MAOI Medication Interaction Checker
When you’ve tried multiple antidepressants and nothing seems to work, the idea of switching to an MAOI might feel like a last resort. But here’s the truth: for some people with severe, treatment-resistant depression, MAOIs are the only thing that brings real relief. The problem? Mixing them with other antidepressants can be deadly if you don’t know what you’re doing. This isn’t theoretical. People have died from serotonin syndrome after combining MAOIs with SSRIs like fluoxetine or sertraline. And yet, many doctors still avoid MAOIs entirely-not because they’re ineffective, but because they’re misunderstood.
What Are MAOIs and Why Do They Still Matter?
MAOIs, or monoamine oxidase inhibitors, were the first antidepressants ever developed. Iproniazid, originally meant for tuberculosis, was found in the 1950s to lift mood in patients. Today, the most common ones are phenelzine (Nardil), tranylcypromine (Parnate), and the transdermal patch selegiline (Emsam). Unlike newer drugs that just block serotonin reuptake, MAOIs stop the enzyme that breaks down serotonin, norepinephrine, and dopamine. That means more of these mood-boosting chemicals stay active in your brain.
They’re not first-line treatments for a reason: they come with serious risks. But for about 20-30% of people with depression that doesn’t respond to SSRIs, SNRIs, or even TCAs, MAOIs work where nothing else does. Studies show response rates of 40-60% in treatment-resistant cases. They’re especially helpful for atypical depression-where you feel heavy, oversleep, crave carbs, and are hypersensitive to rejection. If you’ve been stuck for years, MAOIs might be the key.
The Deadliest Mix: MAOIs and SSRIs/SNRIs
The most dangerous combination is MAOIs with SSRIs (like Prozac, Zoloft) or SNRIs (like Effexor, Cymbalta). Why? Both types increase serotonin. When you combine them, serotonin levels can spike dangerously fast. That’s serotonin syndrome-a medical emergency.
Symptoms include high fever, muscle rigidity, rapid heartbeat, confusion, seizures, and in the worst cases, death. A 1995 study in the Journal of Clinical Psychiatry found that 7 out of 8 fatal cases involved fluoxetine and tranylcypromine. The FDA issued a boxed warning: never combine these. And it’s not just about taking them together. Timing matters just as much.
If you’re switching from an SSRI to an MAOI, you need to wait. For most SSRIs, that’s 14 days. But for fluoxetine? You have to wait five weeks. Why? Fluoxetine and its active metabolite, norfluoxetine, stick around in your body way longer than other SSRIs. Jumping in too soon can kill you.
And it doesn’t work the other way either. If you stop an MAOI and try to start an SSRI too soon, your body hasn’t rebuilt the monoamine oxidase enzymes yet. That’s why you need at least 14 days between stopping an MAOI and starting any SSRI or SNRI.
What About Tricyclic Antidepressants (TCAs)?
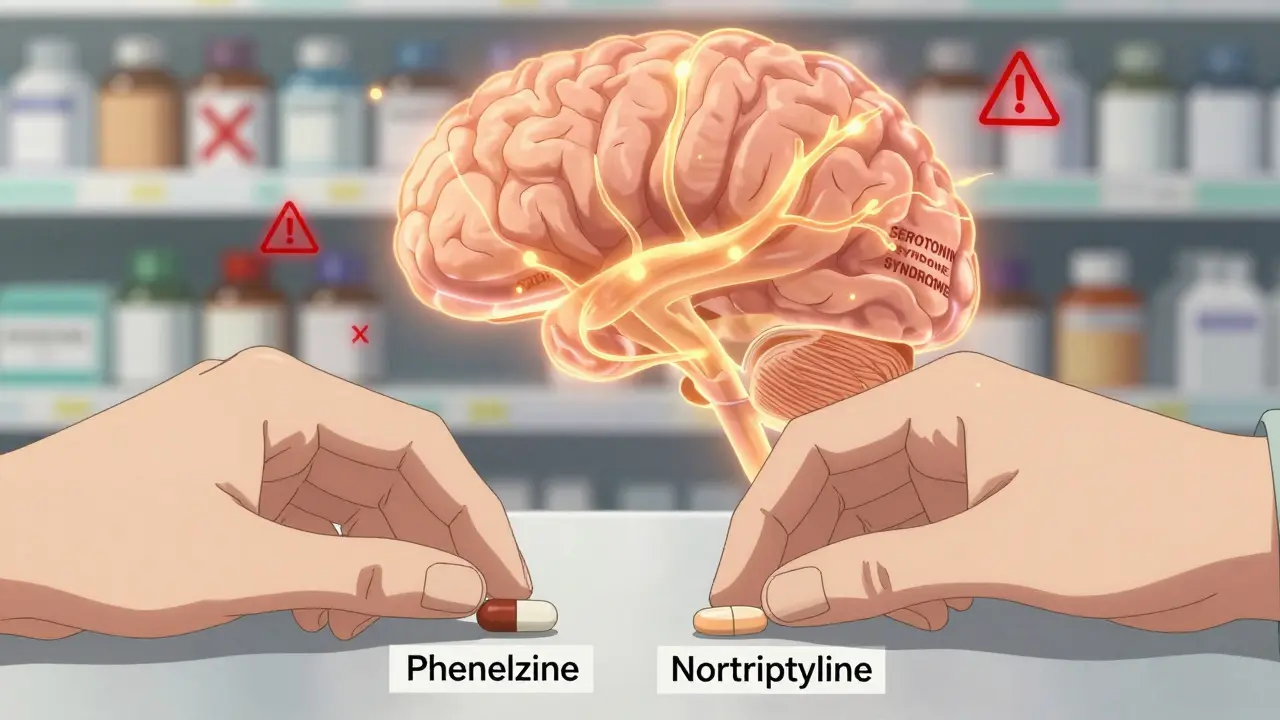
This is where things get messy. For decades, doctors were told to never combine MAOIs with TCAs like amitriptyline or clomipramine. The fear was serotonin syndrome. But recent research is turning that advice on its head.
A 2022 review in PMC9680847 found that combining MAOIs with certain TCAs-especially nortriptyline-can be safe and effective in treatment-resistant cases. In one study, 57% of patients responded to phenelzine plus nortriptyline with minimal side effects. That’s not a fluke. It’s a proven strategy.
But here’s the catch: you can’t just add an MAOI to someone already on a TCA. The order matters. The TCA must be started first-or at the same time. If you give the MAOI first, the risk of adverse reactions skyrockets. And clomipramine? Avoid it entirely. It’s too strong on serotonin reuptake.
So yes, some TCAs can be combined with MAOIs. But only under strict supervision, with slow titration and close monitoring. This isn’t something you do on your own. It’s a specialist-level decision.
Safe Alternatives: What You Can Combine
Not all antidepressants are dangerous with MAOIs. In fact, there are several that are considered safe-and even useful-when used together.
- Bupropion (Wellbutrin): It works on dopamine and norepinephrine, not serotonin. No risk of serotonin syndrome. Many clinicians use it alongside MAOIs to boost energy and motivation.
- Mirtazapine (Remeron): Increases serotonin and norepinephrine through a different mechanism. Multiple case reports show it’s well tolerated with MAOIs, especially for sleep and appetite issues.
- Trazodone: Often used for insomnia, it has minimal serotonin reuptake effects. Safe to combine with MAOIs for sleep problems.
- Nortriptyline: As mentioned, this TCA is the safest option when combined with MAOIs, thanks to its weaker effect on serotonin reuptake.
Some psychiatrists even add dopamine agonists like pramipexole for patients stuck with apathy or anhedonia. These aren’t antidepressants per se, but they help with the emotional flatness that often lingers even when mood improves.
And don’t forget non-antidepressant supports: benzodiazepines for anxiety, or non-benzodiazepine sleep aids like zolpidem. These are generally safe with MAOIs and can make a huge difference in quality of life.
Dietary Risks Are Still Real
Even if you avoid all drug interactions, you can’t ignore food. MAOIs block the enzyme that breaks down tyramine-a compound found in aged cheeses, cured meats, tap beer, soy sauce, and fermented foods. Without that enzyme, tyramine builds up and triggers a dangerous spike in blood pressure.
That’s not a mild headache. That’s a hypertensive crisis: severe headache, chest pain, vomiting, stroke risk. The risk is highest with older MAOIs like phenelzine and tranylcypromine. But even the selegiline patch (Emsam) requires dietary caution at doses above 6mg/24hr. At lower doses, most people don’t need to change their diet.
Here’s what to avoid:
- Aged cheeses (Parmesan, blue cheese, cheddar)
- Tap beer and draft wine
- Salami, pepperoni, and other fermented sausages
- Overripe bananas, soy sauce, and miso
- Home-brewed beer and certain yeast extracts
And remember: you still need to follow these restrictions for two weeks after stopping an MAOI. Your body needs time to rebuild the enzyme.

Stopping MAOIs Isn’t Simple
Don’t just quit. Abruptly stopping an MAOI can cause a withdrawal syndrome that feels like the flu on steroids. Symptoms include restlessness (62% of cases), upset stomach (48%), tingling or burning skin (37%), flu-like symptoms (55%), sleep problems (71%), and headaches (68%).
Always taper slowly-over 2 to 4 weeks. Your doctor should guide you through this. There’s no one-size-fits-all plan, but most people reduce by 10-25% every 5-7 days.
Why Aren’t More Doctors Prescribing MAOIs?
Here’s the sad part: most psychiatrists don’t feel trained to use them. A 2019 study found only 32% of psychiatry residents felt confident managing MAOIs. That’s not because they’re too complex-it’s because they’re rarely taught. Medical schools barely cover them. Pharmacies don’t stock them. Patients are scared off by the warnings.
But for the 15-20% of people with truly refractory depression, MAOIs are the most effective tool we have. The key isn’t avoiding them-it’s using them right. With proper timing, careful combinations, and strict dietary rules, they can change lives.
What’s Next for MAOIs?
Research is moving forward. Newer MAO-B selective inhibitors are being tested to reduce side effects. Some clinics are even exploring combinations with ketamine for rapid relief in treatment-resistant cases. The future isn’t about replacing MAOIs-it’s about making them safer and more accessible.
For now, if you’re struggling after multiple antidepressants, ask your doctor about MAOIs. Not as a last resort-but as a legitimate, evidence-backed option. Just make sure you’re under the care of someone who knows how to use them.
Can I take SSRIs after stopping an MAOI?
Yes, but you must wait at least 14 days after stopping the MAOI before starting an SSRI. If the MAOI you took was fluoxetine (Prozac), you need to wait five weeks because it stays in your system much longer than other SSRIs. Rushing this can cause serotonin syndrome, which can be fatal.
Is it safe to combine MAOIs with bupropion?
Yes, bupropion is one of the safest antidepressants to combine with MAOIs. Unlike SSRIs or SNRIs, it doesn’t significantly affect serotonin reuptake-it works on dopamine and norepinephrine. Many clinicians use this combination to treat fatigue and lack of motivation in treatment-resistant depression.
Why is nortriptyline considered safer than other TCAs with MAOIs?
Nortriptyline has weaker serotonin reuptake inhibition compared to other TCAs like clomipramine or amitriptyline. This means it’s less likely to cause serotonin overload when combined with an MAOI. Studies show it can be used safely in combination with phenelzine under careful monitoring, with high response rates and low side effects.
Do I need to avoid all cheese if I’m on an MAOI?
You need to avoid aged, fermented, or strongly cured cheeses like Parmesan, blue cheese, cheddar, and Swiss. Fresh cheeses like mozzarella, cottage cheese, and cream cheese are generally safe. The risk comes from tyramine, which builds up in aged foods. Always check labels and ask your pharmacist if you’re unsure.
Can I drink alcohol while on an MAOI?
It’s best to avoid alcohol entirely. Alcohol can interact unpredictably with MAOIs, increasing drowsiness, dizziness, and the risk of high blood pressure. Tap beer is especially dangerous due to tyramine content. Even moderate drinking can trigger side effects. If you must drink, talk to your doctor first-some people can tolerate small amounts of wine, but never beer or spirits.
How long does it take for MAOIs to start working?
Most people start noticing improvements in mood and energy after 2 to 4 weeks, but full effects can take 6 to 8 weeks. This is similar to other antidepressants, but because MAOIs are often used in treatment-resistant cases, patience is critical. Don’t stop just because you don’t feel better right away.


11 Comments
Chiraghuddin Qureshi
January 22, 2026MAOIs saved my life after 8 years of SSRIs failing me 😭 But man, the diet? I miss cheese so bad… now I just eat fresh mozzarella and pretend it’s gourmet. Also, bupropion + phenelzine = my new best friends 🙌
Kenji Gaerlan
January 23, 2026so like… uhhh… MAOIs? i thought those were like, old school? why are ppl still using them? also i ate blue cheese yesterday and im fine?? maybe its all hype??
Oren Prettyman
January 25, 2026It is, indeed, a matter of considerable scientific and clinical importance that monoamine oxidase inhibitors-despite their demonstrated efficacy in treatment-resistant depressive disorders-remain underutilized due to a combination of inadequate medical education, pharmacological misinformation, and an overly cautious regulatory environment that prioritizes liability over therapeutic innovation. The historical stigma attached to dietary restrictions and potential drug interactions, while not without basis, has been exaggerated to the point of medical malpractice in certain cases, particularly when patients are left without viable alternatives after exhausting multiple first-line pharmacotherapies.
Liberty C
January 25, 2026Of course the only people who benefit from MAOIs are those who’ve spent a decade bouncing between SSRIs like a broken pinball machine. Meanwhile, the rest of us just… live? Maybe if you didn’t treat depression like a chemical equation you’d realize some people just need therapy, sunlight, and a damn life. But no-let’s keep prescribing nuclear options because convenience trumps wisdom.
Daphne Mallari - Tolentino
January 27, 2026While the article presents a compelling case for the reconsideration of MAOI usage in refractory depression, one must not overlook the ethical imperative of informed consent. The potential for fatal serotonin syndrome, coupled with stringent dietary limitations and the necessity for lifelong pharmacological vigilance, renders the risk-benefit ratio highly contingent upon patient compliance, access to specialist care, and socioeconomic stability. In a healthcare system where these conditions are frequently unmet, the promotion of MAOIs as a legitimate alternative may constitute a form of therapeutic paternalism.
Neil Ellis
January 28, 2026Hey-I’ve been on phenelzine for three years now. No blue cheese, no beer, no drama. But I finally slept through the night for the first time since I was 22. Bupropion was the cherry on top. I know it’s not ‘cool’ to say this, but… MAOIs didn’t just help me. They gave me back my life. If you’re tired of feeling numb, don’t give up. Find a doctor who knows what they’re doing. You’re worth the effort.
Lana Kabulova
January 29, 2026Wait-so you’re saying you can combine MAOIs with nortriptyline? But not clomipramine? And you have to start the TCA first? And fluoxetine stays in your system for five weeks? And you still need to avoid soy sauce? And you can’t just stop cold turkey? And you need to wait two weeks after stopping the MAOI to start anything else? And you need a psychiatrist who actually knows this? And this isn’t taught in med school? I’m just… wow. I’m just… wow.
Rob Sims
January 29, 2026Oh wow. So the answer to ‘I tried everything and nothing worked’ is… a drug that requires a PhD in pharmacology to use safely, a diet that turns you into a sad salad-eating monk, and a 5-week waiting period just to switch meds? Congrats. You’ve turned depression into a full-time job. Next up: mandatory MAOI certification and a loyalty card for fresh mozzarella.
Tatiana Bandurina
January 30, 2026They’re not ‘misunderstood.’ They’re dangerous. People die from this. The fact that you’re casually listing combinations like a recipe book is terrifying. I’ve seen patients go into serotonin syndrome because they ‘read it on Reddit.’ This isn’t biohacking. This is playing Russian roulette with your brainstem.
Akriti Jain
January 30, 2026MAOIs? Funny… I wonder if Big Pharma is okay with this? They made billions off SSRIs. Now they want you to go back to the 50s? And suddenly it’s ‘safe’ if you do it just right? 🤔 Maybe the real cure is not drugs at all… maybe it’s not being born into a system that treats sadness like a glitch to be patched?
🌍💊Hilary Miller
February 1, 2026MAOIs work. Period.