What Exactly Are Cataracts?
Cataracts are a natural part of aging for most people. They happen when the clear lens inside your eye slowly becomes cloudy, like a foggy window. This clouding blocks light from reaching the retina, making everything look blurry, faded, or washed out. It’s not a film over the eye - it’s the lens itself changing. You can’t see it in the mirror, but you’ll notice it in how you see the world: colors seem dull, night driving becomes scary because of glare, and reading small print feels impossible even with glasses.
By age 80, more than half of all Americans have cataracts or have had surgery to remove them. The National Eye Institute estimates that 24.4 million people in the U.S. over 40 are affected. It’s not caused by overuse of the eyes, reading in dim light, or screen time. It’s the slow breakdown of proteins in the lens over decades. Think of it like milk turning sour - it’s a chemical change inside the eye, not an infection or injury.
How Cataract Surgery Changed Everything
For centuries, the only "treatment" was couching - poking the cloudy lens out of place with a needle. It didn’t restore vision; it just made the eye less cloudy. That changed in 1949, when British surgeon Sir Harold Ridley implanted the first artificial lens - an intraocular lens, or IOL - during cataract removal. It was revolutionary. Suddenly, you didn’t just remove the bad lens; you replaced it with a new one that could focus light again.
Today, cataract surgery is the most common surgical procedure in the United States. About 3.8 million surgeries are done every year. It’s an outpatient procedure, meaning you go home the same day. Local anesthesia numbs the eye, so you’re awake but feel no pain. The whole process takes less than 20 minutes per eye.
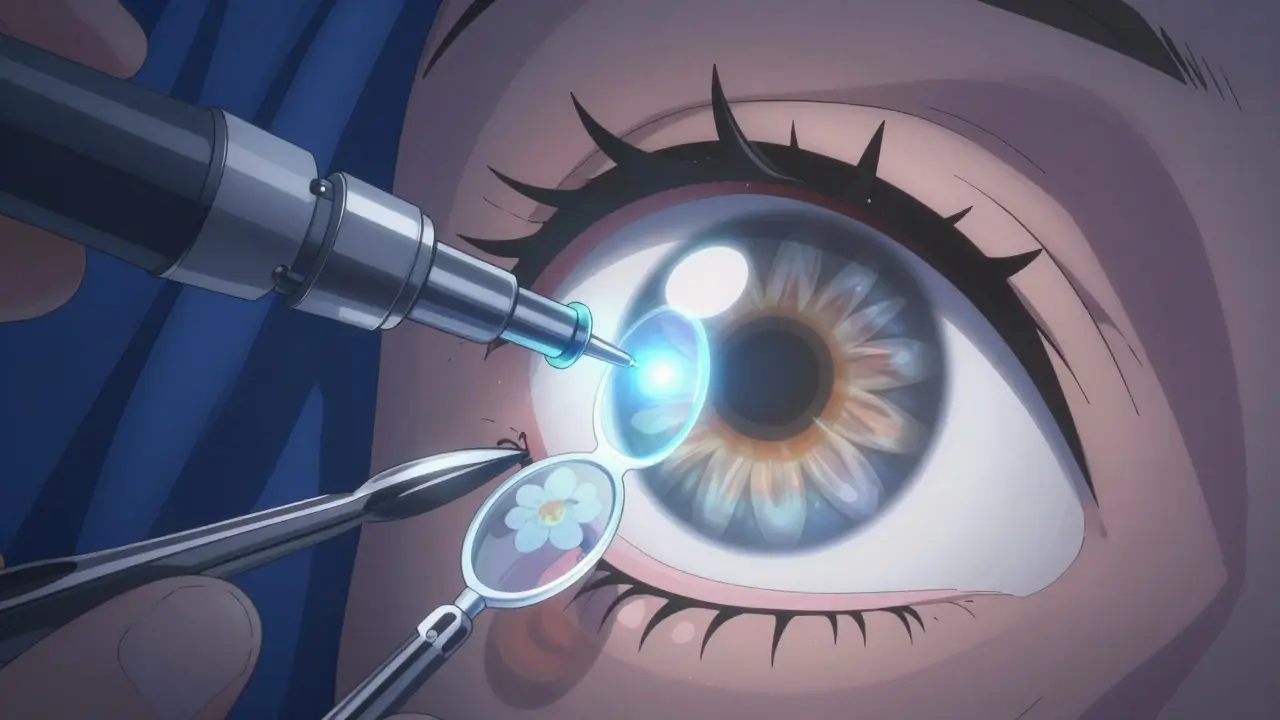
How the Surgery Works: Phacoemulsification
Nearly all modern cataract surgeries use a technique called phacoemulsification. Here’s how it works:
- A tiny incision, just 2.2 to 2.8 millimeters wide, is made in the edge of the cornea.
- A small ultrasonic probe is inserted. It vibrates at high speed to break the cloudy lens into tiny pieces.
- Those pieces are gently suctioned out.
- A foldable intraocular lens (IOL) is inserted through the same tiny opening.
- The lens unfolds inside the capsule where your natural lens used to be.
No stitches are needed because the incision is so small. It seals on its own. This is why recovery is faster and safer than ever before.
Types of Artificial Lenses (IOLs)
Not all IOLs are the same. Your choice affects whether you’ll still need glasses after surgery.
| Type | Best For | Do You Need Glasses? | Cost Range (Per Eye) |
|---|---|---|---|
| Monofocal | Distance vision (driving, TV) | Yes, for reading and close work | $1,500 - $3,000 |
| Toric | Distance vision + astigmatism | Yes, for reading | $2,500 - $4,500 |
| Multifocal | Distance, intermediate, and near | Usually no | $2,500 - $4,500 |
| Trifocal (e.g., PanOptix) | Excellent intermediate vision (computer use) | 81% don’t need glasses | $3,000 - $4,500 |
| Extended Depth of Focus (e.g., Tecnis Symfony) | Smooth vision across all distances | 89% achieve 20/25 vision or better | $3,000 - $4,500 |
Standard monofocal IOLs are often covered by Medicare and most insurance plans. But premium lenses - like toric, multifocal, or trifocal - are considered elective upgrades. They cost extra because they reduce or eliminate the need for glasses. Many patients say the extra cost is worth it.
What to Expect After Surgery
Right after surgery, your vision will likely be blurry. That’s normal. Your eye needs time to heal. You might feel a scratchy, gritty, or slightly itchy sensation. Mild discomfort is common for the first couple of days. Don’t rub your eye.
Most people notice clearer vision within 1 to 3 days. Colors look brighter - like you’re seeing in HD for the first time in years. One patient on Reddit described it as "seeing the world in color again after decades of gray."
But full recovery takes longer. While some clinics say you’re healed in 4 weeks, others say it can take up to 10 weeks. Vision can keep adjusting for months as your brain learns to interpret the new signals from the IOL. That’s why some people report strange depth perception at first - their brain has to relearn how to judge distance.
Recovery Rules: What Not to Do
Following simple rules helps avoid complications:
- Don’t drive until your doctor says it’s safe - usually after your first post-op checkup.
- Avoid water in your eye for at least a week. No swimming, showers with eyes open, or washing hair with water running over your face.
- No heavy lifting or strenuous exercise for 2-4 weeks. That includes weightlifting, gardening, or even bending over to pick up a toddler.
- Avoid eye makeup for 1-2 weeks.
- Wear the protective shield at night for the first week to prevent accidental rubbing.
Eye Drops Are Non-Negotiable
You’ll be given a strict eye drop schedule. Skipping them increases the risk of infection or inflammation. Typical drops include:
- Antibiotics (like Vigamox) - 4 times a day for 1 week to prevent infection.
- Corticosteroids (like Pred Forte) - tapered over 4 weeks to reduce swelling.
These aren’t optional. Even if your eye feels fine, keep using them exactly as prescribed.
Can You Still Need Glasses After Surgery?
Yes - and that’s okay. If you get a standard monofocal IOL, it’s designed to give you clear distance vision. You’ll still need reading glasses for phones, books, and menus. That’s by design. If you want to avoid glasses entirely, you need a premium IOL.
Even with premium lenses, some people still need occasional glasses for fine print or low-light reading. No IOL perfectly mimics the natural lens. But most patients report being far less dependent on glasses than before surgery.
When Vision Doesn’t Fully Return
Most people regain 90% of their vision after surgery. But if you had other eye conditions - like glaucoma, diabetic retinopathy, or macular degeneration - your vision may not improve as much. Surgery fixes the cataract, but it can’t fix damage from other diseases.
That’s why a full eye exam before surgery is so important. Your doctor needs to know what else might be affecting your vision.
Post-Surgery Vision Therapy
Some patients benefit from vision therapy - a set of exercises to help the brain adapt to the new lens. This isn’t for everyone, but if you feel eye strain, headaches, or trouble focusing after surgery, it can help. Exercises might include shifting focus between near and far objects, tracking moving targets, or practicing depth perception tasks.
Studies show vision therapy can reduce fatigue, improve concentration, and speed up adaptation. It’s especially useful for people with multifocal or trifocal IOLs, whose brains need time to learn how to use the different focal zones.
What Can Go Wrong?
Cataract surgery is one of the safest procedures in medicine. The success rate is over 95%. Complications occur in only 2-5% of cases.
The most common issue is posterior capsule opacification (PCO) - sometimes called a "secondary cataract." It’s not a new cataract. It’s when the membrane holding the IOL becomes cloudy. It’s easy to fix: a quick, painless laser procedure called YAG capsulotomy. It takes 5 minutes, no incisions, and vision clears within hours.
Other rare risks include infection, bleeding, or retinal detachment. These happen in less than 1% of cases. The overall safety rate for over a million procedures is 99.5%.
The Future of Cataract Surgery
Technology keeps improving. New IOLs like the Zeiss AT LISA tri 839MP, approved in early 2023, offer sharper intermediate vision - perfect for computer users. In clinical trials, accommodating IOLs that move like a natural lens are showing promise. These could one day restore full, natural focusing ability.
The global market for cataract devices is expected to hit $6.32 billion by 2027. Aging populations and demand for glasses-free vision are driving innovation.
Is Surgery Right for You?
You don’t need to wait until you’re "blind" to have surgery. If cataracts are interfering with your daily life - driving at night, reading, hobbies, or even recognizing faces - it’s time to talk to an eye doctor.
There’s no rush. Cataracts develop slowly. But delaying surgery doesn’t make the procedure harder. It just means you’re living with poor vision longer than you need to.
Most patients say they wish they’d done it sooner. One common refrain: "I didn’t realize how much I’d been missing."
Can cataracts come back after surgery?
No, cataracts cannot return because the natural lens is removed. But a cloudy membrane can form behind the new lens, called posterior capsule opacification (PCO). This feels like a cataract coming back, but it’s easily fixed with a quick laser treatment that takes minutes and has no downtime.
How long does it take to recover from cataract surgery?
Most people notice better vision within 1 to 3 days. Full healing takes 4 to 10 weeks, depending on the individual. Your vision may keep improving for months as your brain adapts to the new lens. Avoid heavy lifting and water in the eye for at least a week.
Will I still need glasses after cataract surgery?
It depends on the type of lens you choose. Standard monofocal lenses correct distance vision, so you’ll still need reading glasses. Premium lenses like multifocal, trifocal, or toric IOLs can reduce or eliminate the need for glasses. Talk to your surgeon about your lifestyle - if you read a lot or use a computer, a premium lens may be worth the extra cost.
Is cataract surgery covered by insurance?
Basic cataract surgery with a standard monofocal IOL is typically covered by Medicare and most private insurance. Premium lenses - like toric or multifocal - are considered elective upgrades and are not covered. You’ll pay out-of-pocket for those, usually between $2,500 and $4,500 per eye.
Can cataract surgery fix astigmatism?
Yes. A toric IOL is specially designed to correct astigmatism during cataract surgery. It replaces the need for glasses to correct distance vision if you have astigmatism. This is different from standard lenses and requires precise measurements before surgery. Not all surgeons offer this, so ask if it’s an option for you.
Are there non-surgical treatments for cataracts?
No. There are no eye drops, pills, or exercises that can reverse or cure cataracts. The only proven treatment is surgical removal of the cloudy lens and replacement with an artificial lens. Delaying surgery won’t make the cataract worse in a way that makes surgery riskier - it just means you’re living with blurry vision longer.
What’s the success rate of cataract surgery?
Over 95% of patients report significant improvement in vision after surgery. Patient satisfaction rates are around 98%. Complications are rare, occurring in only 2-5% of cases. The procedure has a 99.5% safety rate based on data from over a million surgeries.






11 Comments
Brian Furnell
December 21, 2025Phacoemulsification is a marvel of microsurgical engineering-2.2mm incision, ultrasonic fragmentation, foldable IOL deployment… it’s like nanotech for the cornea. The real breakthrough isn’t just removing the cataract-it’s the precision of posterior capsule retention. No sutures, minimal astigmatism induction, and sub-20-minute procedural time? That’s not medicine; it’s surgical poetry.
Siobhan K.
December 21, 2025So let me get this straight-you’re telling me I paid $4,000 for a lens that lets me see my phone without reading glasses, but I still can’t read the microwave clock without squinting? Classic.
Theo Newbold
December 23, 202595% success rate? That’s statistically significant, sure-but when your 95% is someone else’s 100% failure, you start questioning the metrics. Who’s tracking the long-term chromatic aberration from multifocal IOLs? The industry’s selling a dream, not a guarantee.
Dan Adkins
December 25, 2025It is of paramount importance to note that the pathophysiology of cataractogenesis involves the denaturation of crystalline proteins, a process which is inexorably linked to oxidative stress and advanced glycation end-products. The surgical intervention, while efficacious, does not address the systemic etiology, and thus, one must consider holistic nutritional supplementation as a coadjutant therapy.
Cameron Hoover
December 26, 2025I had the surgery last year. The first time I saw my granddaughter’s face without blur? I cried in the waiting room. Like, full-on ugly crying. I didn’t know colors could be this… alive. I still get teary when I look at my garden. It’s not just vision-it’s joy restored.
Sarah Williams
December 27, 2025Don’t skip the drops. Seriously. I did. Got a nasty inflammation. Two weeks of steroid hell. Worth every penny to avoid that mess.
Michael Ochieng
December 28, 2025In Nigeria, access to this is still a luxury. Many rely on traditional healers or wait until they’re nearly blind. It’s heartbreaking. This tech exists-and it’s life-changing. We need global equity in ophthalmic care, not just premium upgrades for the wealthy.
Meina Taiwo
December 29, 2025PCO is common. YAG laser fixes it in 5 minutes. No big deal.
Southern NH Pagan Pride
December 31, 2025They’re putting microchips in your eye, you know. The IOLs are linked to the CDC’s vision tracking network. That’s why they say it’s ‘safe’-they’re monitoring your pupils for behavioral patterns. Don’t fall for the ‘HD vision’ lie. It’s surveillance with a side of cataracts.
John Hay
January 1, 2026My mom had this done. She said the world looked like someone turned up the brightness. She’s 78. Now she reads the newspaper without her glasses. Best thing she ever did.
Jon Paramore
January 2, 2026For patients with pre-existing macular degeneration, cataract surgery won’t improve acuity beyond the retinal damage threshold. Always perform OCT and visual field testing pre-op. The IOL is a lens, not a retinal repair tool. Manage expectations-otherwise, you’re setting up a malpractice case.