When your child has a rash, eczema flare-up, or minor burn, it’s natural to reach for a cream or ointment to soothe the skin. But what seems like a simple fix can become dangerous if you don’t know the rules. Topical medications for kids aren’t just smaller versions of adult products-they work differently, absorb faster, and carry risks most parents never expect.
Children’s skin is thinner, more porous, and has a higher surface-area-to-body-weight ratio than adults’. This means a cream applied to a small patch of skin can be absorbed into the bloodstream at rates 3 to 5 times higher than in adults. For babies under one year, that number can jump to 10 times higher. A pea-sized amount of hydrocortisone on a toddler’s face isn’t harmless-it can suppress their stress hormone system just like taking oral steroids. And that’s just one of many hidden dangers.
Why Kids Are More Vulnerable
Think of a child’s skin like a sieve. Their outer layer, the stratum corneum, hasn’t fully developed. That’s why a lotion meant to treat diaper rash can end up entering the bloodstream, especially if the skin is cracked or inflamed. Inflamed skin, like in eczema, can absorb medications up to 15 times more than healthy skin. This isn’t theoretical-it’s why babies have had seizures from too much lidocaine cream, or developed blue lips from benzocaine teething gel.
The U.S. Food and Drug Administration (FDA) banned benzocaine products for children under two after over 400 cases of methemoglobinemia were reported since 2006. This condition stops blood from carrying oxygen properly. Symptoms come on fast-pale, gray, or blue skin, trouble breathing, dizziness. In infants, it can happen within minutes. There’s no safe dose for toddlers. Even a small dab on the gums can be life-threatening.
Topical Corticosteroids: The Most Common Mistake
Topical corticosteroids are the most prescribed skin treatments for children. But they’re also the most misused. Parents often think stronger means better. It doesn’t. A class I steroid like clobetasol is 100 times more potent than a class VII steroid like hydrocortisone 1%. Using the wrong one can cause serious side effects.
A 2022 review of 12,350 children showed that 15.8% of those using high-potency steroids developed HPA axis suppression-meaning their body stopped making its own cortisol. That’s the same hormone your body releases when you’re stressed. Without it, kids can crash during illness, infection, or even minor trauma. One study found that applying a thick layer of hydrocortisone to just 20% of an infant’s body was as risky as giving them oral prednisone at 2mg per kilogram per day.
The rule? Use the lowest strength that works. For mild eczema, hydrocortisone 0.5% or 1% is enough. For severe cases, a doctor might prescribe a mid-potency steroid like triamcinolone-but only for short bursts, usually no longer than two weeks. Never use potent steroids on the face, groin, or armpits unless directed. And never use them daily for months. The skin thins. Stretch marks appear. Blood vessels become visible. These aren’t rare side effects-they’re common when parents don’t know the limits.
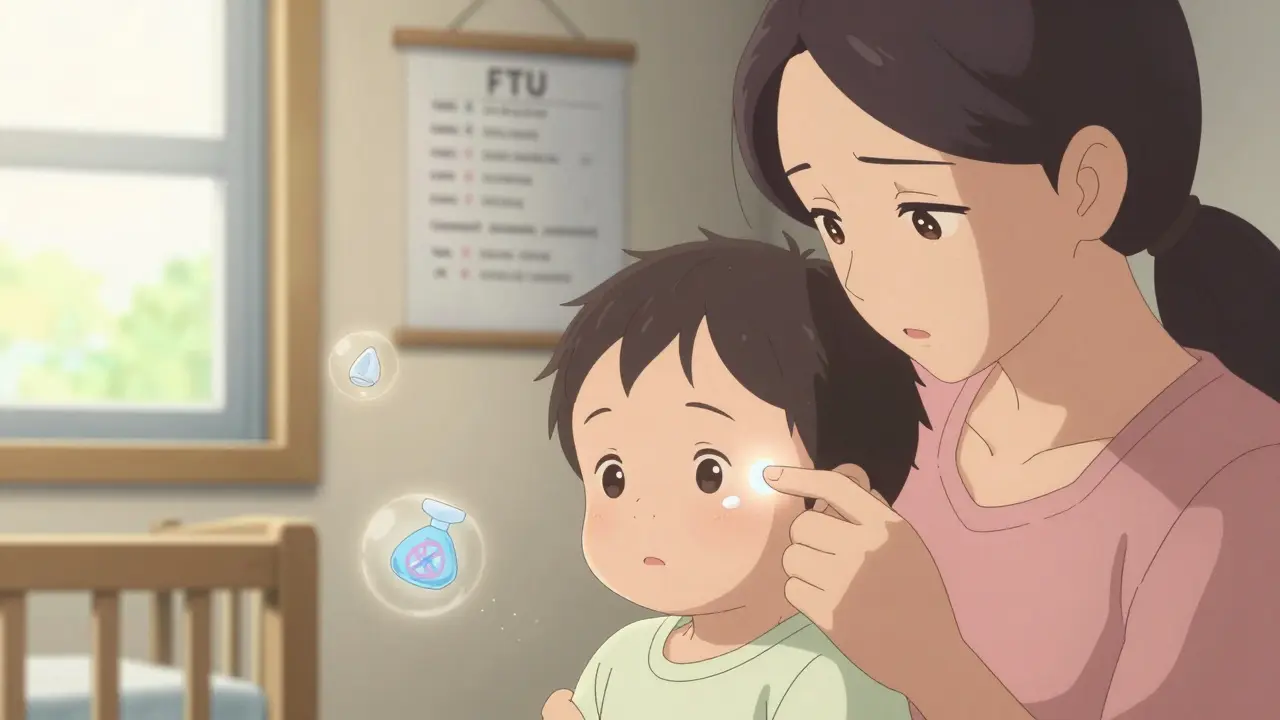
The Fingertip Unit: How Much Is Too Much?
Most parents use the “pea-sized” rule. That’s not accurate. The correct way to measure topical medication is the fingertip unit (FTU). One FTU is the amount of cream or ointment squeezed from a standard tube (5mm diameter) from the first crease to the tip of the index finger. That’s about 0.5 grams.
One FTU covers an area equal to two adult palms. For a child under 10kg (about 22 pounds), the maximum daily dose of a topical corticosteroid should not exceed 2 grams total-that’s four FTUs. Spread across the whole body? That’s dangerous. Even applying it to one leg or one arm can be enough if you use too much.
Here’s a simple guide:
- One full arm: 1 FTU
- One full leg: 2 FTUs
- Face and neck: 0.5 to 1 FTU
- Back: 3 to 4 FTUs
Never apply more than one FTU per area. And never cover it with plastic wrap, Tegaderm, or a tight diaper unless your doctor specifically says to. Occlusion can boost absorption by 300% to 500%. That turns a safe dose into a toxic one.
What to Avoid Completely
Some products have no place in a child’s medicine cabinet. Here’s what to throw out:
- Benzocaine-teething gels, sore throat sprays. No exceptions. The FDA banned these for under-2s for good reason.
- Dibucaine-found in some hemorrhoid creams. Even small amounts can cause toxicity in kids.
- Lidocaine patches or gels-not for routine use. Only under medical supervision for procedures like IV starts.
- High-potency steroids (clobetasol, betamethasone)-never for children under two unless in a hospital setting.
- Antibiotic creams (neomycin, bacitracin)-they cause allergic reactions more often than they help. Plain petroleum jelly works better for minor cuts.
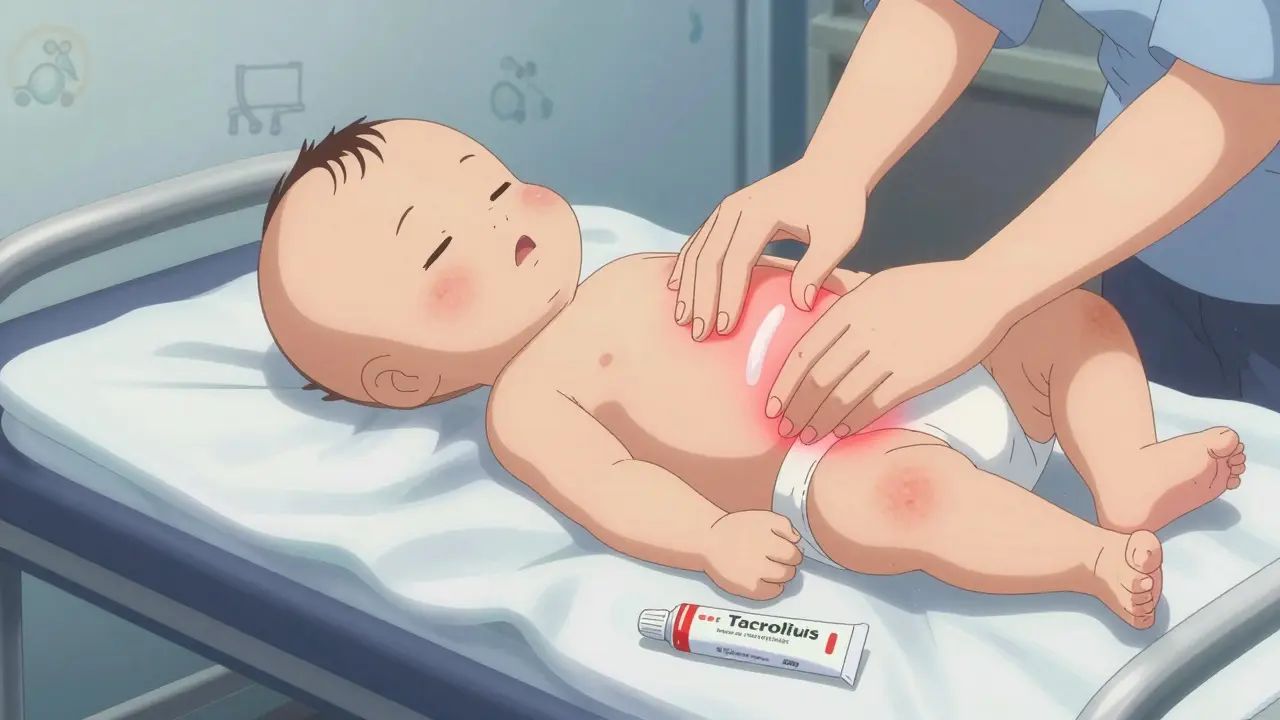
There are safer alternatives. For teething, chilled (not frozen) teething rings work better than any gel. For eczema, topical calcineurin inhibitors like tacrolimus 0.03% or pimecrolimus are approved for infants as young as three months. They don’t thin skin or suppress hormones. Yes, they come with a black box warning about cancer risk-but after 15 years of real-world use, there’s not a single confirmed case linking them to cancer in children.
Storage and Prevention: The Silent Danger
Most accidental poisonings don’t happen because a child broke into a cabinet. They happen because a parent left the tube on the bathroom counter after applying cream. The American Association of Poison Control Centers found that 78% of pediatric topical medication exposures occur when products are left within reach after use.
Always return creams to child-resistant packaging immediately. Even if you’re in a hurry. Even if you think you’ll be back in five minutes. That five minutes is all it takes. The Consumer Product Safety Commission mandated child-resistant packaging for topical anesthetics over 30 years ago-but many over-the-counter products still don’t comply. A 2022 FDA check found 32% of retail lidocaine products still sold in non-child-resistant packaging.
Keep all topical medications locked away. Not just in a cabinet-but out of sight, out of reach. Grandparents, babysitters, and older siblings need to know this rule too. One in five households share topical medications between family members. That’s how a child ends up with a steroid meant for their cousin’s psoriasis.

When to Call for Help
Most topical reactions are mild-redness, itching, irritation. But some are emergencies. Call 911 or go to the ER if your child has:
- Blue or gray skin, especially around the lips or fingertips
- Difficulty breathing or rapid, shallow breathing
- Extreme drowsiness, confusion, or unresponsiveness
- Seizures or muscle twitching
- Swelling of the face, tongue, or throat
These are signs of systemic toxicity. Methemoglobinemia from benzocaine requires immediate treatment with methylene blue. Lidocaine overdose can cause seizures and heart rhythm problems. Don’t wait. Don’t Google it. Call emergency services.
What’s Changing for the Better
There’s progress. The FDA’s 2023 draft guidance now requires all topical medications to include clear pediatric labeling: maximum body surface area, age limits, duration of use. New products are being designed with child-safe dosing systems-think pumps instead of tubes, pre-measured sachets, and QR codes that link to safety videos.
Pharmacies in the UK and US are starting to stock pediatric-specific formulations. The American Academy of Pediatrics now recommends calcineurin inhibitors as first-line for facial eczema in babies over three months. That’s a big shift. Doctors are finally recognizing that low-potency steroids and moisturizers are often all you need.
The future of pediatric skin care isn’t stronger creams-it’s smarter ones. Nanoparticle delivery systems are in late-stage trials. These tiny carriers deliver medication exactly where it’s needed, reducing absorption into the bloodstream by up to 80%. They’re not on shelves yet-but they’re coming.
Bottom Line: Less Is More
Topical medications for children aren’t like adult ones. They’re not safer just because they’re labeled for kids. The safest treatment is often no medication at all. For mild rashes, use fragrance-free moisturizers. For teething, use cold rubber teethers. For eczema, use a gentle cleanser and thick emollient twice a day.
If you need a cream, use the lowest strength possible. Apply the smallest amount needed. Never use it on broken skin. Never cover it. Always store it away. And never, ever use adult products on a child.
Your child’s skin is delicate. Treat it that way.
Can I use hydrocortisone cream on my baby’s face?
Yes, but only if it’s 0.5% or 1% hydrocortisone, and only for a few days at a time. Use no more than half a fingertip unit for the entire face. Avoid daily use for more than a week. For long-term eczema on the face, doctors now recommend topical calcineurin inhibitors like tacrolimus 0.03%-they’re safer and just as effective.
Is it safe to use lidocaine cream before a needle stick?
In controlled medical settings, yes. Hospitals use 4% lidocaine cream for infants during IV placement or blood draws, but only under strict supervision. Apply it 30 to 60 minutes before, cover with a dressing, and use no more than 1.2g total in 24 hours. Never use it at home without a doctor’s instruction. Overuse can cause seizures or heart problems.
What should I do if my child swallows a topical cream?
Call Poison Control immediately at 1-800-222-1222 (US) or 111 (UK). Do not wait for symptoms. Even small amounts of benzocaine, lidocaine, or strong steroids can be dangerous. Keep the product container handy-poison control will need the ingredients and concentration. Do not induce vomiting unless instructed.
Are natural or herbal topical remedies safe for kids?
Not necessarily. Many herbal creams contain hidden ingredients like essential oils, which can be toxic to children. Tea tree oil, eucalyptus, and lavender oils have caused seizures and hormonal disruptions in infants. Even coconut oil or olive oil can worsen eczema in some babies. Always check with your pediatrician before using anything not approved by a doctor.
How do I know if a topical cream is approved for children?
Look for the age range on the label. Prescription creams will list approved ages in the prescribing information. For over-the-counter products, check the Drug Facts panel. If it doesn’t mention children, assume it’s not meant for them. If you’re unsure, ask your pharmacist or pediatrician. Never rely on marketing claims like “gentle for babies”-those aren’t regulated.





11 Comments
Meghan Hammack
January 8, 2026My 14-month-old had a bad eczema flare-up last winter and I nearly panicked when the dermatologist said to use hydrocortisone. I thought I was being reckless-turns out I was just ignorant. This post saved me. One FTU? I had been using like a quarter of the tube. Holy crap. Thank you for the clarity.
Now I keep the cream locked in the bathroom cabinet with the childproof cap on, even if I’m just stepping out for 2 minutes. Worth it.
Also-teething rings in the fridge, not the freezer. Game changer.
RAJAT KD
January 9, 2026Correct. Benzocaine is a silent killer. I saw a 10-month-old in the ER with methemoglobinemia after his grandma applied ‘just a dab’ of Orajel. He turned blue before we could get the methylene blue. No exceptions. No ‘but my cousin used it’ stories. This isn’t folklore-it’s pharmacology.
Jeffrey Hu
January 10, 2026Actually, you’re all missing the bigger point. The FDA’s 2023 draft guidance doesn’t go far enough. They still allow hydrocortisone 1% OTC for infants under 2-completely irresponsible. The American Academy of Pediatrics’ recommendation of calcineurin inhibitors as first-line is a step forward, but we need to ban all topical steroids under age 2 outright. The HPA axis suppression data is overwhelming.
And let’s not forget: occlusion isn’t just dangerous-it’s a form of child endangerment when done without medical oversight. Parents think wrapping a diaper over steroid cream is ‘enhancing absorption’-it’s poisoning.
Also, ‘natural remedies’? Tea tree oil causes gynecomastia in male infants. Lavender oil is an endocrine disruptor. This isn’t ‘holistic healing’-it’s chemical negligence.
Lindsey Wellmann
January 10, 2026OMG I JUST REALIZED I’VE BEEN USING MY COUSIN’S CLOBETASOL ON MY KID’S ECZEMA 😭😭😭
THANK YOU FOR THIS POST I’M DELETING IT RIGHT NOW AND BUYING A LOCKBOX AND A TACROLIMUS TUBE AND I’M GOING TO CRY IN THE BATHROOM FOR 20 MINUTES 😭🙏😭
Also, I used to leave the lidocaine cream on the counter after baths. Like, I’d be like ‘oh I’ll put it back in 5’-but then I’d get distracted by TikTok and-
MY BABY COULD’VE DIED. I’M SO SORRY BABY 😭
tali murah
January 11, 2026Oh, so now we’re pretending this is a parenting guide and not a fearmongering pamphlet from Big Pharma? Let’s be real-most of these ‘toxic’ reactions happen because parents panic and overapply. You don’t need to treat every little red spot like it’s a biohazard.
And ‘never use adult products’? My 3-year-old had a sunburn and I used my leftover hydrocortisone cream. He’s fine. The world didn’t end. Kids are resilient. Not every parent is a negligent idiot.
Also, why is everyone so terrified of steroids? My kid had eczema for 18 months and we used low-dose triamcinolone for 3 weeks. No stretch marks. No adrenal suppression. Just less itching. That’s not a tragedy-it’s medicine.
Jenci Spradlin
January 13, 2026just a heads up-i used to think the fingertip unit was just a myth til i started using it. i was putting on like a whole blob of cream thinking ‘this should cover it’ but then i measured it and holy cow it was like 3x too much.
also-lidocaine patches? nope. nope nope nope. my niece got a seizure from one when her grandma stuck it on her leg for a mosquito bite. she was 18 months. we got lucky she didn’t die.
and yeah, forget the ‘natural’ stuff. my cousin used coconut oil on her baby’s face and it made the eczema worse. like, way worse. like, ‘we had to go to the dermatologist at 2am’ worse.
just use the stuff the doc says. and lock it up.
Ashley Kronenwetter
January 14, 2026Thank you for this comprehensive and clinically accurate guide. As a pediatric nurse, I see the consequences of misinformation daily. The most alarming trend is not misuse-it’s normalization. Parents treat topical steroids like lotion and benzocaine like candy. This isn’t negligence; it’s systemic failure of public health education.
I urge all caregivers to treat pediatric topical medications with the same caution as oral prescriptions. Store them securely. Use only as directed. Never assume ‘it’s just a cream.’
And please, if you’re unsure-ask. Your pediatrician or pharmacist is there for this exact reason.
Aron Veldhuizen
January 16, 2026Let’s talk about the elephant in the room: why are we letting corporations dictate what’s ‘safe’ for children? The FDA bans benzocaine but allows hydrocortisone 1% OTC? That’s not science-it’s lobbying.
And who decided that ‘fingertip unit’ is the gold standard? Who measured it? On what infant skin? This is all anecdotal nonsense dressed up as medicine.
Maybe the real solution is to stop medicating children altogether. Let their skin heal naturally. Let them feel discomfort. That’s how evolution works.
Also-why are we so obsessed with ‘covering’ skin? Skin needs to breathe. Maybe the problem isn’t the cream-it’s our obsession with ‘fixing’ everything.
Chris Kauwe
January 16, 2026As an American, I find it offensive that we’re importing European-style pediatric protocols without understanding our own healthcare realities. In the UK, they have access to specialist dermatologists and pediatric pharmacists. In rural America? Parents are using YouTube videos and Walmart’s ‘baby-safe’ aisle.
Yes, benzocaine is dangerous. But telling a single mom in Mississippi to use tacrolimus instead of hydrocortisone is like telling her to use a Tesla instead of a pickup truck. It’s not practical.
We need scalable, realistic solutions-not elitist guidelines written by Ivy League MDs who’ve never changed a diaper at 3 a.m.
Johanna Baxter
January 18, 2026my baby had a rash and i used the hydrocortisone and then i cried because i thought i was a bad mom and then i used it again and then i cried again and then i locked it away and now i just rub coconut oil on her and pray
why is everything so hard
Matthew Maxwell
January 18, 2026It is deeply irresponsible to suggest that ‘less is more’ when it comes to pediatric dermatological care. This post, while well-intentioned, dangerously underestimates the severity of conditions like atopic dermatitis and the necessity of appropriate medical intervention. To imply that moisturizers alone are sufficient for moderate-to-severe eczema is not only medically unsound-it is a dereliction of duty to vulnerable children.
Parents must be empowered with precise, evidence-based guidance-not vague platitudes about ‘natural healing.’ The HPA axis suppression data is real, yes-but so is the suffering of children with uncontrolled eczema, who scratch until they bleed and cannot sleep.
The solution is not fear. It is education. And the education must come from physicians-not internet bloggers.