Many people over 65 take five or more medications every day. Some of those pills might not be helping anymore-but they’re still costing you money. You might be paying $80 a month for a sleep aid you haven’t needed in years, or $120 for a supplement your doctor never even recommended. The truth is, deprescribing isn’t just about safety-it’s one of the most direct ways to cut your monthly drug bills without sacrificing your health.
What Deprescribing Really Means
Deprescribing isn’t just stopping pills. It’s a careful, step-by-step process where you and your doctor review every medication you’re taking and decide which ones you can safely stop. The goal? Remove drugs that no longer help-or that might be hurting you more than helping. This isn’t a quick fix. It’s a conversation. And it’s backed by data: a 2020 Kaiser Permanente study found that when patients stopped unnecessary medications, their drug costs dropped by $1.2 million in one year across a single health system.One of the biggest drivers behind this? Polypharmacy-taking five or more medications at once. Nearly 4 in 10 adults over 65 are in this group. And the more pills you take, the higher your risk of side effects: dizziness, falls, memory problems, kidney stress. Worse, many of these drugs are prescribed years ago for conditions that have changed-or disappeared.
Why You’re Paying for Pills You Don’t Need
Think about it: when was the last time someone sat down with you and asked, “Why are you still taking this?”Often, medications get added over time-maybe after a hospital stay, or during a flare-up of a chronic condition. Once they’re on your list, they just stay there. A 2021 study found that patients bring an average of 2.3 unnecessary medications to their doctor’s office during a simple “brown bag review,” where you dump all your pills-prescription, over-the-counter, supplements-onto the table.
Here’s a real example: a 72-year-old woman from Ohio was taking a $120/month sleep aid, a $60/month calcium supplement, and a $45/month herbal remedy for joint pain. Her doctor found out she hadn’t had trouble sleeping in over a year, her blood calcium levels were normal, and the herbal remedy interacted dangerously with her blood pressure pill. Stopping all three saved her $2,220 a year.
And it’s not just seniors. About 1 in 7 adults between 40 and 64 are taking five or more meds. If you’re on a fixed income, that’s 18% of your monthly budget going to pills that might not even be working anymore.
How to Start the Conversation
You don’t need to wait for your doctor to bring it up. Be ready. Before your next appointment:- Gather every pill, patch, capsule, and supplement you take-including vitamins, CBD, and herbal teas.
- Write down why you take each one, how long you’ve been on it, and how much it costs per month.
- Write down any side effects you’ve noticed: fatigue, confusion, stomach upset, dizziness, or muscle pain.
Then, bring these questions to your doctor:
- Why am I still taking this?
- Is this still helping me-or just adding risk?
- Could this be causing falls, memory issues, or kidney problems?
- Can I stop it? If so, how?
- Who should I call if I feel worse after stopping?
Doctors want to help. But most primary care visits last just 15 to 18 minutes. The more prepared you are, the more likely they’ll make time for this.
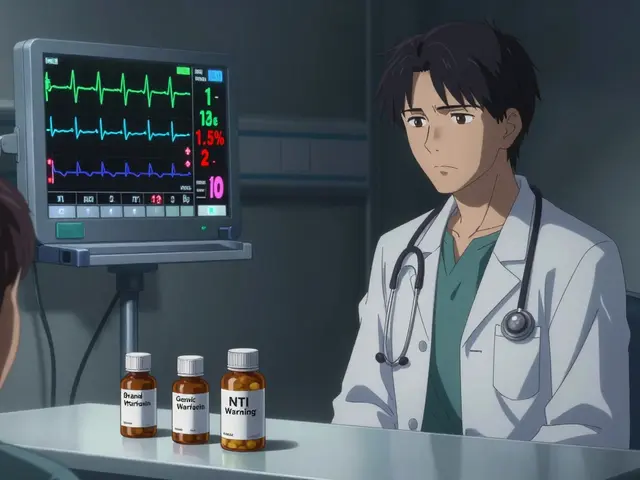
The Tools Doctors Use to Decide What to Stop
Your doctor isn’t guessing. They’re using proven tools. One of the most common is the Beers Criteria, a list of 53 medications that are risky for older adults-like certain sleeping pills, antihistamines, and muscle relaxants. If you’re on any of these, your doctor should question whether they’re still needed.Another tool is the Medication Appropriateness Index (MAI). It scores each medication on 10 factors: Is it necessary? Is the dose right? Are there interactions? Is it causing side effects? Each med takes about 7 minutes to review. That’s why it’s so important to come prepared-you’re helping them work faster.
Some clinics use AI tools like MedStopper, which scans your medication list and flags high-risk or low-benefit drugs with 89% accuracy. These tools aren’t replacing doctors-they’re helping them make better decisions faster.
How Deprescribing Actually Works
You don’t just quit cold turkey. That’s dangerous. Deprescribing is slow and monitored.For example:
- If you’re on a blood pressure pill that’s no longer needed, your doctor might reduce the dose by half for two weeks, then stop it-while checking your blood pressure at home.
- If you’re on a proton pump inhibitor (PPI) for heartburn, studies show you can stop it safely in 4 to 8 weeks with gradual tapering. You might get mild reflux at first, but it usually fades. And you’ll save $420 a year.
- For antidepressants or anti-anxiety meds, stopping too fast can cause brain zaps, insomnia, or nausea. Your doctor will create a tapering schedule-maybe reducing by 10% every two weeks.
Always stop one medication at a time. That way, if something changes, you know which pill caused it.
Where You Can Get Extra Help
You don’t have to do this alone. Your pharmacist is a hidden ally.Under Medicare Part D, most community pharmacies offer free Medication Therapy Management (MTM). A pharmacist will sit down with you, review all your meds, check for interactions, and suggest cheaper alternatives. One 2022 study found these sessions uncover an average of $1,200 in annual savings per patient.
Some health systems, like Kaiser Permanente, have full deprescribing programs. Patients in these programs report 92% satisfaction-and they save $47 per month on average.
If you’re on Medicaid or Medicare Advantage, ask if your plan covers a comprehensive medication review. Since 2023, CMS requires these for high-risk patients-and they’re free.
What Happens If You Stop Without Guidance?
Some people try to stop meds on their own. They see a high price tag and think, “I don’t need this.” But that’s risky.A 2022 survey by the National Council on Aging found that 18% of people who stopped meds without doctor help ended up in the ER or hospital. The average cost of those unexpected visits? $1,200.
One man stopped his beta-blocker because it made him tired. Two weeks later, he had chest pain and ended up in the hospital with a heart rhythm issue. He didn’t realize the pill was also controlling his arrhythmia.
Another woman stopped her statin because she thought it was “just for cholesterol.” She didn’t know it was also reducing her risk of stroke. Within six months, she had a mini-stroke. Her drug cost was $60/month. Her hospital bill? $28,000.
Deprescribing isn’t about cutting corners. It’s about cutting waste-with safety.
How Much Can You Really Save?
Let’s do the math:- One $50/month pill you no longer need = $600 saved per year.
- Three unnecessary pills = $1,800 saved.
- Avoiding one medication-related hospitalization = saves $15,700 (Medicare 2022 data).
According to the Lown Institute, inappropriate polypharmacy costs the U.S. system $30 billion a year. For you? That’s $600, $1,200, or even $2,000 back in your pocket.
And it’s not just about pills. A 2021 JAMA study found that stopping unnecessary proton pump inhibitors didn’t just save $420-it also lowered the risk of pneumonia by 25%. That’s fewer sick days, fewer doctor visits, and less stress.
What If Your Doctor Says No?
Sometimes, doctors hesitate. Maybe they’re busy. Maybe they’re worried about liability. Or maybe they don’t know how to start.If that happens, bring this up:
- “I’ve read that deprescribing is recommended by the American Geriatrics Society as one of the top five things to do for older adults.”
- “I’d like to try stopping this under your supervision-maybe over 8 weeks-with check-ins.”
- “Can we get a second opinion from a pharmacist?”
Many doctors are supportive-78% say they believe in deprescribing. But only 35% feel trained to do it well. You’re not pushing back. You’re helping them do their job better.
What Comes Next?
After you stop a medication, schedule a follow-up in 4 to 6 weeks. Check in with your pharmacist. Track how you feel. Are you sleeping better? More energy? Less dizziness? Any new symptoms?And keep doing this. Medication needs change. Your body changes. What helped at 65 might not help at 75. Make medication reviews part of your annual checkup-like blood pressure or cholesterol tests.
Deprescribing isn’t about taking less medicine. It’s about taking the right medicine. And when you do, you don’t just get healthier-you get your money back.
Is deprescribing safe?
Yes-when done properly. Deprescribing is a planned, gradual process guided by your doctor. Stopping medications suddenly can be dangerous, but with a tapering plan and monitoring, it’s one of the safest ways to reduce side effects and improve health. Studies show that when done correctly, deprescribing reduces hospital visits by 28% and lowers the risk of falls and confusion.
Can I stop my meds on my own if they’re expensive?
No. Stopping medications without medical supervision can cause serious problems-like rebound high blood pressure, seizures, anxiety, or heart rhythm issues. Even supplements and over-the-counter pills can interact dangerously. If cost is the issue, ask your doctor or pharmacist for alternatives, generic versions, or patient assistance programs. Never stop cold turkey.
How often should I review my medications?
At least once a year. If you’re on high-risk medications-like blood thinners, sedatives, or diabetes drugs-review them every 6 months. After any hospital stay, surgery, or major health change, schedule a full medication review. Your needs change as you age, and so should your pills.
Do I need to tell my specialist if I stop a medication?
Yes. If you’re seeing multiple doctors, make sure all of them know what you’ve stopped. A pill your cardiologist prescribed might be helping your migraines too. If your primary care doctor stops it without telling your neurologist, you could end up with new symptoms. Keep a shared list-digital or paper-and share updates with every provider.
Does Medicare cover medication reviews?
Yes. Medicare Part D requires pharmacies to offer free Medication Therapy Management (MTM) to high-risk beneficiaries. You can also get a comprehensive medication review as part of your Annual Wellness Visit under Medicare Part B. Ask your pharmacist or doctor if you qualify. These services are free and can save you hundreds or even thousands of dollars a year.
Are there apps or tools to help track my meds?
Yes. Apps like Medisafe, MyTherapy, and MyTherapy allow you to log all your pills, set reminders, and share your list with your doctor. Some pharmacies offer free digital tools through their patient portals. You can also use a simple spreadsheet with columns for name, dose, reason, cost, and start date. The key is having a clear, updated list you can show at every appointment.



10 Comments
Wesley Pereira
January 6, 2026So let me get this straight-we’re paying $120/mo for a sleep aid we haven’t needed since 2019? And the doc just lets it ride? Welcome to American healthcare, where the algorithm prioritizes billing over brain function. I’ve got three meds on my list that were prescribed during a panic attack in 2017. I haven’t had a panic attack since 2018. Still paying. Still taking. Still wondering why my liver hates me.
Rachel Wermager
January 8, 2026Actually, the Beers Criteria was updated in 2023 to include GABAergics with half-lives >24h in patients with CKD stage 3+, and many clinicians still use outdated versions. The MAI scoring system also doesn’t account for polypharmacy-induced cognitive load, which correlates with non-adherence in >62% of geriatric patients per JAMA Intern Med 2021. You need to cross-reference with STOPP/START v2 and the PRISCUS list if you’re in a VA system. Otherwise you’re just guessing.
Leonard Shit
January 9, 2026My grandma stopped her statin because it made her legs ache. Two months later she got a stroke. Turned out the statin wasn’t just for cholesterol-it was keeping her plaque from turning into a brick in her carotid. She didn’t know that. Neither did her cardiologist. Point is: don’t be the guy who thinks ‘expensive = useless.’ Sometimes the pill you hate is the one keeping you alive. Talk to your pharmacist first. They’re the real heroes in white coats.
Gabrielle Panchev
January 11, 2026Okay, but have you considered that deprescribing without a structured tapering protocol, especially for benzodiazepines or SSRIs, can induce rebound anxiety, insomnia, or even serotonin discontinuation syndrome-which presents with electric shock sensations, vertigo, and gastrointestinal distress, sometimes lasting weeks? And if you’re on multiple CNS-active drugs, the withdrawal interactions are not trivial, and many primary care providers aren’t trained to manage them-hence the 18% ER visit rate you cited. This isn’t just ‘cutting waste’-it’s pharmacological triage, and if you’re not monitoring labs, ECGs, and cognitive function during the process, you’re gambling with your neurological integrity.
Dana Termini
January 11, 2026I did this last year. Stopped three things: a sleep pill I didn’t need, a calcium supplement my bloodwork showed was fine, and a ‘joint support’ herb that was making my stomach burn. Saved $1,800. Felt better. No crashes. No withdrawals. Just… lighter. I didn’t know how much weight those pills were putting on me-mentally and physically. My doctor was surprised I even knew to ask. Turns out, I’m not the weird one. The system is.
Matt Beck
January 13, 2026Deprescribing is the ultimate act of radical self-trust. 🤔 You’re not rejecting medicine-you’re reclaiming your body from the industrial medical complex. Every pill you stop is a quiet rebellion against the idea that you’re broken and need fixing. The real cost isn’t the $120/month supplement-it’s the decades of learned helplessness we’ve been sold. So ask the questions. Challenge the script. Your body remembers what your prescription pad forgot. 🌿✨
Molly McLane
January 14, 2026Just had my first MTM session with my pharmacist. She found I was taking two different antihistamines that canceled each other out, and a supplement that raised my blood pressure. She switched me to a $5 generic, cut my monthly med cost by 40%, and gave me a printed checklist. No judgment. No rush. Just ‘let’s make this work for you.’ If your doctor won’t do this, find a pharmacist who will. They’re the unsung heroes of safe, smart care.
Katie Schoen
January 15, 2026My mom’s on 11 meds. She’s 74. She can’t remember which ones are for what. I made her a color-coded chart. Blue = blood pressure, red = heart, green = ‘stuff I forgot why I’m taking.’ She stopped the sleep aid last month. Slept worse for two nights. Then slept like a baby. Saved $2,200. And she didn’t even realize how tired she was until it was gone. Don’t wait for a crisis. Just ask. One pill at a time.
Beth Templeton
January 15, 2026Stop the sleep aid. You don’t need it. Done.
Ryan Barr
January 16, 2026Most of these ‘savings’ are statistically insignificant when you factor in the marginal utility of polypharmacy in frail elderly populations. The Lown Institute’s data is cherry-picked. Real-world deprescribing requires geriatric pharmacology expertise, which 90% of PCPs lack. This is feel-good populism dressed as fiscal responsibility. If you’re going to stop meds, do it with a geriatrician-not a Reddit post.