Blood Pressure Medication Decision Guide
Find Your Best Blood Pressure Medication Match
Answer a few questions to get personalized recommendations for blood pressure medications based on your health profile and priorities.
Quick Takeaways
- Zestoretic combines an ACE inhibitor (lisinopril) with a thiazide diuretic (hydrochlorothiazide) to lower blood pressure in one pill.
- Alternatives fall into four groups: ACE inhibitors, ARBs, calcium‑channel blockers, and diuretics used alone or in other combos.
- Switching depends on kidney function, electrolyte balance, cost and how many pills you want to pop each day.
- Most people tolerate Zestoretic well, but cough, low potassium or high blood sugar can be deal‑breakers.
- Use the comparison table below to match your health profile with the drug class that fits best.
Ever looked at a prescription bottle and wondered if there’s a better option out there? If you’ve been prescribed Zestoretic (a combo of lisinopril and hydrochlorothiazide) you’re not alone. Many patients ask whether a single‑pill combo is the smartest move or if a different drug or combo might give fewer side effects, lower cost, or a better fit for their health history. This guide breaks down Zestoretic, explains how it works, and lines it up side‑by‑side with the most common alternatives.
What is Zestoretic?
Zestoretic is a fixed‑dose combination tablet that pairs lisinopril, an ACE inhibitor, with hydrochlorothiazide, a thiazide diuretic. It was approved by the FDA in 2011 and is marketed for adults with hypertension who need both blood‑pressure‑lowering mechanisms.
How Zestoretic Works
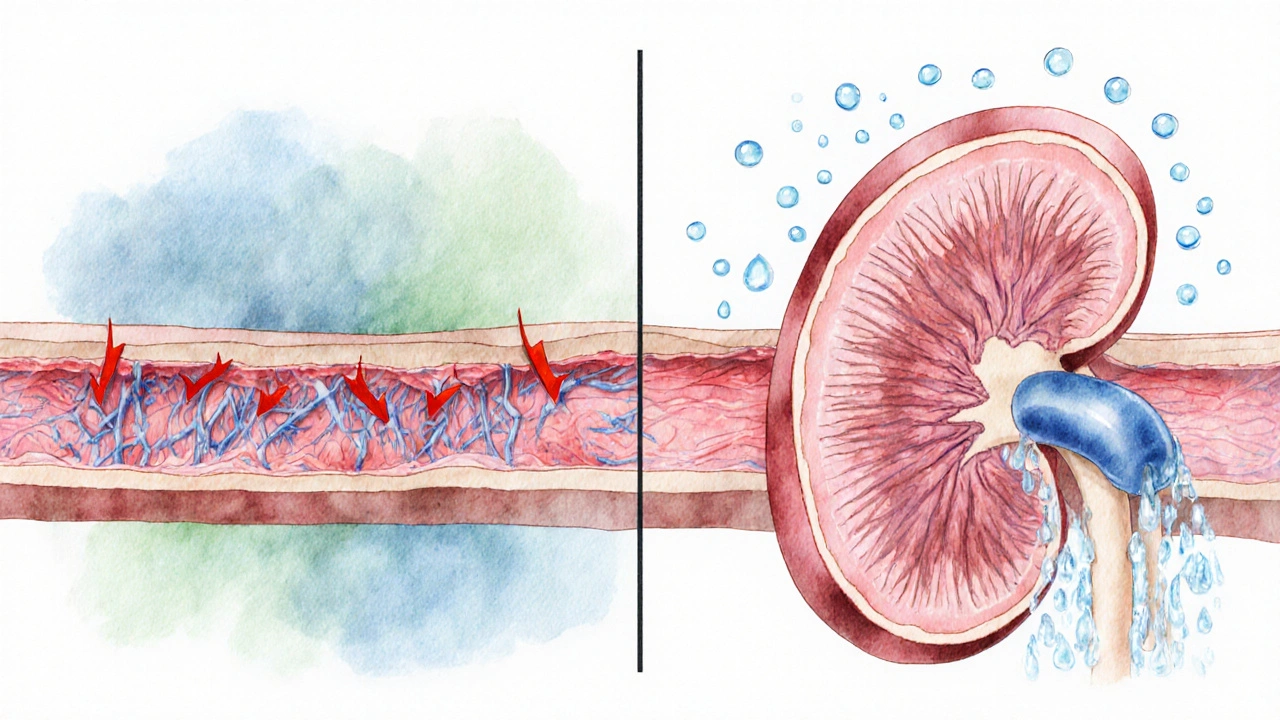
Lisinopril blocks the conversion of angiotensin I to angiotensin II, a hormone that narrows blood vessels. By lowering angiotensin II levels, blood vessels relax and pressure drops. Hydrochlorothiazide increases the excretion of sodium and water, reducing blood‑volume pressure. Together they tackle two pathways that raise blood pressure, often achieving target numbers faster than either drug alone.
Typical Uses and Dosing
- First‑line treatment for stage1 or stage2 hypertension when a single agent isn’t enough.
- Common starting strengths: 10mg lisinopril/12.5mg hydrochlorothiazide or 20mg/12.5mg.
- Take once daily, preferably in the morning with or without food.
- Doctor may adjust dose every 2-4 weeks based on blood‑pressure readings.
Common Side Effects and Warnings
Because Zestoretic mixes two drugs, you inherit side effects from both.
- Lisinopril can cause a dry cough, elevated potassium, or rare angio‑edema.
- Hydrochlorothiazide may lead to low potassium, low magnesium, higher blood sugar, or gout flare‑ups.
- Both agents can lower blood pressure too much, causing dizziness or light‑headedness, especially when you stand up quickly.
- People with severe kidney disease, pregnancy or a history of angio‑edema should avoid this combo.
Alternatives to Zestoretic
If you’re wondering about other options, they generally fall into four categories. Below is a quick snapshot of each, followed by a detailed comparison table.
- Losartan - an angiotensinII receptor blocker (ARB) that works like an ACE inhibitor but usually doesn’t cause a cough.
- Amlodipine - a calcium‑channel blocker that relaxes the smooth muscle in blood‑vessel walls.
- Benazepril - another ACE inhibitor, often paired with a separate diuretic if needed.
- Hydrochlorothiazide alone - the same thiazide diuretic used without an ACE inhibitor.
- Chlorthalidone - a thiazide‑like diuretic considered more potent than hydrochlorothiazide.
- Furosemide - a loop diuretic used for resistant hypertension or fluid overload.
- Spironolactone - a potassium‑sparing diuretic that can also improve outcomes in resistant hypertension.
Side‑by‑Side Comparison
| Drug (or combo) | Drug class | Typical dose range | Key benefit | Common drawback |
|---|---|---|---|---|
| Zestoretic | ACE‑inhibitor + thiazide diuretic | 10/12.5mg - 40/25mg once daily | One pill covers two mechanisms, good for pill‑burden reduction | Cough (ACE), electrolyte shifts (thiazide) |
| Losartan | ARB | 25mg - 100mg once daily | Rare cough, works well in patients with ACE‑inhibitor intolerance | May raise potassium, less potent alone for high BP |
| Amlodipine | Calcium‑channel blocker | 2.5mg - 10mg once daily | Effective for isolated systolic hypertension, minimal metabolic effects | Can cause ankle swelling, may interact with CYP3A4 inhibitors |
| Benazepril | ACE‑inhibitor | 5mg - 40mg once daily | Similar efficacy to lisinopril, flexible dosing | Same cough risk as other ACE inhibitors |
| Hydrochlorothiazide alone | Thiazide diuretic | 12.5mg - 50mg once daily | Low cost, well‑studied | May need separate ACE/ARB for full control |
| Chlorthalidone | Thiazide‑like diuretic | 12.5mg - 25mg once daily | Longer half‑life, often more effective than HCTZ | Higher risk of low potassium, may raise glucose |
| Furosemide | Loop diuretic | 20mg - 80mg once or twice daily | Powerful diuresis useful in volume‑overload states | Can cause ototoxicity, rapid electrolyte loss |
| Spironolactone | Potassium‑sparing diuretic | 25mg - 100mg once daily | Effective in resistant hypertension, lowers aldosterone | May cause gynecomastia, hyperkalemia |
Decision Criteria: How to Pick the Right Option
Not every drug works the same for everyone. Use these questions as a quick filter.
- Do you have a bothersome cough? If yes, an ARB like Losartan or a calcium‑channel blocker may be better.
- Is potassium a concern? Loop diuretics and potassium‑sparing agents need close monitoring.
- Do you need a low‑pill regimen? Zestoretic or a single‑pill combo (e.g., lisinopril+chlorthalidone) keep the count down.
- What’s your budget or insurance coverage? Older generics such as hydrochlorothiazide or amlodipine are often cheaper.
- Any history of kidney disease? ACE inhibitors/ARBs can protect kidneys, but dosing may need adjustment.

Practical Checklist Before Switching
- Confirm your latest blood‑pressure readings (average of three separate days).
- Review labs: serum potassium, creatinine, fasting glucose.
- List current meds to spot drug‑interaction red flags.
- Discuss lifestyle factors - salt intake, exercise, alcohol.
- Set a follow‑up appointment within 2-4 weeks after any change.
Frequently Asked Questions
FAQ
Can I split Zestoretic tablets?
The tablet isn’t scored, so splitting can give uneven doses. If you need a lower dose, ask your doctor for a different strength or a separate lisinopril plus a lower‑dose thiazide.
Is Zestoretic safe during pregnancy?
No. ACE inhibitors and thiazide diuretics are classified as pregnancy‑category D. They can affect fetal kidney development and cause low amniotic fluid. Switch to a pregnancy‑compatible antihypertensive before conceiving.
How quickly should I see a blood‑pressure drop?
Most patients notice a modest reduction within 1-2 weeks. Full effect may take 4-6 weeks as the body adjusts. Keep a log and report any persistent high readings.
Can Zestoretic be used for heart failure?
Yes, the ACE inhibitor component helps improve heart‑failure outcomes, but the thiazide part is usually omitted unless fluid overload is present. Doctors often prescribe lisinopril alone for heart failure.
What should I do if I develop a dry cough?
A dry cough is a classic ACE‑inhibitor side effect. Talk to your prescriber - they may swap lisinopril for an ARB like Losartan, which usually eliminates the cough.
Next Steps
If you’re already on Zestoretic and feeling fine, keep taking it as prescribed and schedule routine labs. If side effects nag you, bring the checklist to your next appointment and explore the alternatives that line up with your health goals. Remember, hypertension is a marathon, not a sprint - the best drug is the one you can stick with safely.






13 Comments
Sean Kemmis
October 14, 2025Zestoretic sounds like a marketing gimmick wrapped in a pill. It pretends to solve everything but ignores the fact that ACE inhibitors bring cough and thiazides drag electrolytes. If you care about real health you should read the fine print.
Nathan Squire
October 21, 2025While Zestoretic does combine two proven mechanisms, the choice really hinges on your individual tolerance profile. For patients plagued by a dry cough, switching to an ARB like losartan eliminates that nuisance. Conversely, if potassium retention is a concern, a thiazide‑only regimen may be safer, provided you monitor electrolytes. Remember that the fixed‑dose format limits flexibility; you cannot titrate the ACE inhibitor and diuretic independently. If cost is a priority, generic lisinopril and hydrochlorothiazide separately are often cheaper than the combo pill.
In short, the combo is convenient but not universally superior – a nuanced decision, not a one‑size‑fits‑all.
satish kumar
October 28, 2025It is worth noting, dear readers, that the prevalence of adverse events associated with fixed‑dose combinations, such as Zestoretic, may be underappreciated, particularly when clinicians rely heavily on pharmaceutical marketing narratives, which, as we all know, have a penchant for highlighting efficacy while downplaying the nuanced trade‑offs.
First, the inevitability of a cough arising from the lisinopril component cannot be dismissed merely as a minor inconvenience; it frequently leads to non‑adherence, thereby compromising blood pressure control.
Second, the thiazide portion introduces the specter of electrolyte disturbances, notably hypokalemia and hyperglycemia, which may exacerbate comorbid conditions in patients with diabetes or metabolic syndrome.
Moreover, the rigid dosing ratios inherent in a single‑pill formulation preclude the fine‑tuning of each agent to the individual’s pharmacodynamic response, a limitation that is especially consequential in patients with fluctuating renal function or variable volume status.
Third, from a pharmacoeconomic perspective, while the convenience factor may appear appealing, the long‑term cost burden of a brand‑name combination often exceeds that of generic constituent components, particularly in health systems where formulary negotiations favor the latter.
Fourth, the regulatory framework governing combination antihypertensives does not necessarily guarantee superior cardiovascular outcomes compared with monotherapy titrated to optimal doses, a point that has been raised in several meta‑analyses, albeit with heterogeneous study designs.
Fifth, the potential for drug‑drug interactions, especially when patients are already on multiple agents for comorbidities such as dyslipidemia or heart failure, warrants meticulous review, because the additive antihypertensive effect may precipitate orthostatic hypotension.
Sixth, clinicians must remain vigilant for rare but serious adverse events, such as angioedema, which, although uncommon, can be life‑threatening and may be more readily attributed to the ACE inhibitor component when embedded within a combination pill.
Seventh, patient education is paramount; individuals should be counseled on signs of electrolyte imbalance and instructed to report persistent cough promptly.
Eighth, the evolving landscape of hypertension guidelines continues to emphasize individualized therapy, underscoring that a fixed‑dose strategy is but one tool among many.
Ninth, for patients with a robust desire to minimize pill burden, a single‑pill regimen may indeed be advantageous, yet this should never supersede the principle of therapeutic precision.
Tenth, in practice, many clinicians adopt a stepwise approach, initiating monotherapy and only progressing to combinations when monotherapy fails to achieve target pressures.
Eleventh, the decision matrix must incorporate patient preferences, comorbid conditions, renal function, and cost considerations, thereby rendering any blanket endorsement of Zestoretic scientifically untenable.
Twelfth, ultimately, shared decision‑making remains the cornerstone of hypertension management, ensuring that each therapeutic choice aligns with the patient’s values and clinical reality.
Kimberly Dierkhising
November 4, 2025From a pragmatic standpoint, the pharmacokinetic synergy between lisinopril and hydrochlorothiazide in Zestoretic can streamline adherence, especially in patients juggling polypharmacy. However, when you factor in the renin‑angiotensin‑aldosterone system modulation alongside natriuretic effects, the therapeutic window narrows for individuals with borderline electrolyte homeostasis. In such cases, consider leveraging the drug‑drug interaction profile to your advantage: the ACE‑inhibitor component attenuates aldosterone‑mediated sodium retention, while the thiazide promotes natriuresis, together achieving a balanced hemodynamic impact. Still, monitor serum potassium and fasting glucose regularly to preempt dysregulation. For clinicians comfortable with dose titration, separating the agents provides granular control, but the fixed‑dose convenience of Zestoretic remains a compelling option for many.
Rich Martin
November 11, 2025Let’s cut through the fluff and get to the heart of the matter: Zestoretic is a clever little package that can be a boon for some, a bane for others.
We start with the undeniable advantage – one pill, two mechanisms. That’s a win in the adherence department, especially for folks who already have a mountain of daily meds.
But here’s where the devil hides: the ACE‑inhibitor cough isn’t just an annoyance; it’s the leading cause of premature discontinuation, and that can throw a wrench in your blood‑pressure goals.
On top of that, the thiazide component, while cost‑effective, can deplete potassium and magnesium, nudging patients toward metabolic disturbances that may exacerbate diabetes or trigger gout.
Now, if you have a healthy kidney and normal electrolytes, the combo can glide you into target numbers with minimal fuss.
Conversely, in a patient with borderline renal function, the ACE‑inhibitor part demands vigilant creatinine monitoring, and the thiazide can magnify any underlying hypovolemia.
The cost argument is double‑edged. While the branded combo may sit at a premium, the separate generics often undercut it by a substantial margin, especially when insurance formularies favor monotherapy.
Don’t forget drug interactions: calcium channel blockers, NSAIDs, and certain antibiotics can blunt the efficacy or heighten side‑effects, so a thorough medication reconciliation is non‑negotiable.
In the end, the decision boils down to three pillars: tolerance, economics, and the need for simplicity.
If you can tolerate a cough, have stable electrolytes, and the price is acceptable, Zestoretic delivers on its promise.
If any of those pillars wobble, explore alternatives like an ARB‐only regimen or a separate lisinopril plus a low‑dose thiazide.
Remember, hypertension is a marathon, not a sprint; the best regimen is the one you can stick with for the long haul.
Buddy Sloan
November 18, 2025Hang in there, everyone! 😊 If Zestoretic’s side effects are bugging you, talk to your doc about switching to an ARB – it often kicks the cough to the curb. Keep tracking your BP and electrolytes, and you’ll find the right balance. 🙌
Deidra Moran
November 25, 2025It’s astonishing how the mainstream medical establishment pushes combination pills like Zestoretic, effectively blurring the line between transparent care and corporate control. The hidden agenda is clear: maximize profit while compromising personalized therapy. Do you really trust a one‑size‑fits‑all solution when covert data sharing with pharma conglomerates is the norm? The reality is that patient autonomy is being eroded under the guise of convenience, and the next step will be algorithmic prescribing without consent.
Zuber Zuberkhan
December 2, 2025Optimism is key when navigating hypertension treatment, and Zestoretic offers a pragmatic pathway for many. By consolidating an ACE inhibitor with a thiazide, you reduce the psychological barrier of taking multiple pills, which can boost adherence. Yet, maintain vigilance: monitor potassium, watch for cough, and keep an eye on renal markers. If any red flags emerge, don’t hesitate to adjust the regimen – the flexibility to switch to an ARB or separate components ensures you’re not locked into a suboptimal plan. Stay proactive, stay hopeful, and remember that achieving target blood pressure is a journey powered by informed choices and collaborative care.
Tara Newen
December 9, 2025Zestoretic is just another American drug‑industry cash cow.
Amanda Devik
December 16, 2025Embrace the journey! Zestoretic can be a powerful ally when used wisely – one pill, dual action, streamlined routine. But keep a close watch on electrolytes, and don’t let a harmless‑looking cough become a roadblock. With diligent monitoring and open dialogue with your provider, you’ll navigate the maze of hypertension with confidence. 🌟
Jessica Forsen
December 22, 2025Sure, Zestoretic is convenient, but let’s not pretend it’s a miracle cure. It’s a tool, not a silver bullet.
NIck Brown
December 29, 2025Honestly, anyone still using Zestoretic without a thorough risk‑benefit analysis is ignoring basic clinical principles. Evaluate labs, assess side‑effects, and consider generics before settling on a branded combo.
Andy McCullough
January 5, 2026What about the impact of Zestoretic on nocturnal blood pressure patterns?