When a pharmacist hands you a new prescription, they’re not just giving you pills-they’re giving you instructions for your health. But too often, that moment feels rushed. You get a pill bottle, a printed sheet, and maybe a quick "Take this twice a day." That’s not counseling. That’s compliance. Real counseling-pharmacist counseling scripts-is what turns that moment into a chance to actually improve how people use their meds.
Why Scripts Matter More Than You Think
Pharmacist counseling isn’t optional. Since 1990, the Omnibus Budget Reconciliation Act (OBRA '90) made it a legal requirement for Medicaid patients to receive counseling when picking up prescriptions. But the law didn’t say how to do it. That’s where scripts came in. They weren’t meant to be read like teleprompters. They were meant to be frameworks-so no patient gets skipped, no key detail gets missed, and no pharmacist has to guess what to say next. In high-volume pharmacies, where pharmacists might see 150 patients a day, scripts keep things consistent. A 2022 study found that using a basic three-question script cut average counseling time from 4.2 minutes to 2.9 minutes-without lowering quality. That’s not just efficiency. It’s safety.The Core Three: What Every Script Must Include
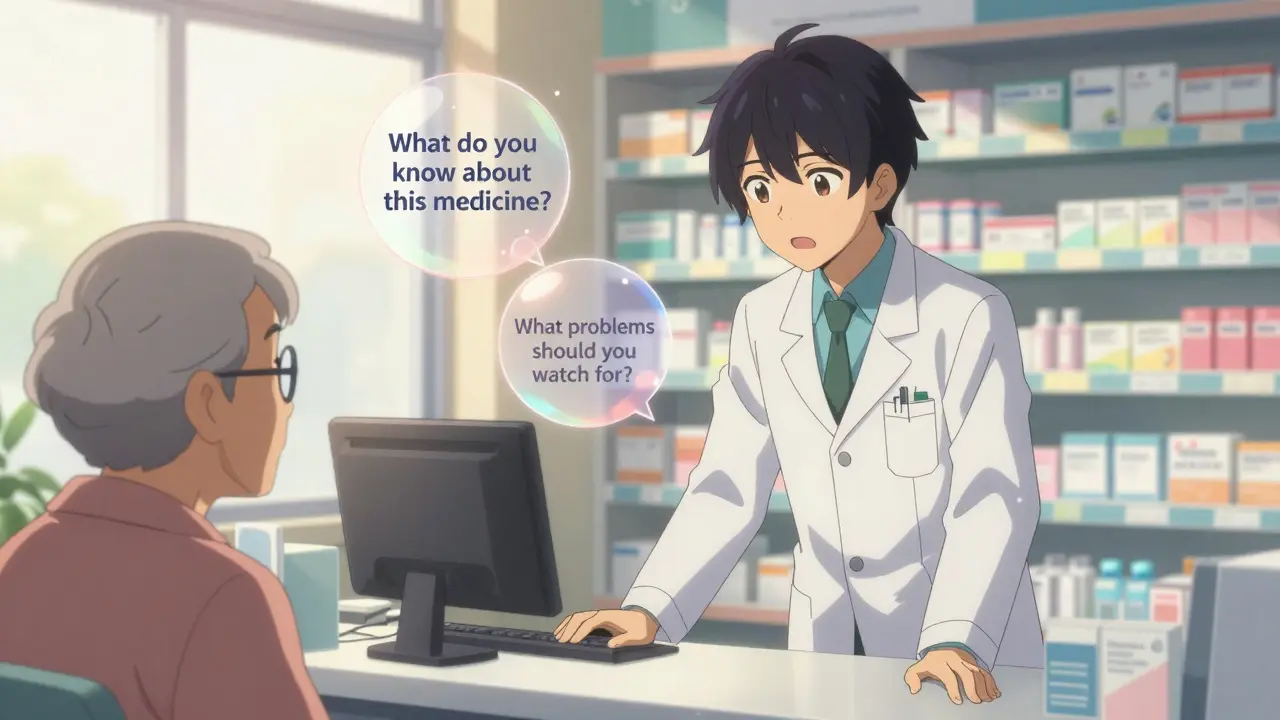
The most trusted model comes from the Indian Health Service, cited in over 9 academic studies. It’s simple, but powerful:- What do you know about this medicine? This isn’t a test. It’s a starting point. Maybe the patient thinks it’s for headaches, but it’s actually for high blood pressure. Or they’ve never heard the name before. You need to know where they are before you can help them move forward.
- How do you take it? Sounds basic, right? But studies show nearly 40% of patients misunderstand dosage instructions. Is it once daily or twice? With food or on an empty stomach? Should they swallow it whole or crush it? One wrong answer can mean hospitalization.
- What problems should you watch for? Not every side effect. Just the serious ones. If they’re on warfarin, they need to know about unusual bruising. If they’re on opioids, they need to know about breathing trouble and naloxone. This is where scripts save lives.
How Scripts Evolve From Training to Real Life
New pharmacists start by learning scripts word-for-word. That’s how you build confidence. But the goal isn’t to sound like a robot. It’s to internalize the structure so you can adapt it. Dr. Daniel Holdford, who studied this in 2006, put it plainly: "Scripts help inexperienced students learn. As experience grows, they adapt the script to their own style." That’s the sweet spot. You don’t throw away the script. You make it yours. A good pharmacist doesn’t say, "This is lisinopril, 10 mg, take one daily." They say, "This is a blood pressure pill. You take it every morning, even if you feel fine. Some people get a dry cough-nothing to panic about, but let me know if it lasts more than a week. Have you ever taken something like this before?" That’s the difference between reading and connecting.
What Scripts Don’t Cover (And Why That’s a Problem)
Scripts work best for routine meds: antibiotics, blood pressure pills, diabetes drugs. But they fall apart in complex cases. Take anticoagulants. Warfarin isn’t just about "take once a day." It’s about diet, alcohol, other meds, bleeding signs, INR checks. A generic script won’t cut it. That’s why specialized training exists-like the ones for opioids, mental health meds, or injectables. And then there’s the documentation. OBRA '90 doesn’t just require counseling-it requires proof. Pharmacists must record: Was counseling offered? Was it accepted? Did the patient understand? Many pharmacies use EHR checkboxes now. But checking "understood" doesn’t mean they did. That’s why the teach-back method matters. Teach-back means asking the patient to explain it back in their own words. Not "Do you understand?" That’s a yes/no trap. Try: "Can you tell me how you’ll take this pill tomorrow?" If they say, "I’ll take it when I remember," you’ve found your gap. Then you fix it.Where Scripts Fail-And How to Fix Them
The biggest complaint from pharmacists? "Script fatigue." A 2022 survey found 42% of community pharmacists felt burned out by corporate-mandated scripts that didn’t account for literacy levels, language barriers, or emotional states. One script for a 75-year-old with three chronic conditions? Same as for a 22-year-old getting birth control? That’s not counseling. That’s checkbox farming. Solutions? Two things:- Language access. Over 150 languages are available through services like Language Access Network. Pre-printed, translated sheets for common meds are now standard in many pharmacies.
- Flexible templates. Instead of one rigid script, use modular ones. Core questions stay the same. Details change based on the patient’s age, condition, or culture. A script for a refugee might include family involvement. One for a teen might use analogies they relate to.
The Real Cost of Not Doing It Right
Medication non-adherence isn’t just a "problem." It’s a $312 billion problem in the U.S. every year. That’s more than the entire annual budget of the CDC. People skip doses. They mix meds. They stop because they’re scared, confused, or embarrassed to ask. Pharmacist counseling reduces hospitalizations. Reduces ER visits. Reduces waste. A 2023 study showed that when pharmacists used structured scripts with teach-back, adherence rates jumped by 27% for chronic disease meds. And it’s getting more important. By 2025, Medicare Part D will require documented proof of patient comprehension. Not just "counseling happened." But "the patient can explain it." That’s going to force every pharmacy to upgrade their scripts.What’s Next for Counseling Scripts
The future isn’t more scripts. It’s smarter ones. Pilot programs at CVS and Walgreens are testing AI-assisted dynamic scripts. These tools listen to patient responses and adjust the next question in real time. If a patient says, "I’m worried about gaining weight," the system suggests adding a line about appetite changes and alternatives. Early results? 23% higher patient comprehension scores. Meanwhile, Ireland’s 2024 guidelines are pushing for "concordance"-counseling as a conversation, not a checklist. The U.S. is slowly moving that way too. The goal isn’t to check boxes. It’s to build trust.How to Get Started
If you’re a pharmacy student, start with the three-question model. Practice it with classmates. Record yourself. Then ask: Did I learn what they knew? Did I find out what they didn’t? Did I leave them feeling heard? If you’re a practicing pharmacist, audit your current scripts. Are they written for the patient-or the regulator? Can a 6th grader understand them? Are they flexible enough for someone who speaks English as a second language? And if you’re a pharmacy owner? Don’t buy the cheapest script software. Look for ones that let you customize, integrate with your EHR, and track outcomes-not just compliance. Counseling isn’t a task. It’s the reason people trust you with their health. And scripts? They’re not the enemy. They’re the scaffold. Build on them. Don’t just follow them.Are pharmacist counseling scripts mandatory by law?
Yes, under OBRA '90, pharmacists must offer counseling to Medicaid patients. Many states have gone further and require actual counseling-not just an offer-for all prescriptions. Medicare Part D also requires proof of patient understanding by 2025. It’s not optional anymore.
What’s the teach-back method, and why is it important?
Teach-back means asking the patient to explain the instructions back in their own words. Instead of "Do you understand?" you say, "Can you tell me how you’ll take this pill?" This catches misunderstandings before they become problems. Studies show it improves adherence by up to 27%.
Can I use the same script for every patient?
No. A script for a teenager on birth control is different from one for an elderly person on five medications. Generic scripts work for routine meds, but complex conditions like diabetes, anticoagulation, or mental health need specialized versions. The best scripts are flexible templates, not rigid scripts.
How do language barriers affect counseling?
Language barriers are one of the biggest reasons counseling fails. Many pharmacies now use pre-translated materials in over 150 languages and telephonic interpretation services. Never rely on family members to translate-especially for meds. Misunderstandings can be deadly.
Do I need special training to use counseling scripts?
Yes. Most pharmacy schools require 8-12 weeks of supervised practice to move from reading scripts to adapting them. The American Society of Consultant Pharmacists recommends 15 hours of annual continuing education focused on counseling skills. It’s not just about knowing the drugs-it’s about knowing how to talk to people.
What’s the difference between ASHP and CMS counseling guidelines?
ASHP focuses on pharmaceutical care-what’s best for the patient. CMS focuses on legal compliance-what’s required by law. ASHP’s guidelines are more detailed and patient-centered. CMS’s are simpler and built around OBRA '90. Most pharmacies use a hybrid: ASHP’s structure with CMS’s documentation.
How do I know if my counseling is working?
Track adherence. If patients refill their meds on time, they’re probably following instructions. Look at hospital readmission rates for chronic conditions. Ask for feedback. Some pharmacies now use the Pharmacist Counseling Outcomes Registry to measure real-world results like blood pressure control or A1C levels after counseling.
Are there free counseling scripts I can use?
Yes. The Indian Health Service’s three-question model is publicly available and widely used. ASHP and CMS also publish free guidelines online. Many state pharmacy associations offer downloadable templates. Avoid commercial scripts unless they let you customize them. The best ones are simple, adaptable, and patient-focused.





9 Comments
Lydia H.
January 19, 2026Man, I’ve seen pharmacists rush through counseling like they’re on a clock. But this? This is the real deal. The three-question model? Genius. It’s not about checking boxes-it’s about listening. I had a pharmacist ask me, 'What do you know about this?' and I said, 'I think it’s for anxiety.' Turns out it was for migraines. She didn’t laugh. She just smiled and said, 'Okay, let’s start from there.' That’s the difference.
Jake Rudin
January 20, 2026Scripts… as scaffolds… not shackles… yes… this is the epistemological pivot… the pharmakon… both remedy and poison… when reduced to corporate checkboxes… they become instruments of alienation… but when internalized… as lived praxis… they become the very architecture of trust…
Tracy Howard
January 21, 2026Ugh. I’ve had pharmacists in Canada use these ‘scripts’ like they’re reading a cereal box. ‘Take it twice a day.’ No context. No empathy. No ‘what do you know?’-just a robot with a stethoscope. And now you’re telling me this is the gold standard? Please. If you’re not tailoring it to someone’s life, their culture, their trauma-then you’re not counseling. You’re compliance theater. And if your pharmacy thinks a translated sheet fixes everything? You’re still failing. Language isn’t a checkbox. It’s a bridge. And you’re building it with duct tape.
Josh Kenna
January 21, 2026so i work at a pharmacy and honestly the scripts saved my life when i started. i was so nervous i’d forget something important and someone would end up in the er. but after a few months i stopped reading them word for word and started using them like a checklist in my head. like, ‘ok, what do they know? how do they take it? what’s scary?’ and then i just talk. and the teach-back thing? holy crap. one guy said he was taking his blood pressure med ‘when he felt dizzy’-like, every other day. i fixed that. no fancy tech. just asking him to repeat it back. also, typo: ‘naloxone’ not ‘naloxone’ lol
Erwin Kodiat
January 22, 2026I’ve been to pharmacies in rural India, in Nairobi, and here in Ohio. The script doesn’t matter as much as the person behind it. One pharmacist in Nairobi didn’t have a printed script-just a notebook with doodles and bullet points. But he asked, ‘Who helps you take your pills?’ and the patient started crying because her daughter was gone. That’s counseling. It’s not about the words you’re supposed to say. It’s about the silence you’re willing to hold.
Phil Hillson
January 23, 2026Look I get it you want to feel like a healer but the truth is most people dont care about your three questions they just want the pill and to get out of here. and the ‘teach back’ thing? that’s just a fancy way of making patients feel stupid. ‘Can you explain it back?’ yeah i can explain it back but i dont wanna be your lab rat. and ai scripts? next thing you know they’ll be replacing pharmacists with chatbots that say ‘have you tried not being sick?’
Jacob Hill
January 23, 2026Love the point about flexibility. I’ve seen scripts that are 12 pages long for a simple antibiotic. Meanwhile, the 78-year-old woman who just lost her husband and is on 12 meds? She needs one thing: ‘I’m here. Let’s go slow.’ The script should be a guide-not a cage. And if your EHR forces you to click ‘understood’ after 45 seconds? That’s not documentation. That’s a lie.
Jackson Doughart
January 24, 2026There is a quiet dignity in the act of asking, 'What do you know?' It is not interrogation. It is invitation. And in a system that reduces human beings to data points and compliance metrics, this small gesture-this humble inquiry-becomes radical. The script, when used with intention, is not a tool of control. It is an act of reverence. We are not dispensing pills. We are holding space for someone’s life to unfold. And that, above all, is sacred.
Malikah Rajap
January 25, 2026Wait… so if I’m a teen on birth control and I’m scared to tell my mom I’m on it… and the script says ‘do you have support at home?’… and I say ‘no’… and you just move on? What’s the point? You’re not gonna fix my life. You’re just gonna check the box. And then I’m gonna stop taking it because I’m scared and nobody asked me how I feel. You can’t script trust. You can’t script vulnerability. You can’t script the fact that I’m 17 and I don’t know how to say ‘I’m alone’ out loud. So… what now? Do I just… go home and cry?