Hyponatremia Risk Calculator for Older Adults
This tool estimates your risk of developing hyponatremia (low sodium levels) while taking SSRIs based on factors discussed in the article. It is not a substitute for medical advice. Always consult your doctor.
Every year, hundreds of thousands of older adults in the U.S. start taking SSRIs to manage depression or anxiety. These medications help many feel better-but for some, they bring hidden dangers. The biggest risks? Hyponatremia and falls. Both can turn a simple treatment into a life-threatening event. And the worst part? Many of these cases are preventable.
What Is Hyponatremia-and Why Does It Happen With SSRIs?
Hyponatremia means your blood sodium level drops too low-below 135 mmol/L. Sodium is crucial for keeping your nerves, muscles, and fluids balanced. When it dips, your body holds onto too much water. That’s exactly what SSRIs can trigger. SSRIs cause something called SIADH-Syndrome of Inappropriate Antidiuretic Hormone Secretion. Normally, your kidneys adjust how much water they keep or flush out. But with SSRIs, your body keeps releasing too much ADH (antidiuretic hormone), so your kidneys hang onto water like a sponge. That dilutes the sodium in your blood. This doesn’t happen to everyone. But in older adults, it’s far more likely. Why? Because aging changes how your body handles fluids. You have less total body water. Your kidneys don’t filter as well. Your hormones don’t respond as sharply. All of this makes you more sensitive to even small changes in sodium. Studies show older adults on SSRIs are more than twice as likely to develop hyponatremia compared to those not taking these drugs. About 6 out of every 100 seniors on SSRIs will have low sodium levels. In about 1 out of 100, it gets severe enough to cause confusion, seizures, or coma.Which SSRIs Carry the Highest Risk?
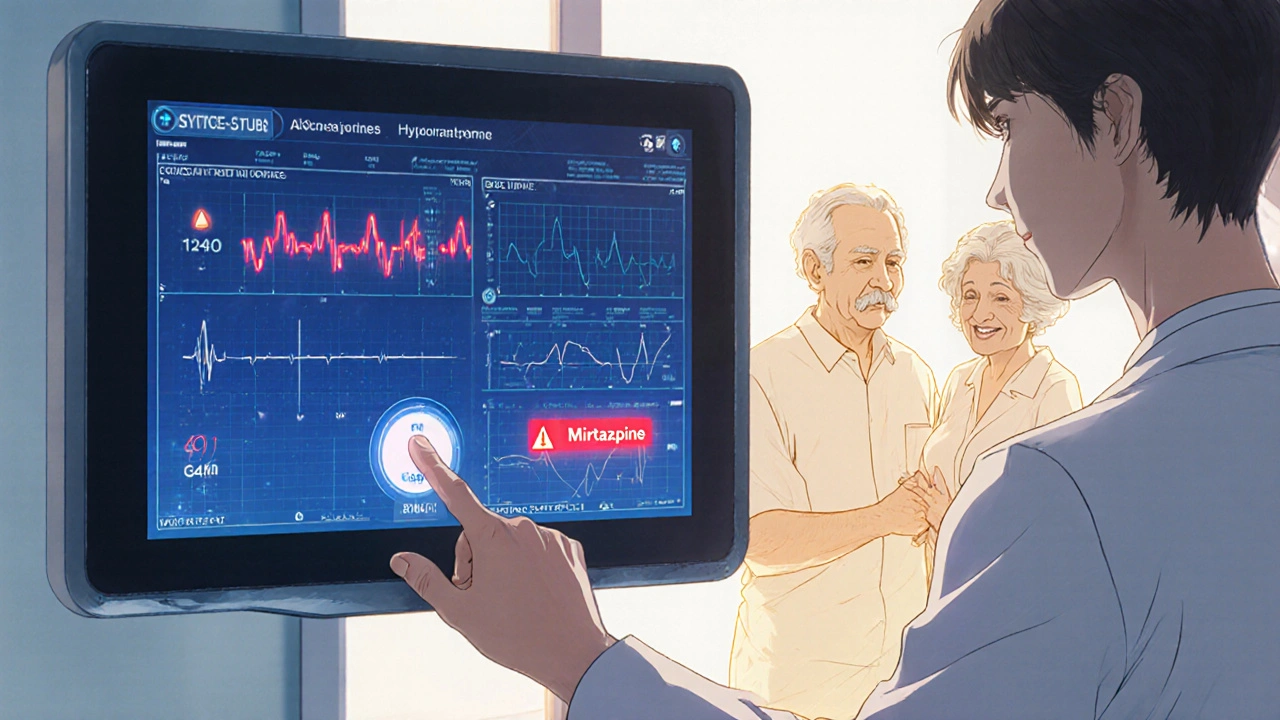
Not all SSRIs are created equal when it comes to hyponatremia risk. Fluoxetine (Prozac) has the highest reported risk among SSRIs-nearly 3.6 times more likely to cause low sodium than other antidepressants. Sertraline (Zoloft) and paroxetine (Paxil) also carry moderate risk. Escitalopram (Lexapro) and citalopram (Celexa) are a bit safer, but still risky for older adults. Even SNRIs like venlafaxine (Effexor) are worse than most SSRIs. If you’re over 65 and your doctor suggests an antidepressant, knowing which one carries the least risk matters. Mirtazapine (Remeron) is often the best alternative. It’s not an SSRI, and studies show it rarely causes hyponatremia. Bupropion (Wellbutrin) is another option with low sodium risk-but it doesn’t work as well for everyone, especially those with severe anxiety.Who’s Most at Risk?
Some people are far more likely to develop hyponatremia on SSRIs. Watch out if you have:- Low starting sodium levels (below 140 mmol/L)
- Body weight under 68 kg (150 lbs)-especially if you’re female
- Take a thiazide diuretic (like hydrochlorothiazide) for high blood pressure
- Have kidney problems or heart failure
- Started or increased your SSRI dose in the last 2-4 weeks

How Hyponatremia Leads to Falls
Low sodium doesn’t always cause obvious symptoms like nausea or vomiting. In older adults, it often shows up as:- Dizziness when standing up
- Feeling weak or unsteady on your feet
- Confusion or trouble thinking clearly
- Falling more often than usual
What Should Doctors Do? (And What They Often Don’t)
Experts agree: Before starting an SSRI, check the patient’s sodium level. Then check it again two weeks later. That’s the bare minimum. But here’s the problem: Many doctors don’t do this. A 2023 study found that while 80% of clinics have guidelines for sodium monitoring in seniors on SSRIs, only about 30% actually follow them. Why? Time. Cost. Lack of reminders in electronic health records. Some hospitals have fixed this. Johns Hopkins Bayview Medical Center added automated alerts in their system. When a doctor prescribes an SSRI to someone over 65, the system flags: “Check sodium before and at 2 weeks.” They saw a 22% drop in ER visits for hyponatremia within a year. The American Society of Health-System Pharmacists created a tool now used in over 120 hospitals that automatically warns doctors if they prescribe an SSRI with a thiazide diuretic. That alone cut risky prescriptions by nearly 19%. Yet, many primary care doctors still don’t know about these tools-or aren’t using them.What You Can Do as a Patient or Family Member
You don’t need to wait for your doctor to act. Here’s what you can do:- Ask for a blood test before starting any SSRI. Request a basic metabolic panel (BMP)-it includes sodium.
- Ask for a repeat test two weeks after starting or after any dose increase.
- Know the warning signs: dizziness, confusion, weakness, frequent stumbling. Don’t brush them off as “just aging.”
- Review all medications. If you’re on a water pill (hydrochlorothiazide, chlorthalidone), ask if it’s safe with your antidepressant.
- Ask about alternatives. If you’re high-risk, ask if mirtazapine or bupropion might be better.
The Big Contradiction: Why Monitoring Alone Isn’t Enough
Here’s the frustrating part. A 2023 study showed that even when doctors followed the guidelines and checked sodium levels, it didn’t reduce hospitalizations. Why? Because finding low sodium isn’t the end-it’s the beginning. If you detect it but don’t act, nothing changes. The real solution isn’t just testing. It’s:- Stopping the SSRI if sodium drops below 130
- Restricting fluid intake if it’s mild
- Switching to a safer antidepressant
- Monitoring closely for signs of worsening symptoms
What’s New in 2025?
New tools are emerging. The Geriatric Antidepressant Safety Collaborative launched an AI tool that predicts who’s most at risk. It looks at age, sodium levels, fall history, kidney function, and current meds-and flags high-risk patients before they even start an SSRI. The American Geriatrics Society updated its guidelines in 2024 to say: “Consider fall history when choosing an antidepressant.” That’s huge. For the first time, doctors are being told to think about mobility-not just mood-when prescribing. And the NIH just funded a $2.8 million study to finally answer the question: What monitoring protocol actually saves lives? Results aren’t due until 2027, but the hope is clear: better rules, better tools, better outcomes.Bottom Line: Safety Comes Before Speed
SSRIs can help older adults feel like themselves again. But they’re not harmless. The risk of hyponatremia-and the falls that follow-is real, preventable, and often ignored. If you or someone you love is on an SSRI:- Don’t assume it’s safe just because it’s common.
- Don’t wait for symptoms to appear.
- Ask for sodium testing before and after starting.
- Speak up if dizziness or falls start happening.
- Ask about safer alternatives.
8 Comments
Matthew Williams
November 1, 2025So let me get this straight-we’re giving old people antidepressants that make them fall over, and the medical system is too lazy to check sodium levels? Classic. I’ve seen this with my dad. Doctor handed him Prozac like it was candy, no blood test, no warning. Two weeks later he’s in the ER after sliding down the stairs. They called it ‘old age.’ Bullshit. It’s negligence wrapped in a white coat.
And don’t even get me started on the ‘alternative meds’-mirtazapine? Sure, if you want your grandpa to sleep 18 hours a day and eat his weight in chips. Bupropion? Good luck with that if he’s got anxiety. This isn’t a menu, it’s a minefield.
Meanwhile, Big Pharma’s laughing all the way to the bank while nursing homes fill up with broken hips. Someone needs to sue the entire geriatric psych pipeline.
And no, ‘just monitor’ doesn’t cut it. Monitoring is just a paper trail for when the lawsuit happens. Action is what saves lives. Stop treating seniors like lab rats with a pulse.
Dave Collins
November 2, 2025Oh wow, a 12-page pamphlet disguised as a Reddit post. Did you write this for your med school presentation? Or just copy-paste the entire American Journal of Geriatric Psychiatry? Congrats, you’ve turned depression into a public health crisis worthy of a CDC bulletin.
Let me guess-next you’ll tell us to check for vitamin D deficiency before giving someone a coffee. Maybe we should also require a background check on their socks before prescribing SSRIs.
Meanwhile, actual people are getting better. Not ‘less likely to fall.’ Not ‘sodium levels optimized.’ Better. Happier. Alive. Not just surviving. Living.
Stop pathologizing aging. Sometimes people get dizzy because they’re 72, not because their kidneys are conspiring against them.
Suresh Patil
November 3, 2025In India, many elderly take antidepressants without regular blood tests-because access to labs is limited, and family often manages care at home. We don’t have automated alerts or NIH-funded studies. But we do have patience, observation, and quiet vigilance.
My grandmother took sertraline for three years. My mother watched her closely: if she stumbled, we cut back fluids. If she seemed foggy, we waited a week before the next pill. No doctor visits, no alarms-just love and attention.
Maybe the real solution isn’t more tech, but more presence. Not every risk needs a protocol. Sometimes it just needs someone who notices.
Ram Babu S
November 4, 2025Respect to the author for laying this out clearly. I’m a caregiver for my uncle-he’s 78, on Zoloft, and had two falls last winter. We didn’t connect it to the med until his niece (a nurse) asked about sodium. Turned out his level was 131. We switched to mirtazapine. No more dizziness. He’s back to gardening.
It’s not about fear. It’s about awareness. And awareness starts with asking questions. Even if the doctor rolls their eyes.
Also, if you’re on hydrochlorothiazide? Ask. Just ask. It’s that simple. No shame in being the one who speaks up.
Kyle Buck
November 5, 2025The pathophysiological cascade initiated by SSRI-induced SIADH is a well-documented phenomenon in geriatric pharmacology, particularly in the context of age-related decline in renal concentrating capacity and reduced total body water composition. The clinical implications of hyponatremia, particularly in the context of neuromuscular destabilization and postural instability, are not merely correlative but causally linked to increased fall risk, as evidenced by longitudinal cohort analyses from the Framingham Heart Study and the Health ABC Study.
Furthermore, the pharmacodynamic variability among SSRIs-particularly the differential affinity for the serotonin transporter and subsequent modulation of ADH secretion-warrants stratified prescribing algorithms. The absence of standardized electronic health record (EHR) decision support systems remains a critical systemic failure in primary care delivery.
While patient advocacy is commendable, the structural imperative lies in institutional implementation of protocol-driven pre- and post-prescription electrolyte monitoring, ideally integrated with pharmacogenomic risk profiling for CYP2D6 and CYP2C19 polymorphisms.
Amy Craine
November 7, 2025I’m a nurse practitioner in a geriatric clinic, and I can tell you-this post nails it. We started doing mandatory BMPs before SSRIs six months ago. We also have a checklist: ‘Any recent falls? On diuretics? Weight under 150?’
Within three months, we cut our hyponatremia cases in half. Not because we’re geniuses. Because we finally stopped assuming ‘it’s just aging.’
And yes, we talk to patients like humans. We say: ‘This med helps your mood, but it can make you wobbly. Let’s check your numbers before you start-and again in two weeks. If you feel off, call us. Don’t wait.’
It’s not complicated. It’s just care. And care shouldn’t be optional.
Alicia Buchter
November 8, 2025Ugh. I just got off a Zoom call with my mom’s ‘wellness coach’ who told her to ‘try natural remedies’ for depression instead of meds. Then she switched her to St. John’s Wort-which she’s now taking with a thiazide diuretic. And she’s 74. And she fell last Tuesday.
So now I’m the villain for pushing SSRIs. But if I don’t, she’ll be on some ‘herbal tea’ that interacts with her blood pressure meds and ends up in a nursing home.
Why is it that the people who know the least about medicine are the loudest about it? And why does everyone think ‘natural’ means ‘safe’? My grandma’s tea killed her. Her ‘natural’ remedy was a lethal cocktail of hawthorn and hydrochlorothiazide.
Stop romanticizing ignorance. This isn’t a yoga retreat. It’s a hospital waiting to happen.
MaKayla VanMeter
November 10, 2025This is why I don’t trust doctors. 😭