 2weeks; adjust to oral antihistamines if ocular relief is insufficient.
- Discuss AIT eligibility if symptoms recur year after year.
Frequently Asked Questions
Can allergic conjunctivitis lead to permanent eye damage?
Chronic inflammation can cause keratoconjunctivitis sicca (dry eye) and, rarely, corneal scarring. Early treatment and proper lubrication usually prevent irreversible damage.
Why do some people only get eye symptoms and not a runny nose?
Individual IgE profiles vary. Some patients have higher ocular mast‑cell density, making the eyes the dominant site of reaction.
Is it safe to use over‑the‑counter antihistamine drops for an entire season?
Yes, most OTC drops are formulated for prolonged daily use. However, if you need steroids or experience worsening symptoms, see a clinician.
How soon before pollen season should I start preventive treatment?
Begin prophylactic eye drops 1‑2weeks before the first forecasted high‑pollen day. This allows mast‑cell stabilizers to build up protective effects.
Do diet or supplements affect allergic conjunctivitis?
Omega‑3 fatty acids and quercetin have modest anti‑inflammatory properties, but they should complement-not replace-standard medication.
Understanding the seasonal dynamics behind allergic conjunctivitis empowers patients to act before the eyes start itching. By combining smart environmental habits with the right drops-and considering immunotherapy for the stubborn cases-most people can keep their eyes clear throughout pollen‑heavy months.






19 Comments
Rashi Shetty
October 5, 2025While the article offers a thorough overview, it neglects the socioeconomic disparities that exacerbate allergic conjunctivitis in under‑privileged populations. The focus on pharmacologic solutions feels overly commercial, as if promoting a market for eye‑drops rather than addressing root causes. Moreover, the environmental control recommendations assume access to HEPA filters, which many patients simply cannot afford. 🌍💧 It would be prudent to include community‑level interventions alongside individual strategies. 😒
Queen Flipcharts
October 6, 2025One might contemplate the very notion of "seasonal" in a world where climate change renders traditional calendars obsolete. Our nation’s forefathers imagined a static climate, yet we now confront relentless pollen onslaughts that defy borders. The article wisely underscores prophylactic treatment, but fails to invoke the patriotic duty of safeguarding our citizens’ ocular health. In the spirit of national resilience, we must fund research into indigenous plant variants that provoke fewer reactions.
Yojana Geete
October 8, 2025Oh dear the drama of those itchy eyes! I swear the pollen was like an army invading my lids without any mercy yet the article just lists steps like a grocery list. Still the tone sounds like a lecture from a distant professor.
Jason Peart
October 9, 2025Hey folks, I totally get how frustrating allergic conjunctivitis can be – it’s like trying to focus on a video game while your screen is fogged. My recommendation? Start the combo antihistamine/mast‑cell drops a week before the forecast, even if you feel fine now. Also, keep a small bottle in your bag – you never know when a surprise flare will hit during a meeting. Remember, a little pre‑emptive care goes a long way, and don’t hesitate to ask your doc about oral antihistamines if the drops alone aren’t cutting it.
Hanna Sundqvist
October 10, 2025Honestly, all this “science” is a cover‑up for a global conspiracy to keep us buying overpriced meds. I read somewhere that pollen counts are faked to boost pharmaceutical profits. Maybe we should just accept the itching.
Jim Butler
October 11, 2025The systematic approach outlined in the piece is exemplary; it aligns with best practices and underscores the necessity for early intervention. Implementing HEPA filtration and wearing protective eyewear can reduce exposure by nearly half, a statistic that should motivate policy makers. Let us embrace these evidence‑based strategies for the betterment of public health. 😊
Ian McKay
October 13, 2025It’s "antihistamine" not "anti‑histamine".
Deborah Messick
October 14, 2025While the data supporting combination eye‑drops is compelling, I maintain a healthy skepticism toward industry‑driven recommendations. The article could have better addressed alternative therapies, such as acupuncture, which some patients find effective. Also, the emphasis on corticosteroids, albeit brief, should be starkly warned against due to potential intra‑ocular pressure spikes. In sum, a more balanced discourse would serve readers well.
Jolanda Julyan
October 15, 2025First, let us acknowledge that allergic conjunctivitis, though often dismissed as a minor inconvenience, can profoundly impact daily productivity and overall quality of life. Second, the article’s checklist is a solid foundation, yet it omits the crucial role of patient education in ensuring adherence to prophylactic regimens. Third, while HEPA filters are beneficial, many low‑income households cannot afford such devices, leading to an inequitable health burden. Fourth, the recommendation to wear wrap‑around sunglasses is sound, but cultural considerations often deter consistent use, especially among younger demographics.
Fifth, the timing of initiating treatment-ideally one to two weeks before peak pollen-requires accurate forecasting, which is not uniformly available across regions. Sixth, the article rightly highlights the superior efficacy of combination antihistamine/mast‑cell drops, yet it fails to discuss the cost‑effectiveness compared to monotherapy. Seventh, there is a growing body of evidence supporting oral omega‑3 supplementation as an adjunctive anti‑inflammatory measure, which could have been mentioned.
Eighth, the discussion on allergen‑specific immunotherapy (AIT) is promising, but the logistical challenges-such as patient commitment to daily sublingual dosing and the need for specialist supervision-warrant deeper exploration. Ninth, the potential side effects of short‑course topical steroids, including raised intra‑ocular pressure and cataract formation, should be emphasized with clear monitoring guidelines. Tenth, the article could have elaborated on the psychosocial impact of chronic eye itching, which often leads to irritability and reduced concentration.
Eleventh, environmental controls like showering after outdoor exposure are straightforward but rely on personal discipline, a factor that varies widely. Twelfth, schools implementing anti‑pollen wipes represent an innovative community approach, yet the feasibility and cost implications remain uncertain. Thirteenth, the mention of urban heat islands prolonging pollen season is accurate, but mitigation strategies-for example, increasing urban green spaces with low‑pollen species-are absent.
Fourteenth, the piece briefly touches on dry‑eye syndrome as a comorbidity, but does not provide guidance on lubricating eye‑drop selection or usage frequency. Fifteenth, the reference to the 2024 Melbourne app demonstrates technology’s role, yet similar platforms are lacking in many parts of the world.
Sixteenth, overall, the article provides a valuable framework, but future editions should strive for a more holistic perspective that integrates socioeconomic, cultural, and technological dimensions to truly empower patients across diverse settings.
Kevin Huston
October 16, 2025Yo, the pollen blitz is like a rogue army marching through our nostrils and eyes, and the pharma giants are just cashing in on our misery. This article does a decent job listing drops, but it forgets to shout about the eco‑war we’re fighting. People need to get their heads out of the bottle and start demanding greener policies.
Amanda Hamlet
October 17, 2025Listen, I’ve read every clinical trial on allergic conjunctivitis, so let me set the record straight. The “environmental controls” section is superficial; real mitigation requires municipal pollen monitoring, not just personal sunglasses. Also, the suggested eye‑drop regimen is a one‑size‑fits‑all, which is scientifically inaccurate. Finally, you’re all ignoring the emerging research on monoclonal antibodies that could revolutionize treatment.
Nolan Jones
October 19, 2025Dude, I just skimmed through the long post above, and I gotta say, it’s solid but a bit dense. For anyone feeling overwhelmed, start with the easy wins: keep windows shut on high pollen days and use those wrap‑around shades. It’s not rocket science, and you’ll notice less itching that way. Also, don’t forget to have a bottle of combo drops handy – they’re a game‑changer. Just remember, consistency beats occasional use.
Jada Singleton
October 20, 2025The article’s tone oscillates between overly optimistic and alarmist, which may mislead readers about the severity of allergic conjunctivitis. It’s essential to maintain an objective stance, presenting both benefits and risks of each therapeutic option. Moreover, the piece could have cited more recent meta‑analyses to substantiate its claims. As it stands, the narrative feels somewhat biased toward pharmacologic intervention.
Emily Rossiter
October 21, 2025I appreciate the comprehensive checklist; it gives patients clear actionable steps. It’s also helpful that the article emphasizes starting treatment before symptoms flare. Keeping the information straightforward makes it easier for non‑specialists to follow. Great job staying clear and concise.
Renee van Baar
October 22, 2025Balancing the need for prompt relief with long‑term management is key, and this article does a commendable job outlining both. The inclusion of environmental strategies alongside pharmacotherapy reflects a holistic approach. While the text is thorough, a brief summary at the end would aid quick reference for busy readers. Overall, a valuable resource that could benefit from a few visual aids.
Mithun Paul
October 24, 2025The dissection of treatment modalities is analytically sound, yet the author neglects to address the economic implications for patients in low‑income brackets. A brief discussion on generic alternatives would enhance the article’s applicability. Nonetheless, the data-driven approach remains rigorous.
Sandy Martin
October 25, 2025Reading through the recommendations reminded me of my own battle with seasonal eye irritation. I found the part about using HEPA filters particularly useful, as it’s a simple change that made a noticeable difference for me. Also, the advice to start drops early saved me from a week of constant itching last year.
Steve Smilie
October 26, 2025One must admire the article’s eloquent prose, though it borders on pedantry at times. The author’s penchant for exhaustive tables is impressive, yet a more narrative style could engage a broader audience. Still, the scholarly rigor is evident throughout.
Josie McManus
October 27, 2025I totally feel you on the struggle-my eyes have been a mess every spring. The checklist is super helpful; I’m already buying some cheap wrap‑around glasses and setting up a reminder to start my drops early. Let’s keep each other motivated and share what works best for our eyes.