Antibiotic Comparison: How to Pick the Right Medication
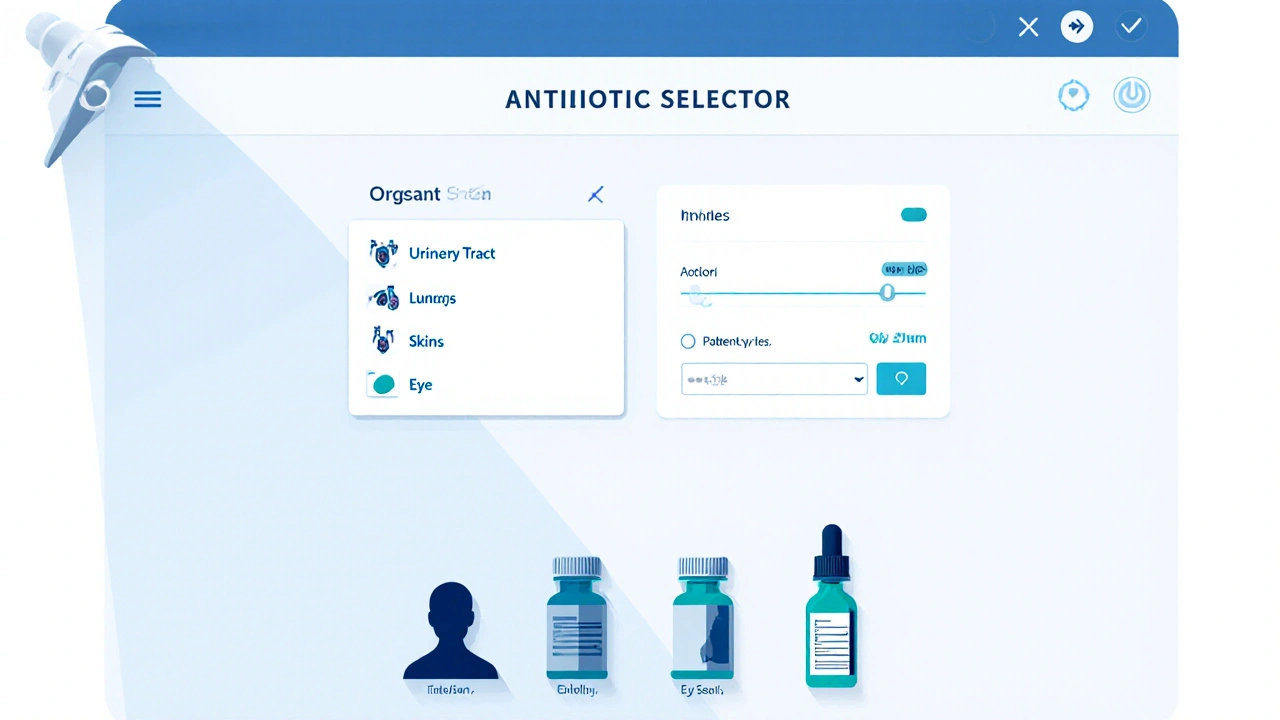
When working with antibiotic comparison, the process of evaluating and contrasting different antibiotics based on spectrum, safety, cost, and resistance risk. Also known as antibiotic selection, it helps patients and clinicians decide which drug will work best. Key players in this space include Clindamycin, a lincosamide used for skin and bone infections, Chloramphenicol, a broad‑spectrum agent with rare blood‑disorder side effects, and Tinidazole, an anti‑protozoal that also covers certain anaerobic bacteria. Understanding generic drug pricing, how identical formulations can vary in cost across pharmacies rounds out the comparison.
First, look at the antibiotic’s spectrum. Some drugs hit a wide range of bacteria (broad‑spectrum), while others target a specific group (narrow‑spectrum). Broad agents are handy when you’re not sure what’s causing the infection, but they also push resistance faster. Narrow choices, like Clindamycin for certain gram‑positive infections, spare the good microbes and keep future options open.
Second, weigh safety and side‑effects. Chloramphenicol, for example, can cause a serious blood disorder called aplastic anemia, so doctors reserve it for severe cases where alternatives fail. Tinidazole may upset the gut, so pairing it with probiotics can protect your microbiome. Knowing these risks lets you match a drug to the patient’s health profile.
Third, factor in resistance patterns. Local labs often publish which bacteria are becoming resistant to which drugs. If a community shows high resistance to a particular antibiotic, choosing another—like swapping a penicillin for Clindamycin—can improve outcomes. This step requires staying up‑to‑date with regional antibiograms.
Finally, compare costs. Generic versions of the same drug can differ dramatically between online pharmacies, big‑box stores, and local pharmacies. A 500 mg tablet of generic Clindamycin might cost $0.10 at one outlet and $0.30 at another. Adding a generic drug pricing check to your comparison saves money without sacrificing quality.
Why a Structured Antibiotic Comparison Matters
A systematic comparison saves time, reduces trial‑and‑error prescribing, and lowers the chance of adverse reactions. It also supports antimicrobial stewardship—using the right drug at the right dose for the right duration—helping keep resistance in check for everybody.
When you combine spectrum analysis, safety data, resistance trends, and price checks, you create a clear decision tree. That tree guides you from “I need an antibiotic” to “Clindamycin 300 mg twice daily for seven days is the safest, most effective, and affordable option for this skin infection.”
Below you’ll discover a curated set of articles that dive deeper into specific antibiotic comparisons, cost‑saving tips, safety guides, and real‑world case studies. Each piece adds a layer of detail to the framework outlined here, helping you make informed, confident choices for every infection scenario.
Baycip (Ciprofloxacin) vs Alternatives: Comprehensive Comparison Guide
A detailed guide comparing Baycip (ciprofloxacin) with common antibiotic alternatives, covering effectiveness, side effects, suitability, and a decision checklist.
Continue Reading



