Switching from a brand-name drug to a generic version is supposed to save money - and for most people, it does. But sometimes, your body reacts differently. You might feel off. Maybe you’re more tired than usual. Or you get a rash. Or your condition seems to be getting worse. If that happens, don’t ignore it. You might not be imagining things. There’s real science behind why some people have problems after switching to generics.
Why Do Generics Sometimes Cause Problems?
Generics are required by the FDA to contain the same active ingredient, strength, and dosage as the brand-name drug. That means the part of the pill that treats your condition - say, the serotonin reuptake inhibitor in antidepressants or the thyroid hormone in levothyroxine - is identical. So why do some people have side effects?
The answer lies in the inactive ingredients. These are the fillers, dyes, preservatives, and binders that hold the pill together or help it dissolve. While they don’t treat your illness, they can affect how your body absorbs the medicine. For most people, this doesn’t matter. But for others, especially those with allergies or sensitivities, even a tiny change in filler can trigger a reaction.
And here’s the kicker: the FDA allows generics to vary in how much of the active ingredient enters your bloodstream by up to 20%. That sounds small - but for certain drugs, it’s not. These are called narrow therapeutic index (NTID) drugs. With these, the difference between a safe dose and a dangerous one is razor-thin. A 10% change in absorption could mean your blood pressure spikes, your seizures return, or your thyroid levels go haywire.
Which Drugs Are Most Likely to Cause Issues?
Not all medications are created equal when it comes to switching. Some are rock-solid in generic form. Others? Not so much.
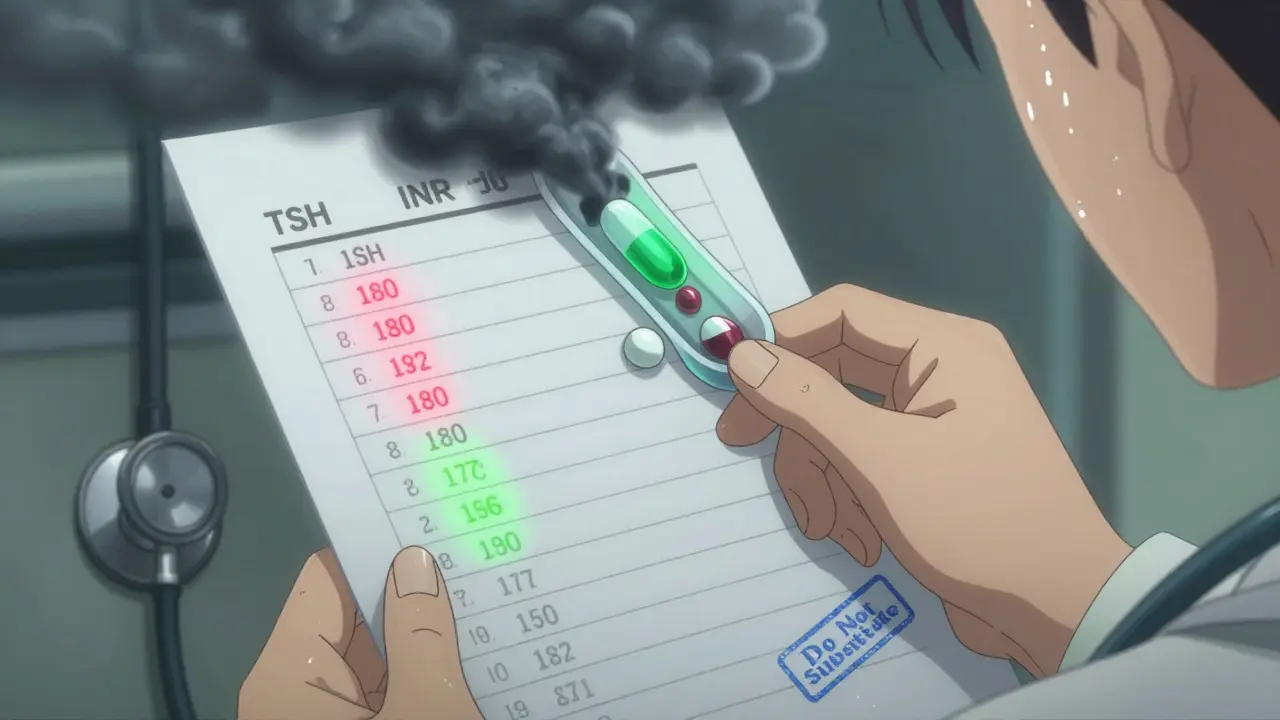
- Levothyroxine (Synthroid): Used for hypothyroidism. Studies show 15% of patients switching from brand to generic had abnormal TSH levels - meaning their thyroid wasn’t being controlled properly.
- Warfarin (Coumadin): A blood thinner. Even small changes in how much warfarin gets into your blood can raise your risk of clots or dangerous bleeding.
- Lamotrigine (Lamictal): Used for epilepsy and bipolar disorder. One study found patients switching between generic versions had a 25% higher chance of having a seizure.
- Phenytoin (Dilantin): Another seizure drug. Blood levels can swing unpredictably with different generics.
- Sertraline (Zoloft) and other SSRIs: While not NTID, many patients report mood changes, anxiety spikes, or nausea after switching. Over 37% of patient reports on Drugs.com cited side effects after switching to generic sertraline.
- Sumatriptan (Imitrex): For migraines. A documented case showed a patient’s migraines returned after switching to generic - and vanished when they went back to the brand.
For drugs like metformin (for diabetes) or atorvastatin (for cholesterol), switching is almost always safe. But if you’re on one of the drugs above - or anything else that requires precise dosing - proceed with caution.
Warning Signs You Need to Call Your Doctor
Not every weird feeling means something’s wrong. But if you notice any of these after switching to a generic, call your doctor within 24 hours:
- Skin rash, hives, or itching: This could be an allergic reaction to a dye or filler. About 14% of reported adverse events from generic switches involve skin reactions.
- Persistent nausea or vomiting: If it lasts more than a day or two, it might mean your body isn’t absorbing the drug properly.
- Unexplained fatigue or dizziness: Especially if you’re on a heart, thyroid, or seizure medication. These can be signs your drug levels are off.
- Changes in how well your medication works: Your blood pressure isn’t dropping? Your seizures are back? Your depression feels worse? Don’t assume it’s "just stress."
- Headaches, mood swings, or confusion: These are common with brain-targeting drugs like lamotrigine or sertraline. Even small bioavailability shifts can trigger them.
If you experience any of these symptoms, don’t wait. Call your doctor. Don’t stop taking the drug unless instructed - but do get advice fast.
Emergency Signs - Call 911
Some reactions need immediate care:
- Swelling of the throat or tongue: This can block your airway.
- Difficulty breathing: Wheezing, gasping, or feeling like you can’t get enough air.
- Systolic blood pressure below 90 mmHg: That’s dangerously low. You might feel faint, cold, or confused.
If you have any of these, call 911. These are signs of anaphylaxis - a life-threatening allergic reaction. It’s rare, but it can happen with a new filler or dye in a generic pill.
What to Do If You Suspect a Problem
Don’t guess. Don’t assume it’s "all in your head." Here’s what to do:
- Check your pill. Look at the packaging. Did the shape, color, or imprint change? That’s a sign you got a different generic version.
- Call your pharmacy. Ask them which manufacturer made your new generic. Some manufacturers are more consistent than others.
- Ask your doctor about testing. For drugs like warfarin, they can check your INR. For levothyroxine, they can test your TSH. For seizure meds, they can measure blood levels.
- Request your old version. In 28 states, laws require pharmacists to notify your doctor before switching NTID drugs. You have the right to ask for the brand - or the same generic you were on.
- Keep a symptom log. Write down what you feel, when it started, and how bad it is. This helps your doctor see the pattern.

What Your Doctor Can Do
Your doctor isn’t just going to say, "It’s probably fine." They can:
- Order lab tests to check drug levels or biomarkers (like TSH or INR).
- Prescribe a specific generic brand that’s known to be more consistent.
- Request a "Do Not Substitute" note on your prescription - this legally prevents the pharmacy from switching you without approval.
- Switch you back to the brand-name version if it’s medically necessary.
In fact, the American Medical Association now recommends doctors document when a brand-name drug is medically necessary. That helps prevent automatic substitutions that could put you at risk.
How to Protect Yourself Going Forward
Here’s how to avoid problems before they start:
- Ask before you switch. If you’re on a high-risk drug (like those listed above), ask your doctor: "Is it safe to switch to generic?"
- Stick with one pharmacy. Pharmacies sometimes switch generics without telling you. If you always use the same one, they’re more likely to keep you on the same version.
- Check the FDA’s Orange Book. It lists which generics are rated "A" (therapeutically equivalent) and which are "B" (potential issues). You can search it online - no login needed.
- Know your state’s laws. Some states - like California - require pharmacists to notify your prescriber before switching NTID drugs. Find out what your state requires.
- Consider pharmacogenomic testing. Companies like Color Genomics now offer tests that show how your genes affect drug metabolism. If you’re sensitive to many medications, this could help predict reactions.
The bottom line? Generics are safe for most people. But for some, even a small change can be dangerous. Your body knows when something’s off. Listen to it. And don’t be afraid to speak up.
Can I get sick from inactive ingredients in generic drugs?
Yes. While the active ingredient is the same, inactive ingredients like dyes, preservatives, or fillers can trigger allergic reactions or digestive issues. People with sensitivities to lactose, gluten, or artificial colors are especially at risk. If you notice a rash, nausea, or swelling after switching, it could be the filler - not the medicine itself.
Are all generics the same?
No. Different manufacturers use different fillers and manufacturing processes. Two generics for the same drug can behave differently in your body. One might dissolve faster, another slower. That’s why sticking with the same brand of generic - if it works for you - is often the safest choice.
Can my pharmacist switch my generic without telling me?
In most cases, yes - unless your prescription says "Do Not Substitute." But for narrow therapeutic index drugs like levothyroxine or warfarin, 28 states now require pharmacists to notify your doctor before switching. Check your state’s laws to know your rights.
I switched and feel worse. Should I go back to the brand-name drug?
Talk to your doctor first. If your symptoms started right after switching, it’s very likely the generic. Your doctor can write a new prescription for the brand or a different generic. Don’t stop taking your medication abruptly - that could be dangerous. But don’t ignore the warning signs either.
Is there a list of drugs that shouldn’t be switched to generics?
The FDA doesn’t ban any generics outright, but it does rate them. Look up your drug in the FDA’s Orange Book. Drugs with an "A" rating are considered equivalent. Those with a "B" rating may have issues. High-risk drugs include levothyroxine, warfarin, lamotrigine, phenytoin, and cyclosporine. Many doctors avoid switching these unless absolutely necessary.

10 Comments
Alex Ogle
February 10, 2026So I switched my levothyroxine to generic last year. Thought I was being smart with the cash. First week? Total zombie mode. Couldn’t get out of bed. Thought I was depressed. Then I remembered-oh right, I changed pills. Went back to the brand. Within three days, I was human again. Turns out, my body isn’t fine with random fillers. FDA says they’re the same? Yeah, right. Like saying two different brands of toilet paper are the same because they both have cellulose. One’s rough, one’s soft. One makes you cry. The other? Just sits there. Don’t trust the system. Trust your body.
Tatiana Barbosa
February 12, 2026Yesss this is so real!! I’ve been on lamotrigine for 8 years and switched generics twice. First time? Seizure scare. Second time? Mood rollercoaster for weeks. I stopped blaming myself. Started asking for the exact manufacturer-Lupin. Now I’m stable. Docs don’t always know this stuff. Pharmacies don’t tell you. You gotta be your own advocate. If you feel off after a switch? It’s not in your head. It’s in the coating. 💪
Simon Critchley
February 12, 2026Let’s be real-this whole FDA bioequivalence thing is a farce. 20% variation? That’s not bioequivalence, that’s Russian roulette. And don’t get me started on the ‘A’ and ‘B’ ratings. The Orange Book is a joke. It doesn’t account for inter-individual variability. I’ve seen pharmacists swap generics mid-script like it’s a baseball card trade. And then patients show up with elevated INRs or TSH levels? Nah. It’s not ‘patient noncompliance.’ It’s systemic negligence. The system is rigged. And we’re the lab rats.
Karianne Jackson
February 13, 2026I switched my Zoloft and started crying for no reason. Like, full sobbing in the grocery store. I thought I was going crazy. Then I read this. Changed back. Instant relief. Why do they even let us switch these? It’s like playing musical chairs with your brain. 😭
Andy Cortez
February 14, 2026ugh i swear i switched to generic warfarin and almost died. not kidding. my inr went from 2.8 to 4.9 in 3 days. i was bleeding from my gums. called my doc at 2am. he was like 'oh yeah, that one's bad'. turns out the generic had a different filler. i asked for the brand. they said 'it's too expensive'. i said 'fine, i'll pay for it myself'. now i'm alive. and mad. seriously. this is medical malpractice.
Jessica Klaar
February 14, 2026My mom’s on levothyroxine. She switched generics and started having panic attacks. We didn’t connect it at first. Then we noticed the pill looked different. Called the pharmacy. Turns out they switched from Teva to Mylan. Mom’s TSH was off by 30%. Doctor ordered her back to the original. She’s fine now. This isn’t just about money-it’s about trust. Your body knows when something’s changed. Listen. And don’t let anyone tell you you’re overreacting.
Patrick Jarillon
February 15, 2026They’re lying. All of them. The FDA, the pharmacists, the doctors. The 'inactive ingredients' are a cover. They’re using glyphosate, talc, and nano-particles to control us. Why do you think the same generic works for some and kills others? It’s not the filler-it’s the tracking chip. They want to monitor your brain chemistry. That’s why they push generics. That’s why they won’t let you know who made your pill. Wake up. The Orange Book? A distraction. The real data? Buried in a server in Virginia.
John Watts
February 15, 2026Hey everyone, if you’re reading this and you just switched meds-take a breath. You’re not alone. This stuff is scary, but you’ve got power. Ask your pharmacist for the manufacturer. Check the pill imprint. Keep a symptom journal. And if your doctor brushes you off? Find a new one. There are docs out there who get it. You deserve to feel like yourself again. You’re not crazy. You’re just paying attention. Keep going. You got this. 💙
Randy Harkins
February 17, 2026Just wanted to say thank you for this post. I’ve been on cyclosporine since my transplant, and I switched generics once. Within 48 hours, my creatinine spiked. I didn’t know why. This article explained everything. I called my transplant team, they pulled my old prescription, and now I’m on the same generic brand-Teva. My numbers are stable again. If you’re on an NTID drug: don’t wait. Act fast. Your life depends on it.
Chima Ifeanyi
February 18, 2026Let’s cut through the noise. This isn’t about generics. It’s about profit margins. Pharma companies don’t care if you get a rash-they care if you stop buying. The brand-name drug has a patent. The generic? It’s a commodity. So they optimize for cost, not consistency. They don’t test for individual sensitivity. They test for ‘average’ patients. And who are you? An outlier. A statistical noise. That’s why you feel weird. You’re not broken. The system is. And they’ll keep doing this until we force them to stop. Until then? Demand transparency. Demand accountability. Or keep getting sick.