Surviving a heart attack is just the beginning. What comes next-how you eat, what pills you take, and how you move-can mean the difference between living well for years or facing another crisis. The truth is, recovery isn’t about going back to how things were. It’s about building a new normal, one that protects your heart for good.
Medications: Your Daily Shield
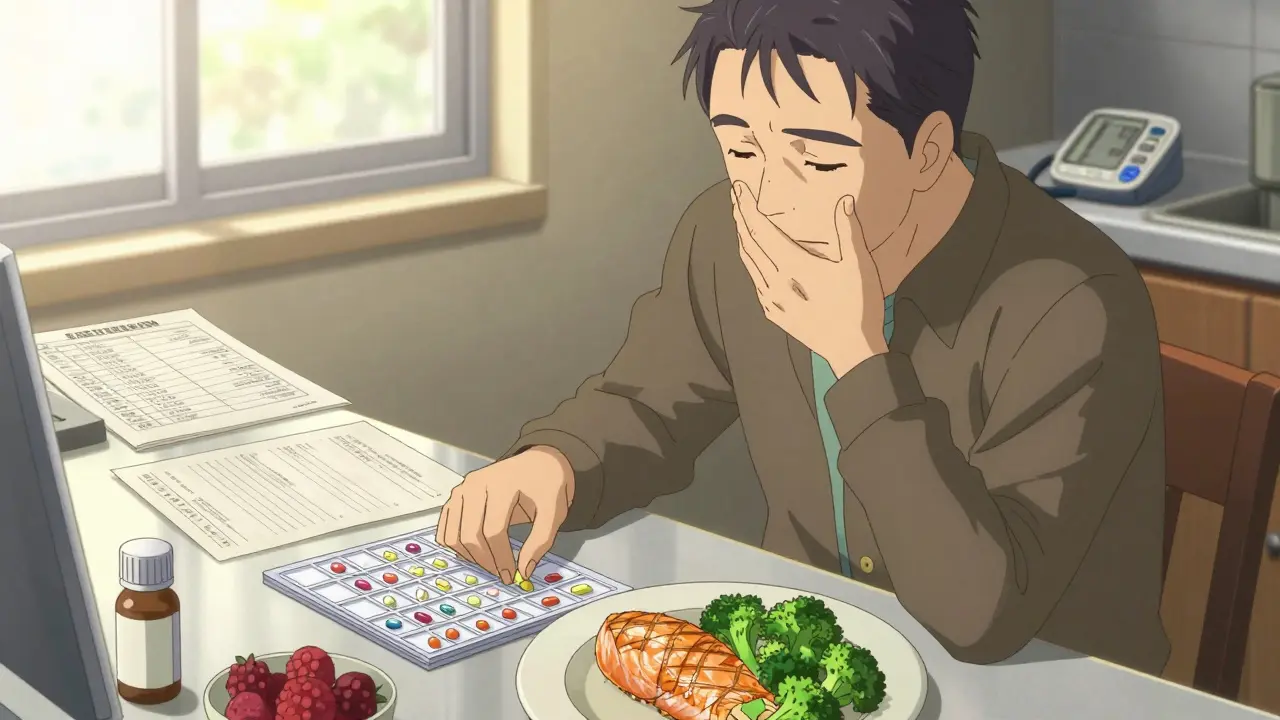
Right after a heart attack, your medical team will start you on a mix of medicines. These aren’t optional. They’re your first line of defense against another event. You’ll likely be on at least four types: aspirin to stop clots, a statin to lower cholesterol, a beta-blocker to reduce heart strain, and an ACE inhibitor or ARB to help your heart heal and lower blood pressure. Some may also need a blood thinner like rivaroxaban or clopidogrel, especially if stents were placed.
It’s easy to forget pills. You might feel fine. You might think, “I don’t need this anymore.” But your heart is still healing, and those medicines are working behind the scenes. Missing doses raises your risk of another heart attack by up to 40%, according to NHS data. Keep a written list of every medication, the dose, and why you’re taking it. Carry it with you. Show it to every doctor, even your dentist.
Pharmacists are your allies here. Many hospitals now include them in your recovery team. They can explain side effects-like fatigue from beta-blockers or a dry cough from ACE inhibitors-and help you find cheaper generics if cost is a problem. Don’t stop or change anything without talking to your doctor first. Even herbal supplements can interfere. Garlic pills, St. John’s wort, or high-dose fish oil? Ask before you take them.
Diet: Food as Medicine
After a heart attack, your plate becomes a tool for healing. You don’t need to eat bland, boring food. You need to eat smart. The goal is to reduce inflammation, lower bad cholesterol, and keep blood pressure in check.
Start by cutting out processed foods. That means no sugary cereals, packaged snacks, frozen meals, or fast food. These are loaded with sodium, hidden sugars, and unhealthy fats. Instead, fill half your plate with vegetables and fruits-especially leafy greens, berries, apples, and oranges. They’re rich in fiber and antioxidants that help your arteries stay flexible.
Choose whole grains over white bread and pasta. Brown rice, oats, quinoa, and barley help stabilize blood sugar and reduce plaque buildup. For protein, go for fish like salmon, mackerel, or sardines at least twice a week. They’re full of omega-3s, which lower triglycerides and reduce heart rhythm problems. Swap butter for olive oil. Use nuts and seeds as snacks, not chips. A small handful of almonds or walnuts daily has been shown to improve artery function.
Watch your salt. The NHS recommends less than 6g per day-about one teaspoon. That’s harder than it sounds. Soy sauce, canned soups, bread, and even breakfast cereals can be salt bombs. Read labels. Look for “low sodium” or “no added salt.” Cook at home more. That’s your best shot at control.
A registered dietitian will work with you in cardiac rehab. They’ll tailor your plan to your culture, tastes, and health needs. Maybe you love Indian curries? They’ll help you make them with less oil and more lentils. You’re not being punished-you’re being empowered.

Activity: Moving Back to Life
You’ll feel tired. Weak. Maybe even scared to move. That’s normal. Your heart muscle was damaged. It needs rest. But too much rest? That’s dangerous. Inactivity weakens your heart even more and raises your risk of blood clots and depression.
Start small. In the first week home, walk around your house. Go up and down the stairs slowly. Sit in a chair for 10 minutes, then stand. Gradually, add five more minutes of walking each day. By week two, aim for 10-15 minutes of slow walking outside. Use a pedometer or phone app. Don’t chase steps-focus on consistency.
Cardiac rehab is the gold standard. It’s not a gym. It’s a supervised program, usually three times a week for 6-12 weeks. You’ll do light cardio on a stationary bike or treadmill, with your heart rate and blood pressure monitored. You’ll learn how hard you can safely push. You’ll also get advice on breathing, pacing, and recognizing warning signs-like chest pain, dizziness, or unusual shortness of breath.
Once you’re cleared, aim for 150 minutes of moderate aerobic activity per week. That’s 30 minutes, five days a week. Walking, swimming, cycling, or dancing-all count. Strength training twice a week helps too. Use light weights or resistance bands. It improves muscle function, which takes pressure off your heart.
Don’t rush. Recovery isn’t a race. Some people feel better in two weeks. Others need three months. Listen to your body. If you’re exhausted the next day, you did too much. Rest. Try again tomorrow.
Cardiac Rehabilitation: Your Recovery Roadmap
Cardiac rehab is the glue that holds everything together. It’s not just exercise. It’s education, emotional support, and a structured plan made just for you. The NHS calls it one of the two most important parts of recovery. The other? Reducing future risk.
In rehab, you’ll meet nurses, physiotherapists, dietitians, and counselors. They’ll help you understand your diagnosis, manage stress, and deal with anxiety. Many people feel guilty or scared after a heart attack. That’s normal. Rehab gives you space to talk about it.
Programs are tailored. If you’re 70 and have arthritis, your exercises will be different from a 50-year-old with no joint issues. If you’re diabetic, your diet plan will reflect that. If you live alone, they’ll help you set up safety measures at home.
Studies show people who complete cardiac rehab are 25-30% less likely to die from heart problems in the next five years. They also return to work sooner and report better quality of life. It’s not a luxury. It’s essential care.
Follow-Up and Long-Term Thinking
You’ll have a check-up four to six weeks after leaving the hospital. Your doctor will check your blood pressure, cholesterol, and how you’re feeling. Blood tests will show if your medicines are working. An ECG or echocardiogram might be repeated to see how your heart is healing.
After that, you’ll likely see your cardiologist every three to six months. Keep those appointments. Even if you feel fine. Your heart can quietly worsen without symptoms.
Long-term, your goal is to make these changes permanent. That means keeping your meds, sticking to your diet, and staying active-even when life gets busy. It also means knowing your risk factors. Age and family history? You can’t change those. But smoking? You can quit. High blood pressure? You can manage it. Obesity? You can lose weight. Diabetes? You can control it.
And don’t forget your mental health. Depression after a heart attack is common. It’s not weakness. It’s a reaction to trauma. If you’re feeling down, hopeless, or unable to sleep, tell someone. Cardiac rehab teams offer counseling. Your GP can refer you to a therapist. You deserve to feel whole again.
What to Watch For
Know the warning signs of another heart attack. They’re not always the same. Chest pain is classic-but not everyone feels it. Watch for:
- Unexplained fatigue that lasts days
- Shortness of breath when resting
- Dizziness or fainting
- Swelling in ankles, legs, or belly
- Irregular heartbeat-fluttering, pounding, or skipping
If any of these happen, call 111 or go to A&E. Don’t wait. Don’t assume it’s just stress. Your heart might be sending a signal.
Recovery after a heart attack isn’t about perfection. It’s about progress. Some days will be hard. Some pills will make you feel off. Some meals will feel boring. But every small choice-you walking today, you choosing grilled fish over fried chicken, you taking your medicine-adds up. You’re not just surviving. You’re rebuilding. And that’s powerful.
How long does it take to recover from a heart attack?
Recovery varies. Most people feel ready to return to light daily activities within two to six weeks. Full recovery-meaning you can resume normal work and exercise-often takes three months. But it depends on how much damage the heart took, your age, other health conditions, and whether you join cardiac rehab. The NHS advises not to rush; healing takes time.
Can I drive after a heart attack?
You must stop driving for at least one week after a heart attack. If you drive a car or motorcycle, you can usually start again after four weeks if you’re feeling well and have no complications. If you drive a large vehicle (like a truck or bus), you’ll need to inform the DVLA and may need a medical assessment. Always check with your doctor before getting behind the wheel.
Are there foods I should never eat again?
You don’t need to ban everything forever, but some foods should be rare. Avoid fried foods, sugary drinks, processed meats like bacon and sausages, and foods with trans fats (check labels for “partially hydrogenated oils”). Limit salt to under 6g per day. You can still enjoy treats occasionally-just not daily. Focus on balance, not perfection.
Can I have sex after a heart attack?
Yes, most people can resume sexual activity within a few weeks, once they can climb two flights of stairs without chest pain or shortness of breath. Sex is a moderate physical activity-similar to walking briskly. If you’re on medications like nitrates, don’t take erectile dysfunction drugs like Viagra without talking to your doctor. They can cause dangerous drops in blood pressure.
What if I can’t afford my medications?
In the UK, prescription charges are capped, and many heart medications are free for people with long-term conditions. Ask your GP for a medical exemption certificate. If you’re still struggling, speak to your pharmacist-they can help you switch to cheaper generics or connect you with patient assistance programs. Never skip doses because of cost. There are always options.





9 Comments
Bryan Wolfe
January 12, 2026Just finished my 8th week of cardiac rehab and I can’t believe how much stronger I feel-like, seriously, I walked up three flights of stairs today without stopping. I used to think I’d never climb stairs again after my MI, but this program? Life-changing. Also, my pharmacist hooked me up with generic versions of everything and saved me $200/month. Don’t let cost scare you off-there’s always a way.
Sumit Sharma
January 13, 2026The statin compliance rate post-MI in India is less than 32% due to cultural stigma and lack of physician follow-up. This is unacceptable. Patients must understand that LDL-C <70 mg/dL is the target, not ‘feeling fine.’ Beta-blockers reduce mortality by 23% at 1 year-this isn’t optional. If you’re skipping doses because you ‘feel okay,’ you’re gambling with your life. Evidence-based medicine isn’t a suggestion-it’s protocol.
Jay Powers
January 15, 2026I was skeptical about cardiac rehab at first. Thought it was just fancy walking. Turns out it’s the only place I felt safe talking about how scared I was. My nurse noticed I was holding back and asked if I’d ever cried since the hospital. I broke down. We didn’t fix my heart that day-but we started fixing me. Everyone deserves that kind of care. No shame in needing it.
Lawrence Jung
January 16, 2026Medications are a crutch for the weak-minded. The real solution is discipline. Stop eating. Move more. Stop blaming pills. You don’t need a dietitian to tell you not to eat fried chicken. You need willpower. And if you can’t muster that? Then maybe you weren’t meant to survive. The heart doesn’t care about your excuses. It just beats-or it doesn’t.
Alice Elanora Shepherd
January 17, 2026Just wanted to add: if you’re on an ACE inhibitor and get that dry cough-don’t just suffer through it. Talk to your GP about switching to an ARB. It’s the same benefit, no cough. Also, if you’re struggling with salt, try potassium-rich foods like sweet potatoes, spinach, and bananas-they help counterbalance sodium. And please, please-keep a meds log. I’ve seen too many people end up back in A&E because they mixed up their pills. Write it down. Even if you think you’ll remember.
Christina Widodo
January 18, 2026Can someone explain why fish oil supplements aren’t recommended? I’ve read conflicting things. I’m on a statin, but I’ve been taking 2000mg of omega-3 daily. Is that okay? Or should I cut it out? I’m confused.
Prachi Chauhan
January 19, 2026After my husband’s heart attack, we stopped eating rice every day. Now we eat dal, roti, and lots of greens. It’s not hard. You just change one thing at a time. First, no fried samosas. Then, no sugar in tea. Then, walk after dinner. Small steps. Heart doesn’t care about big changes. It cares about you showing up.
beth cordell
January 19, 2026Just started cardiac rehab and I’m crying happy tears 😭 I literally didn’t think I’d ever dance again. Today I did a slow waltz with my husband. He said I looked beautiful. I felt like me again. Thank you for writing this. I needed to know I’m not alone.
Lauren Warner
January 20, 2026You people are so naive. Cardiac rehab is a money grab. The NHS doesn’t care about you. They just want you to take your pills and shut up. You think eating kale is going to fix years of bad habits? Wake up. The system is rigged. Your heart is a broken machine. You’re just delaying the inevitable.